Leprosy (Hansen’s Disease)
Comprehensive Community Health Nursing Notes
Introduction to Hansen’s Disease (Leprosy)
Hansen’s disease, commonly known as leprosy, is a chronic infectious disease caused by Mycobacterium leprae, an acid-fast bacillus. It primarily affects the peripheral nerves, skin, upper respiratory tract, and eyes. Despite being one of the oldest documented diseases in human history, Hansen’s disease continues to be a public health concern in several countries worldwide.
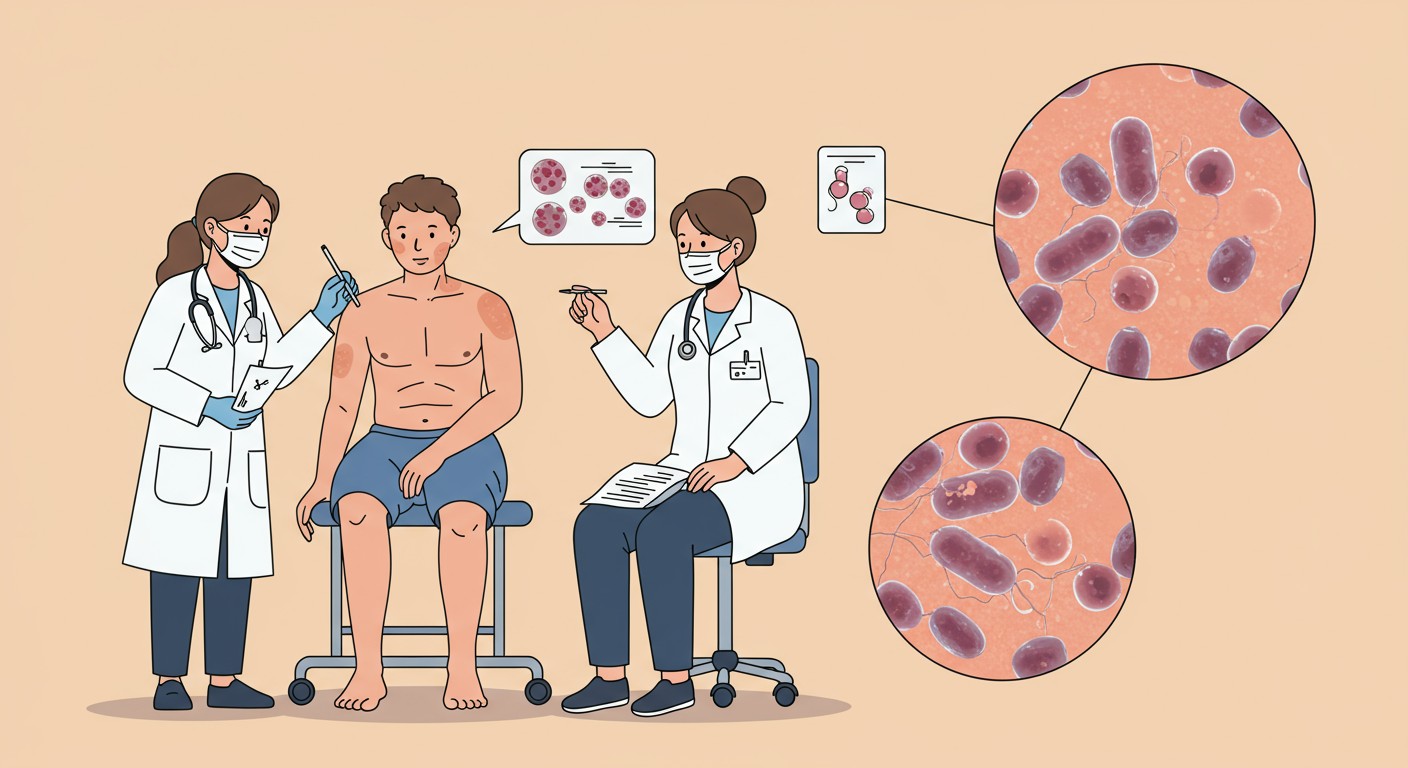
Figure 1: Clinical examination of a patient with Hansen’s disease, showing sensory testing and microscopic view of M. leprae
Clinical Pearl:
Hansen’s disease is one of the least contagious infectious diseases. Approximately 95% of the world’s population has natural immunity to M. leprae infection. Transmission typically requires prolonged close contact with untreated individuals with high bacterial loads.
Epidemiology of Hansen’s Disease
Global Burden
Hansen’s disease remains endemic in over 120 countries. According to the World Health Organization (WHO), approximately 200,000 new cases are reported annually worldwide. The global prevalence has significantly decreased from over 5 million cases in the 1980s to less than 129,192 cases by 2020.
