Low Birth Weight and Kangaroo Mother Care: Comprehensive Nursing Guide
A detailed resource for nursing students and healthcare professionals
Table of Contents
- 1. Introduction
- 2. Low Birth Weight: Definition and Classification
- 3. Pathophysiology of Low Birth Weight
- 4. Risk Factors and Causes
- 5. Assessment of Low Birth Weight Infants
- 6. Complications of Low Birth Weight
- 7. Kangaroo Mother Care: Introduction and History
- 8. Components of Kangaroo Mother Care
- 9. Implementation of Kangaroo Mother Care
- 10. Benefits of Kangaroo Mother Care
- 11. Nursing Interventions for Low Birth Weight Infants
- 12. Challenges in Implementing Kangaroo Mother Care
- 13. Mnemonics for Nursing Students
- 14. Global Best Practices
- 15. Case Studies
- 16. Conclusion
- 17. References
Introduction
Low birth weight (LBW) remains a significant global health concern, affecting approximately 15% of births worldwide. As a leading cause of neonatal mortality and morbidity, understanding and managing LBW infants is crucial for nursing professionals. This comprehensive guide focuses on evidence-based approaches to caring for LBW infants, with special emphasis on Kangaroo Mother Care (KMC) – a cost-effective, accessible intervention that has revolutionized the care of preterm and low birth weight infants.
Kangaroo care emerged in the 1970s in Bogotá, Colombia, as a response to overcrowded nurseries, insufficient incubators, and high infection rates. Today, it has evolved into a standardized method endorsed by the World Health Organization (WHO) and has been implemented globally with remarkable success in improving outcomes for vulnerable neonates.
Key Facts
- An estimated 20 million low birth weight babies are born each year, representing 15-20% of all births worldwide.
- 96.5% of low birth weight births occur in developing countries.
- Low birth weight contributes to 60-80% of all neonatal deaths.
- Kangaroo care has been shown to reduce mortality among LBW infants by up to 40% when implemented correctly.
This guide aims to provide nursing students with comprehensive knowledge about LBW infants and the implementation of kangaroo care as an evidence-based intervention. By understanding the principles, benefits, and techniques of KMC, nurses can play a pivotal role in improving outcomes for this vulnerable population.
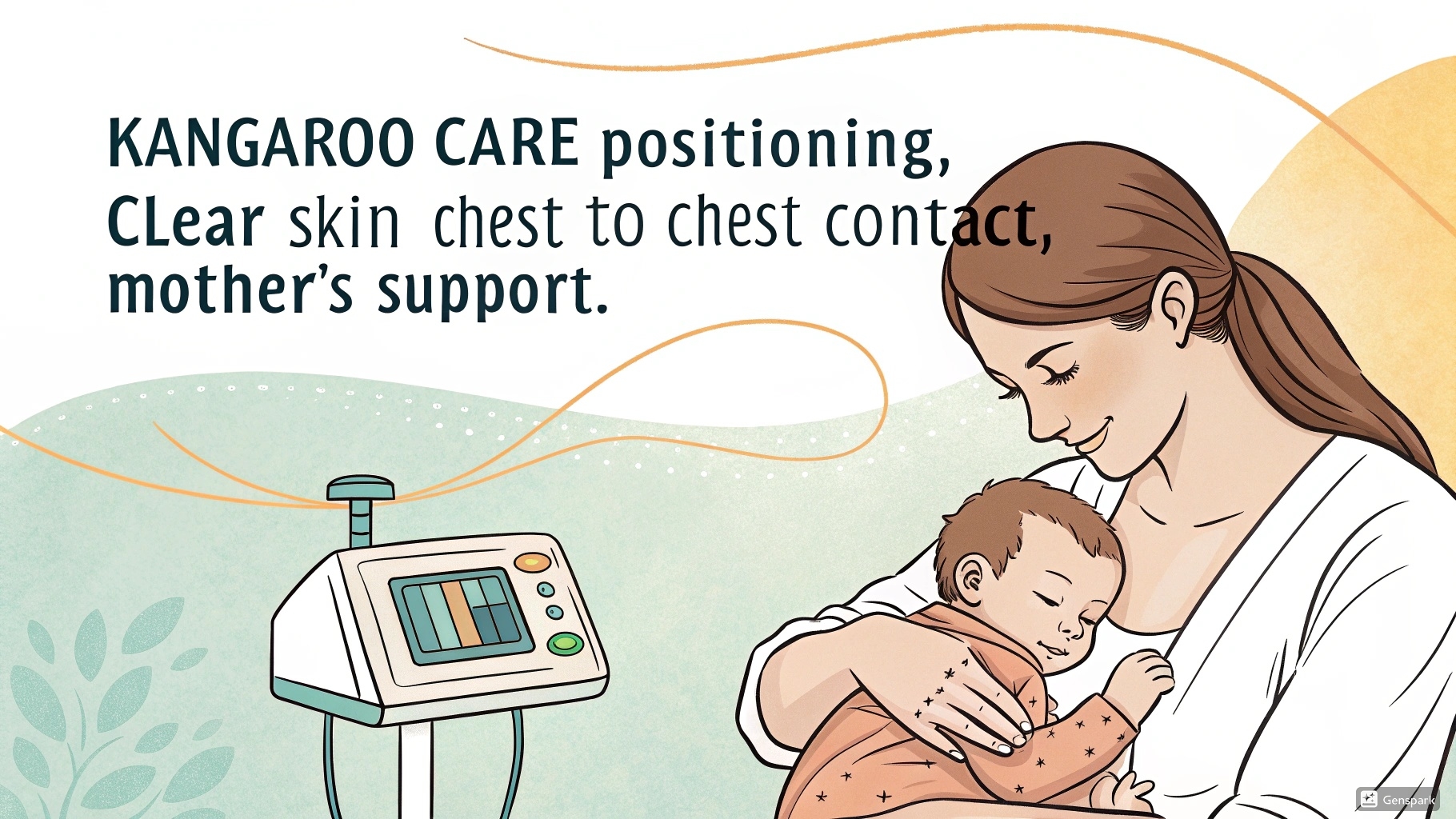
Figure 1: Proper positioning for Kangaroo Mother Care showing skin-to-skin contact with labeled key elements
Low Birth Weight: Definition and Classification
Low birth weight (LBW) refers to a birth weight of less than 2,500 grams (5 pounds 8 ounces), regardless of gestational age. This classification is essential for identifying infants at increased risk of complications and mortality, and for determining appropriate interventions, including kangaroo care.
| Classification | Birth Weight | Risk Level | Common Characteristics |
|---|---|---|---|
| Low Birth Weight (LBW) | < 2,500 grams | Moderate | Increased risk of hypothermia, hypoglycemia, feeding difficulties |
| Very Low Birth Weight (VLBW) | < 1,500 grams | High | Higher risk of RDS, IVH, NEC, and long-term neurodevelopmental issues |
| Extremely Low Birth Weight (ELBW) | < 1,000 grams | Very High | Severe risk of mortality, ROP, BPD, metabolic disturbances |
Categories of Low Birth Weight Based on Causative Factors
Preterm LBW
Infants born before 37 completed weeks of gestation with a weight < 2,500g. This accounts for approximately 2/3 of all LBW cases.
Small for Gestational Age (SGA)
Infants whose birth weight falls below the 10th percentile for gestational age. These infants may be term or preterm but have experienced intrauterine growth restriction (IUGR).
Term LBW
Infants born at term (≥37 weeks) but weighing < 2,500g. These infants have experienced significant IUGR and may have different physiological challenges.
Understanding the classification of LBW is crucial for nurses to implement appropriate interventions, including kangaroo care, which must be adapted based on the infant’s specific category, weight, and health status.
Pathophysiology of Low Birth Weight
The pathophysiology of low birth weight is complex and multifaceted, involving various maternal, placental, and fetal factors. Understanding these mechanisms is essential for nurses to comprehend the challenges faced by LBW infants and the rationale behind interventions like kangaroo care.