Key Epidemiological Statistics (2023)
- New cases reported globally: 182,815
- Female cases: 72,845 (39.8% of total)
- Child cases: Approximately 10,000 (5.5% of total)
- Current prevalence rate: 0.34 per 10,000 population
Geographical Distribution
Hansen’s disease is most prevalent in tropical and subtropical regions with limited access to healthcare. The highest burden is observed in:
| Region | Key Endemic Countries | Percentage of Global Burden |
|---|---|---|
| South-East Asia | India, Indonesia, Bangladesh | ~70% |
| Americas | Brazil, Mexico | ~15% |
| Africa | Nigeria, Ethiopia, DR Congo | ~10% |
| Western Pacific | Philippines, Papua New Guinea | ~5% |
Transmission
Hansen’s disease is primarily transmitted via respiratory droplets during close and prolonged contact with untreated individuals who have high bacterial loads. The main factors influencing transmission include:
- Duration and closeness of contact with untreated cases
- Socioeconomic factors (overcrowding, poor hygiene)
- Host immunologic status
- Environmental conditions (humidity, temperature)
Community Health Insight:
Despite common misconceptions, casual contact with a person with Hansen’s disease does not lead to transmission. Approximately 95% of people have natural immunity. Household contacts of untreated multibacillary cases are at highest risk (5-10 times higher than the general population).
Pathophysiology
Hansen’s disease is caused by Mycobacterium leprae, an obligate intracellular acid-fast bacillus with unique characteristics:
- Extremely slow growth (doubling time: 12-14 days)
- Cannot be cultured on artificial media
- Optimal growth temperature (30-33°C), preferring cooler body areas
- Primarily affects Schwann cells of peripheral nerves
Immunological Spectrum
The clinical manifestations of Hansen’s disease depend on the host’s immune response to M. leprae. This creates a spectrum of disease presentations classified according to the Ridley-Jopling classification:
| Type | Immune Response | Bacterial Load | Clinical Features |
|---|---|---|---|
| Tuberculoid (TT) | Strong cell-mediated | Low (paucibacillary) | Few well-defined lesions, early nerve damage |
| Borderline Tuberculoid (BT) | Strong but less stable | Low | Several asymmetric lesions |
| Mid-Borderline (BB) | Unstable | Intermediate | Numerous asymmetric lesions |
| Borderline Lepromatous (BL) | Poor | High | Many lesions, moderate symmetry |
| Lepromatous (LL) | Very poor | Very high (multibacillary) | Numerous symmetric lesions, diffuse infiltration |
Mnemonic: “HELP” for Lepromatous vs. Tuberculoid Features
- High bacterial load vs. Low bacterial load
- Extensive, multiple lesions vs. Few, limited lesions
- Lymphocyte response weak vs. strong
- Progressive, symmetric disease vs. asymmetric, localized disease
Clinical Manifestations
Hansen’s disease primarily affects the skin, peripheral nerves, upper respiratory tract mucosa, and eyes. The incubation period ranges from 2-20 years (average 5-7 years).
Cardinal Signs
For community health nursing, remember the three cardinal signs of Hansen’s disease:
- Hypopigmented or reddish skin lesions with loss of sensation
- Thickened or enlarged peripheral nerves
- Presence of acid-fast bacilli in skin smears/biopsies
Common Clinical Features by System
Skin Manifestations
- Hypopigmented or erythematous macules/patches
- Nodules or papules (in lepromatous form)
- Infiltrated plaques
- Smooth, shiny, hairless skin
- Loss of sweating in affected areas
- Leonine facies (in advanced lepromatous leprosy)
Neurological Manifestations
- Sensory loss (touch, temperature, pain)
- Motor weakness in hands, feet, face
- Peripheral nerve thickening (ulnar, peroneal nerves)
- Muscle wasting (especially in hands)
- Claw hand deformity
- Foot drop
Ocular Manifestations
- Lagophthalmos (inability to close eyelids)
- Corneal ulceration
- Decreased corneal sensation
- Iridocyclitis
- Cataract
- Progressive blindness
Other Manifestations
- Nasal congestion and epistaxis
- Loss of eyebrows/eyelashes (madarosis)
- Gynecomastia in males
- Testicular atrophy
- Trophic ulcers on pressure points
- Bone changes (absorption)
Mnemonic: “HANSEN” for Clinical Features
- Hypopigmented patches with sensory loss
- Asymmetry of lesions (tuberculoid form)
- Nerve thickening and damage
- Skin infiltration and nodules
- Eyeliashes and eyebrows lost (madarosis)
- Numbness and motor weakness
Prevention & Control Measures
Prevention and control of Hansen’s disease involve multiple strategies aimed at reducing transmission, early case detection, and preventing disabilities.
Primary Prevention
Contact Tracing & Chemoprophylaxis
- Identify household, neighborhood, and social contacts
- Administer single-dose rifampicin (SDR) as post-exposure prophylaxis
- SDR reduces risk of developing Hansen’s disease by ~60%
- Priority for contacts of multibacillary cases
- Regular follow-up examinations for at least 5 years
BCG Vaccination
- Bacillus Calmette-Guérin (BCG) vaccine offers ~26% protection
- Higher efficacy against more severe forms
- Revaccination may provide additional protection
- Part of routine immunization in endemic countries
- Recommended for household contacts
Community-Based Prevention Strategies
| Strategy | Activities | Nursing Role |
|---|---|---|
| Health Education |
|
Develop culturally appropriate educational materials, conduct group sessions, engage community leaders |
| Active Case Finding |
|
Perform skin examinations, identify suspected cases, coordinate referrals, train community health workers |
| Contact Management |
|
Maintain contact registry, conduct home visits, administer prophylaxis, educate about early signs |
| Socioeconomic Measures |
|
Coordinate with social services, advocate for improved living conditions, assist with support group formation |
Community Health Pearl:
Early detection and prompt initiation of multidrug therapy (MDT) is the most effective way to prevent Hansen’s disease transmission. After starting treatment, patients rapidly become non-infectious, usually within 72 hours. This makes early case finding a cornerstone of public health control strategies.
Disability Prevention
Prevention of disabilities is a critical component of Hansen’s disease control programs:
Self-Care Education
- Daily self-inspection of hands and feet
- Proper wound care techniques
- Use of protective footwear
- Regular moisturizing of dry skin
- Eye care practices
Early Intervention
- Prompt treatment of neuritis
- Corticosteroid therapy for reactions
- Splinting for hands/feet
- Physical therapy exercises
- Management of eye complications
Rehabilitation
- Assistive devices provision
- Reconstructive surgery
- Vocational training
- Psychosocial support
- Community integration
Screening & Diagnosis
Community Screening Approaches
Early detection through systematic screening is critical to controlling Hansen’s disease. Community health nurses play a pivotal role in implementing effective screening programs.
Priority Groups for Screening
- Household contacts of known cases
- Neighborhood/social contacts
- Residents of endemic areas
- Individuals with suspicious skin lesions
- Persons with unexplained peripheral neuropathy
- Children in endemic areas
- Healthcare workers in high-burden settings
- Migrants from endemic countries
Diagnostic Approaches
The diagnosis of Hansen’s disease relies on clinical examination supported by laboratory tests when available.
| Diagnostic Method | Description | Nursing Considerations |
|---|---|---|
| Clinical Examination |
|
Ensure proper lighting, maintain privacy, examine the entire body including cooler areas, explain procedures to reduce anxiety |
| Slit Skin Smear |
|
Assist with proper specimen collection, ensure aseptic technique, provide emotional support, prepare patient for minor discomfort |
| Skin or Nerve Biopsy |
|
Explain procedure, obtain informed consent, assist during biopsy, provide post-procedure care, ensure proper specimen handling |
| PCR Testing |
|
Educate about test purpose, coordinate with reference laboratories, ensure proper specimen collection and transport |
Mnemonic: “DETECT” for Clinical Screening
- Discolored skin patches (hypopigmented or reddish)
- Examine sensation (test for touch, pain, temperature)
- Thickened nerves (ulnar, median, radial, peroneal)
- Eyelid problems (inability to close fully)
- Claw hand or foot drop (motor involvement)
- Trophic ulcers (painless wounds on pressure points)
Practical Field Techniques
Sensory Testing Procedure for Community Health Nurses
- Prepare the patient: Explain the procedure and demonstrate on a normal area first.
- Test tools: Use monofilaments, cotton wool, toothpicks, or warm/cold water tubes.
- Testing method: Ask the patient to close their eyes. Apply the stimulus and ask them to point to where they feel it.
- Systematic approach: Test both affected areas and corresponding unaffected areas for comparison.
- Documentation: Mark anesthetic areas on a body chart using standardized symbols.