Physiological Immaturity in Low Birth Weight Infants
Respiratory System
- Immature lung development with decreased surfactant production
- Weak respiratory muscles and compliant chest wall
- Immature respiratory control center leading to apnea of prematurity
- Increased work of breathing and susceptibility to respiratory distress syndrome (RDS)
Cardiovascular System
- Immature myocardium with reduced contractility
- Patent ductus arteriosus (PDA) more common
- Increased risk of hypotension and poor perfusion
- Delayed transition from fetal to neonatal circulation
Thermoregulation
- High surface area to body mass ratio
- Limited subcutaneous fat for insulation
- Immature hypothalamic temperature control
- Limited capacity for non-shivering thermogenesis
- Increased heat loss through evaporation, conduction, convection, and radiation
Gastrointestinal System
- Immature digestive enzymes and absorption capacity
- Delayed gastric emptying and intestinal motility
- Immature intestinal barrier function increasing NEC risk
- Limited glycogen stores leading to hypoglycemia
Neurological System
- Ongoing brain development and myelination
- Fragile germinal matrix increasing IVH risk
- Immature blood-brain barrier
- Weak sucking and swallowing reflexes
- Immature sleep-wake cycles
Immune System
- Reduced maternal IgG transfer (especially in extremely preterm)
- Immature neutrophil function and complement system
- Reduced inflammatory response capacity
- Higher susceptibility to infections
Intrauterine Growth Restriction (IUGR) Pathophysiology
IUGR is a major cause of low birth weight, even in term infants. The primary pathophysiological mechanism involves placental insufficiency:
| IUGR Type | Pathophysiology | Characteristics |
|---|---|---|
| Symmetric IUGR | Early insult affecting overall growth; reduced cell number and size | Proportionate reduction in weight, length, and head circumference |
| Asymmetric IUGR | Later insult with placental insufficiency; brain-sparing effect | Disproportionate reduction with relatively preserved head circumference |
| Mixed IUGR | Combination of early and late insults | Mixed features of symmetric and asymmetric patterns |
Physiological Basis for Kangaroo Care Efficacy
Understanding the pathophysiology of LBW infants helps explain why kangaroo care is so effective. The skin-to-skin contact in kangaroo care:
- Stabilizes thermoregulation through direct heat transfer from parent to infant
- Reduces stress and cortisol levels, promoting better neurological development
- Stimulates vagal activity, improving gastrointestinal function and weight gain
- Regulates breathing patterns through maternal breathing synchronization
- Facilitates colonization with maternal microbiota, enhancing immune function
- Promotes oxytocin release, enhancing bonding and maternal milk production
Risk Factors and Causes
Identifying risk factors for low birth weight is essential for preventive strategies and early intervention. These factors can be categorized into maternal, fetal, and environmental causes, many of which can be addressed through appropriate prenatal care and public health measures.
Maternal Factors
| Category | Risk Factors | Impact |
|---|---|---|
| Demographic |
|
Associated with limited access to prenatal care, nutritional deficiencies, and increased stress |
| Medical Conditions |
|
Can cause placental insufficiency, vascular compromise, metabolic disturbances, and inflammatory responses |
| Obstetric History |
|
Indicates potential underlying problems with carrying pregnancy to term or supporting optimal fetal growth |
| Nutritional Status |
|
Limits nutrients available for fetal growth and placental development |
Fetal Factors
Genetic Factors
- Chromosomal abnormalities (e.g., trisomies)
- Congenital anomalies and syndromes
- Genetic growth disorders
- Inborn errors of metabolism
Multiple Gestations
- Twins, triplets, or higher order multiples
- Shared placental circulation issues
- Twin-to-twin transfusion syndrome
- Competition for maternal resources
Infections
- TORCH infections (Toxoplasmosis, Other, Rubella, Cytomegalovirus, Herpes)
- Zika virus
- HIV and associated opportunistic infections
- Bacterial infections leading to chorioamnionitis
Environmental Factors
Environmental and Behavioral Risk Factors
- Substance Use: Tobacco (20-30% increased risk of LBW), alcohol, illicit drugs (cocaine, heroin, methamphetamine)
- Environmental Toxins: Lead, mercury, arsenic, pesticides, air pollution
- Occupational Hazards: Prolonged standing, physical exertion, exposure to chemicals, shift work
- Psychological Factors: Chronic stress, depression, anxiety, domestic violence, inadequate social support
- Healthcare Access: Inadequate prenatal care, barriers to healthcare services
- Geographic Factors: High altitude residence (>2500m) associated with lower birth weights
Understanding these risk factors is essential for implementing preventive strategies. For infants already born with low birth weight, interventions like kangaroo care become crucial for mitigating adverse outcomes and promoting optimal development.
Assessment of Low Birth Weight Infants
Thorough assessment is crucial for determining the appropriate care plan for LBW infants, including the implementation of kangaroo care. The assessment should be comprehensive, systematic, and ongoing to monitor progress and detect complications early.
Physical Assessment
| Assessment Component | Key Observations in LBW Infants | Nursing Implications |
|---|---|---|
| General Appearance |
|
Assess for proportionality to differentiate between preterm LBW and IUGR |
| Anthropometric Measurements |
|
Use growth charts specific to gestational age; monitor measurements regularly to assess growth trajectory |
| Skin |
|
High risk for skin breakdown; evaluate for jaundice, cyanosis, and perfusion |
| Respiratory System |
|
Monitor for signs of respiratory distress; position to maintain airway; assess response to kangaroo care |
| Cardiovascular System |
|
Monitor for bradycardia, tachycardia, and signs of poor perfusion; assess cardiovascular stability during kangaroo care |
Neurological Assessment
Reflexes and Muscle Tone
- Moro reflex
- Sucking and rooting reflexes
- Grasp reflex
- Muscle tone assessment
- Posture and spontaneous movement
Behavioral Assessment
- State regulation (using NNNS or NBAS)
- Response to handling and stimulation
- Sleep-wake cycles
- Signs of stress or stability
- Consolability
Neurodevelopmental Signs
- Head control
- Visual tracking
- Auditory responses
- Self-regulation abilities
- Signs of neurological impairment
Diagnostic Tests and Monitoring
| Diagnostic Component | Tests/Measurements | Purpose |
|---|---|---|
| Laboratory Tests |
|
Detect anemia, infection, hypoglycemia, electrolyte imbalances, hyperbilirubinemia, and respiratory status |
| Imaging Studies |
|
Assess for intraventricular hemorrhage, respiratory conditions, gastrointestinal issues, and cardiac anomalies |
| Continuous Monitoring |
|
Ongoing assessment of vital signs and detection of apnea, bradycardia, desaturation, and temperature instability |
Assessment During Kangaroo Care
During kangaroo care sessions, nurses should continue to monitor:
- Infant’s temperature (should maintain between 36.5-37.5°C)
- Respiratory pattern and rate (often stabilizes during KC)
- Heart rate and oxygen saturation
- Behavioral cues and stress signals
- Parent’s comfort and confidence
Document findings before, during, and after kangaroo care sessions to evaluate the infant’s response and adaptation.
Complications of Low Birth Weight
Low birth weight infants face numerous complications that can affect both short-term survival and long-term outcomes. Understanding these complications is essential for implementing preventive measures and appropriate interventions, including kangaroo care.