WHO Operational Classification
For treatment purposes, the WHO classifies Hansen’s disease into two groups:
Paucibacillary (PB) Leprosy
- 1-5 skin lesions
- No bacilli on skin smear (if available)
- Corresponds to TT and BT forms
- Limited nerve involvement
- Less infectious
Multibacillary (MB) Leprosy
- More than 5 skin lesions
- Positive skin smear (if available)
- Corresponds to BB, BL, and LL forms
- More extensive nerve involvement
- More infectious
Field Tip:
In resource-limited settings where skin smears are unavailable, community health nurses should apply the principle: “When in doubt, treat as MB.” This ensures adequate treatment coverage even without laboratory confirmation.
Primary Management
Hansen’s disease is a curable condition with WHO-recommended multidrug therapy (MDT). Community health nurses play a crucial role in treatment administration, monitoring, and support.
Multidrug Therapy (MDT)
| Classification | Drug Regimen | Duration | Nursing Management |
|---|---|---|---|
| Paucibacillary (PB) |
|
6 months | Monitor monthly, ensure medication adherence, assess for drug reactions, document progress, educate about expected skin changes |
| Multibacillary (MB) |
|
12 months | Monitor monthly, counsel about skin pigmentation changes from clofazimine, assess for drug reactions, screen for complications, reinforce adherence |
| Children (ages 10-14) |
|
Same as adults | Ensure weight-appropriate dosing, involve parents/guardians in treatment monitoring, assess growth and development, provide age-appropriate education |
Clinical Pearl:
Patients become non-infectious within 72 hours of starting MDT. There is no need for isolation once treatment begins. However, completion of the full course is essential to prevent relapse and drug resistance.
Management of Reactions and Complications
Hansen’s disease reactions are immunological episodes that can occur before, during, or after MDT. They can cause severe nerve damage if not properly managed.
Type 1 Reaction (Reversal Reaction)
- Symptoms: Increased inflammation in existing lesions, new lesions, edema, nerve pain/tenderness
- Treatment: Prednisone/prednisolone 40-60mg daily with gradual tapering over 3-6 months
- Nursing care: Assess nerve function regularly, monitor for steroid side effects, provide pain management
Type 2 Reaction (Erythema Nodosum Leprosum)
- Symptoms: Painful nodules, fever, joint pain, iritis, neuritis, orchitis
- Treatment: Prednisone/prednisolone, thalidomide (with strict precautions), clofazimine
- Nursing care: Monitor vital signs, provide antipyretics, assess for systemic involvement, ensure contraception for women on thalidomide
Mnemonic: “REACT” for Leprosy Reactions
- Recognize early signs (new inflammation, pain, tenderness)
- Evaluate nerve function systematically
- Act quickly with appropriate medication
- Continue MDT during reactions
- Track progress with regular assessments
Nursing Care for Hansen’s Disease Patients
Physical Care
- Wound and ulcer management
- Eye care and protection
- Prevention of traumatic injuries
- Range of motion exercises
- Adaptive equipment provision
- Skin and nail care education
Medication Management
- MDT administration and monitoring
- Pill counts and adherence strategies
- Side effect assessment and management
- Medication education
- Blister pack preparation
- Treatment calendar implementation
Psychosocial Support
- Stigma reduction counseling
- Self-image support
- Family education and involvement
- Support group facilitation
- Community reintegration assistance
- Vocational rehabilitation referrals
Referral Criteria
Community health nurses should recognize situations requiring referral to specialized care. Timely referral is essential for preventing complications and disabilities.
Immediate Referral Indicators
- New nerve function impairment
- Severe leprosy reactions
- Eye involvement (red eye, vision changes)
- Complicated ulcers or infections
- Severe adverse drug reactions
- Pregnancy in patients on MDT
- Signs of relapse after treatment
- Psychological distress or depression
Referral Pathway
| Level of Care | Services Provided | When to Refer |
|---|---|---|
| Primary Health Center |
|
Refer to district hospital if diagnosis is uncertain, complications develop, or specialized care is needed |
| District Hospital |
|
Refer to referral center for severe reactions, nerve function impairment, eye complications, or need for surgery |
| Referral Center/Specialized Hospital |
|
After specialized care, patients return to primary/district level with clear follow-up instructions |
Information to Include in Referrals
- Patient demographics and contact information
- Date of diagnosis and classification (PB/MB)
- MDT start date and doses completed
- Previous reactions and treatments
- Current symptoms and their duration
- Baseline and current nerve function assessments
- Other medical conditions and medications
- Social circumstances affecting care
Community Health Insight:
Establish referral networks before they are needed. Community health nurses should maintain an updated contact list of Hansen’s disease specialists, rehabilitation centers, and supportive services. Pre-established relationships with these providers improve the quality and timeliness of referrals.