Short-term Complications
Respiratory Complications
- Respiratory Distress Syndrome (RDS): Due to surfactant deficiency
- Bronchopulmonary Dysplasia (BPD): Chronic lung disease
- Apnea of Prematurity: Pauses in breathing >20 seconds
- Pneumonia: Higher susceptibility to infections
Cardiovascular Complications
- Patent Ductus Arteriosus (PDA): Failure of fetal vessel to close
- Hypotension: Low blood pressure
- Poor Peripheral Perfusion: Compromised circulation
- Bradycardia: Often associated with apnea
Metabolic & Thermoregulatory
- Hypothermia: Difficulty maintaining temperature
- Hypoglycemia: Low blood sugar due to limited glycogen stores
- Electrolyte Imbalances: Sodium, potassium, calcium disruptions
- Metabolic Acidosis: Acid-base imbalance
Neurological Complications
- Intraventricular Hemorrhage (IVH): Bleeding into ventricles
- Periventricular Leukomalacia (PVL): White matter damage
- Seizures: Due to brain injury or metabolic disturbances
- Hydrocephalus: Excessive CSF accumulation
Sensory Complications
- Retinopathy of Prematurity (ROP): Abnormal retinal blood vessel development
- Hearing Impairment: Higher risk in LBW infants
- Hyperbilirubinemia: Can affect auditory pathways
- Sensory Processing Issues: Related to NICU environment
Infectious Complications
- Sepsis: Increased susceptibility to infections
- Necrotizing Enterocolitis (NEC): Intestinal inflammation and necrosis
- Hospital-Acquired Infections: Related to prolonged hospitalization
- Meningitis: CNS infection
Long-term Complications
| System | Long-term Complications | Impact on Development |
|---|---|---|
| Neurological |
|
May affect academic performance, social integration, and independence in daily activities |
| Respiratory |
|
Can limit physical activity, increase healthcare utilization, and affect quality of life |
| Growth and Metabolic |
|
The “fetal origins” hypothesis suggests increased risk of adult chronic diseases due to fetal adaptations to undernutrition |
Protective Effect of Kangaroo Care
Research has demonstrated that kangaroo care can mitigate many complications associated with low birth weight:
- Reduces hypothermia risk by 78% through effective thermoregulation
- Decreases nosocomial infection rates by 47% through exposure to maternal microbiota
- Improves weight gain by up to 30% compared to conventional care
- Reduces apnea episodes by 75% through respiratory synchronization with the parent
- Promotes better neurodevelopmental outcomes with improved scores on developmental assessments at 6, 12, and 24 months
- Decreases mortality by up to 40% in resource-limited settings when implemented correctly
Kangaroo Mother Care: Introduction and History
Kangaroo care represents one of the most significant innovations in the care of low birth weight infants in the past century. Its evolution from a necessity-driven practice to an evidence-based standard of care illustrates the power of simple, natural interventions in advancing neonatal health outcomes.
Historical Development
Origins in Colombia (1978)
Dr. Edgar Rey Sanabria at the Instituto Materno Infantil in Bogotá, Colombia, developed kangaroo care as a response to:
- Overcrowded nurseries with insufficient incubators
- High rates of nosocomial infections
- Insufficient nursing staff
- High mortality rates among LBW infants
Research and Validation (1980s-1990s)
Dr. Nathalie Charpak and colleagues conducted pioneering research that demonstrated:
- Effectiveness of KMC compared to conventional incubator care
- Improvements in survival rates, weight gain, and breastfeeding
- Reduced hospital stay and cost-effectiveness
- Long-term benefits for growth and development
Global Adoption (2000s-Present)
WHO and UNICEF endorsed kangaroo care as an essential intervention for LBW infants, leading to:
- Implementation in both resource-limited and high-income settings
- Integration into standard NICU practices worldwide
- Expansion of the concept to include fathers and other family members
- Development of standardized protocols and training materials
“The significance of kangaroo care lies not just in its effectiveness but in its elegant simplicity—harnessing the power of the maternal-infant relationship to address complex physiological needs.” — Dr. Nathalie Charpak
Conceptual Framework
Kangaroo Mother Care is based on three key principles that form its conceptual foundation:
| Core Component | Description | Physiological Basis |
|---|---|---|
| Kangaroo Position | Continuous, prolonged skin-to-skin contact between infant and parent in a vertical position between the breasts | Facilitates thermoregulation, cardiorespiratory stability, stress reduction, and sensory stimulation |
| Exclusive Breastfeeding | When possible, exclusive breastfeeding or breast milk feeding (expressed milk when direct feeding not possible) | Provides optimal nutrition, immune protection, and promotes mother-infant bonding |
| Support and Early Discharge | Comprehensive support for mother-infant dyad and early discharge with close follow-up | Reduces hospital-acquired infections, promotes family integration, and improves maternal confidence |
Evolution of Kangaroo Care Concepts
The conceptual understanding of kangaroo care has evolved over time:
- Original Model (1970s-1980s): Alternative to incubator care, primarily focused on temperature regulation and resource limitations
- Expanded Model (1990s): Recognition of broader physiological benefits including cardiorespiratory stability and weight gain
- Comprehensive Model (2000s): Integration of neurodevelopmental benefits, stress reduction, and long-term outcomes
- Family-Centered Model (Current): Incorporation of fathers, siblings, and family dynamics; emphasis on psychosocial and attachment benefits
Components of Kangaroo Mother Care
Kangaroo care comprises several interconnected components that work synergistically to provide comprehensive support for low birth weight infants. Understanding these elements is essential for proper implementation and maximizing benefits.
Key Components of Kangaroo Mother Care
Skin-to-Skin Contact
The cornerstone of kangaroo care, involving direct skin-to-skin placement of the infant on the parent’s chest.
- Infant dressed only in diaper and cap
- Placed between parent’s breasts in vertical position
- Head turned to one side, slightly extended
- Hips flexed, frog-like position
- Secured with cloth wrap or band
Kangaroo Position
Specific positioning that optimizes physiological benefits and safety.
- Upright position (60-90° angle)
- Face visible; nose and mouth unobstructed
- Chest-to-chest contact
- Abdomen at level of parent’s epigastrium
- Support for infant’s back and neck
- Parent semi-reclined at 30-45° when resting
Duration and Timing
The frequency and duration of sessions are critical factors.
- Continuous KMC: 20+ hours/day
- Intermittent KMC: Regular sessions of 60+ minutes
- Begin as early as clinically stable
- Continue until infant no longer tolerates position (typically around 40 weeks corrected age)
- Minimum effective duration: 1-2 hours per session
Nutrition and Feeding
Optimizing nutrition through breast milk and supportive feeding strategies.
- Exclusive breastfeeding when possible
- Expressed breast milk when direct feeding not possible
- Non-nutritive sucking opportunities
- Transition from gavage to oral feeding
- Support for milk production and lactation
Discharge and Follow-up
Continued support beyond hospital settings.
- Early discharge when medically stable
- Home-based continuation of KMC
- Regular follow-up appointments
- Growth and development monitoring
- Parental education and support
Family Support
Comprehensive support for the family unit.
- Education on KMC benefits and techniques
- Psychological support for parents
- Involvement of fathers and other family members
- Peer support from experienced KMC families
- Social service linkages as needed
Types of Kangaroo Care Implementation
| Implementation Model | Description | Setting | Considerations |
|---|---|---|---|
| Continuous KMC | 24-hour skin-to-skin contact with brief interruptions only for hygiene | KMC wards, home post-discharge | Requires significant family commitment; optimal for stable infants; shown to have maximum benefits |
| Intermittent KMC | Regular skin-to-skin sessions (1-3 hours) several times daily | NICU, special care nursery | More practical in conventional NICU settings; beneficial but less impact than continuous |
| Extended Intermittent KMC | Longer sessions (4+ hours) daily but not continuous | NICU with rooming-in facilities | Balance between feasibility and effectiveness; good transition model |
| Community-based KMC | Implementation outside hospital settings | Home, community health centers | Requires strong support system and training; essential in resource-limited areas |
Important Considerations for Component Integration
- Individualization: Components should be adapted to the infant’s medical status, gestational age, and family circumstances
- Progressive Implementation: Begin with shorter sessions and gradually increase duration as tolerated
- Monitoring: Continuous assessment of infant’s response to kangaroo care
- Integration with Medical Care: KMC should complement, not replace, necessary medical interventions
- Cultural Sensitivity: Adapt implementation to align with family cultural backgrounds and preferences
Implementation of Kangaroo Mother Care
Successful implementation of kangaroo care requires a systematic approach, careful preparation, and ongoing support. This section outlines the practical aspects of implementing KMC in various healthcare settings.