Follow-Up Care
Systematic follow-up is essential for ensuring treatment completion, early detection of complications, and preventing disabilities in Hansen’s disease.
Follow-Up Schedule
| Time Period | Activities | Nursing Responsibilities |
|---|---|---|
| During Treatment |
|
Administer supervised doses, conduct physical assessments, provide health education, document progress, address side effects |
| First Year Post-Treatment |
|
Conduct follow-up examinations, reinforce self-care techniques, assess for late reactions, update rehabilitation plan |
| Second Year Onward |
|
Perform biannual checkups, screen for signs of relapse, evaluate disability status, reinforce self-care, address social integration |
Key Follow-Up Assessment Parameters
Clinical Monitoring
- Skin lesion activity (erythema, infiltration)
- New lesion development
- Nerve function (sensory and motor)
- Reaction signs and symptoms
- Eye examination
- Wound and ulcer assessment
- Signs of relapse (new lesions after treatment)
Functional & Psychosocial Assessment
- Activities of daily living performance
- Self-care practices adherence
- Assistive device utilization
- Vocational activities
- Family and community integration
- Mental health status
- Quality of life measures
Relapse Detection and Management
Signs of Potential Relapse
- New skin lesions appearing after treatment completion
- Reactivation or increased activity in old lesions
- New nerve involvement or function loss
- Positive skin smear in previously negative cases
Management Steps
- Confirm diagnosis with skin smear/biopsy when available
- Differentiate from late reactions (may require specialist assessment)
- Reinitiate appropriate MDT regimen (usually as MB)
- Consider drug resistance testing if available
- Intensify follow-up frequency
Follow-Up Strategy:
Implement a “No Lost to Follow-Up” approach using community health workers and mobile outreach to maintain contact with Hansen’s disease patients. Mobile phone reminders, peer support groups, and integrated follow-up with other health services can improve long-term monitoring adherence.
Global Best Practices
Several countries have developed innovative approaches to Hansen’s disease control and management that can be adapted to various settings.
India: ASHA Program Integration
India has successfully integrated Hansen’s disease detection and care into their Accredited Social Health Activist (ASHA) program, creating a sustainable community-based surveillance system.
Key Elements:
- ASHAs trained in early case detection
- Performance-based incentives for case finding
- House-to-house active case detection campaigns
- Treatment adherence monitoring at community level
- Integration with other NTD control programs
Brazil: Post-Exposure Prophylaxis
Brazil has pioneered large-scale implementation of post-exposure prophylaxis (PEP) using single-dose rifampicin (SDR-PEP) for contacts of Hansen’s disease patients.
Key Elements:
- Systematic contact tracing protocols
- Expanded definition of “contacts” beyond household
- Electronic registry systems for contact follow-up
- Integration of PEP with routine primary care
- Regular effectiveness monitoring with research partnerships
Philippines: Integrated Skin NTD Approach
The Philippines has implemented an integrated approach to skin-related Neglected Tropical Diseases (NTDs), combining surveillance and management of Hansen’s disease with other conditions.
Key Elements:
- Integrated skin clinics at primary health centers
- Common training modules for healthcare workers
- Mobile teledermatology for remote diagnosis
- Shared logistics and supply chains
- Combined community education campaigns
Ethiopia: Self-Care Groups
Ethiopia has developed a successful model of self-care groups for Hansen’s disease patients with disabilities, focusing on peer support and economic empowerment.
Key Elements:
- Peer-led support groups meeting regularly
- Shared savings and microfinance initiatives
- Group-based wound care and self-monitoring
- Collective advocacy to reduce stigma
- Income-generating activities and vocational training
Adaptable Best Practices for Community Health Nursing
- Community Health Worker Mobilization: Train local health volunteers in basic screening and follow-up procedures for Hansen’s disease.
- Integrated Service Delivery: Combine Hansen’s disease surveillance with other community outreach activities to maximize resources.
- Digital Health Solutions: Implement simple mobile applications for case reporting, treatment monitoring, and follow-up reminders.
- School-Based Screening: Train teachers to identify suspicious skin lesions and refer children for evaluation.
- Stigma Reduction Campaigns: Develop locally appropriate communication materials highlighting curability and challenging myths.
- Patient Champions: Engage successfully treated individuals as advocates and educators in community awareness activities.
Resources for Community Health Nurses
Clinical Resources
Mobile Applications & Tools
LepApp
Mobile application for healthcare workers with diagnosis algorithms and treatment guidelines.
NLR SkinApp
Differential diagnosis tool for skin NTDs including Hansen’s disease with clinical images.
WHO Leprosy Learning Guide
Interactive learning modules for healthcare workers in endemic settings.