Eligibility Criteria and Patient Selection
| Criteria | Considerations | Exclusion Criteria |
|---|---|---|
| Infant Stability |
|
|
| Birth Weight/Gestational Age |
|
|
| Parental Factors |
|
|
Kangaroo Mother Care Technique
Preparation
- Explain procedure and benefits to parents
- Ensure privacy and comfortable environment
- Adjust room temperature (22-24°C)
- Parent should wear front-opening clothing
- Remove jewelry and ensure clean chest
- Prepare comfortable chair/bed with back support
- Have monitoring equipment ready if needed
Transfer Technique
- Parent seated in semi-reclined position
- Dress infant in only diaper and cap
- Use “scoop” technique for transfer
- Support infant’s head, neck, and bottom
- Place vertically between parent’s breasts
- Turn head to side with neck slightly extended
- Position legs in flexed “frog-leg” position
Securing the Position
- Use supportive binding cloth/wrap
- Start at parent’s back, bring around front
- Secure snugly but not too tight
- Ensure infant’s face is visible
- Check breathing is unobstructed
- Verify proper positioning (upright, head supported)
- Secure any medical equipment/tubes
Safety Considerations During Transfer
- Always use two providers for initial transfers (especially with equipment)
- One person focuses solely on airway/equipment
- Move all tubing/lines together with the infant
- Consider practice with a doll before first session
- Document all positioning details and infant’s response
Duration and Frequency
| Level of Implementation | Duration Recommendations | Clinical Considerations |
|---|---|---|
| Initial Sessions |
|
|
| Established Sessions |
|
|
| Optimal Implementation |
|
|
Implementation Progress Indicators
Signs that kangaroo care is being implemented effectively:
- Physiological Stability: Steady vital signs during and after transfer
- Behavioral Cues: Relaxed posture, reduced stress signals, deeper sleep states
- Growth Parameters: Consistent weight gain, improved feeding
- Parent Confidence: Increased comfort with holding and caring for infant
- Integration: KMC becomes routine part of daily care rather than special event
Monitoring During Kangaroo Care
| Parameter | Monitoring Approach | Expected Response | Concerns/Interventions |
|---|---|---|---|
| Temperature | Check before, during (if needed), and after sessions | Maintenance of 36.5-37.5°C; often increases to optimal range during KMC | If <36.5°C, add blanket over infant's back; if >37.5°C, check for overdressing |
| Respiratory Status | Observe breathing pattern; monitor oxygen saturation if indicated | Stabilization of breathing pattern; potentially reduced apnea | Position adjustment if breathing appears compromised; ensure airway patency |
| Heart Rate | Monitor per unit protocol; continuous for unstable infants | Often decreases slightly to more stable range | If significant bradycardia occurs, check positioning and airway |
| Behavioral State | Observe sleep/wake states, stress cues, feeding readiness | Deeper sleep states, reduced stress signals, increased quiet alert periods | If showing stress cues (splayed fingers, arching), assess for discomfort or need for position adjustment |
Benefits of Kangaroo Mother Care
The benefits of kangaroo care are extensive and well-documented through numerous randomized controlled trials and meta-analyses. These benefits span physiological, psychological, and developmental domains, providing a compelling rationale for implementing KMC as a standard of care for low birth weight infants.
Physiological Benefits
Thermoregulation
- Direct heat transfer from parent to infant
- Reduced incidence of hypothermia by up to 88%
- Stable thermal environment compared to incubator fluctuations
- Lower energy expenditure for temperature maintenance
Cardiorespiratory Stability
- Reduced apnea episodes by 75%
- More stable heart rate patterns
- Improved oxygen saturation
- Synchronization with parent’s breathing pattern
- Reduced bradycardia events
Growth and Development
- Average 30% better weight gain
- Improved linear growth
- Better head circumference gains
- Earlier achievement of growth milestones
- More efficient metabolism
Infection Prevention
- 47% reduction in nosocomial infections
- Colonization with maternal microbiota
- Transfer of maternal antibodies
- Reduced exposure to hospital pathogens
- Lower sepsis rates
Breastfeeding Outcomes
- Increased breastfeeding rates by 50%
- Extended breastfeeding duration
- Higher milk production volumes
- Earlier establishment of direct breastfeeding
- Better weight gain from improved feeding
Mortality Reduction
- Up to 40% reduction in mortality
- Greatest impact in low-resource settings
- Beneficial across weight categories
- Sustained mortality benefit at follow-up
- Life-saving intervention requiring minimal resources
Psychological Benefits
| Benefit Category | For Infant | For Parents |
|---|---|---|
| Stress Reduction |
|
|
| Attachment and Bonding |
|
|
| Mental Health Outcomes |
|
|
“When mothers and babies are separated, the developmental processes of attachment, bonding, and emotional regulation are disrupted. Kangaroo care restores these crucial connections, creating a foundation for optimal development.” — Dr. Ruth Feldman, Neuroscientist
Developmental Benefits
Long-term Neurodevelopmental Outcomes
Research has demonstrated significant long-term benefits of kangaroo care on neurodevelopment:
- Cognitive Development: Higher scores on developmental tests at 6, 12, and 24 months; better performance on cognitive assessments at school age
- Motor Development: Earlier achievement of motor milestones; better fine and gross motor coordination at follow-up
- Behavioral Regulation: Improved self-regulation; reduced hyperactivity; better attention spans
- Sleep Organization: More mature sleep patterns; better sleep quality and duration
- Stress Reactivity: More adaptive stress response systems; better physiological regulation under stress
- Parent-Child Interactions: More reciprocal interactions; better maternal sensitivity; stronger attachment security
Economic Benefits
Beyond clinical outcomes, kangaroo care offers significant economic advantages:
- Reduced hospital stay by an average of 1.6 days for stable LBW infants
- Lower hospital readmission rates
- Decreased need for costly interventions (ventilation, antibiotics)
- Significantly lower cost compared to conventional incubator care
- Estimated cost savings of USD $2,384 per infant in high-income countries
- Even greater cost-effectiveness in low and middle-income settings
- Reduced long-term costs related to developmental interventions
A cost-benefit analysis showed that for every $1 invested in kangaroo care implementation, there is a return of $7 in healthcare savings.
Nursing Interventions for Low Birth Weight Infants
Nurses play a pivotal role in caring for low birth weight infants and implementing kangaroo care effectively. This section outlines the comprehensive nursing interventions required for optimal outcomes in LBW infants.
Essential Nursing Interventions
| Intervention Category | Specific Interventions | Nursing Responsibilities |
|---|---|---|
| Thermoregulation |
|
|
| Respiratory Support |
|
|
| Nutritional Support |
|
|
| Infection Prevention |
|
|
Kangaroo Care Implementation by Nurses
Parent Education
- Explain benefits and procedure of KMC
- Demonstrate proper positioning
- Review safety considerations
- Teach recognition of infant cues
- Provide written materials and resources
Direct Assistance
- Assist with infant transfer
- Help secure infant in position
- Manage medical equipment/tubes
- Ensure comfort of parent and infant
- Provide privacy during sessions
Monitoring
- Assess vital signs before, during, after
- Monitor infant’s behavioral cues
- Evaluate parent’s comfort and confidence
- Document duration and infant responses
- Track long-term outcomes
KANGAROO CARE Nursing Implementation Mnemonic
- Know the eligibility criteria for each infant
- Assess infant’s readiness and stability
- Nurture parent’s confidence through education
- Guide proper positioning and transfer techniques
- Adjust environment for optimal experience
- Respect privacy and promote bonding
- Observe and monitor safety parameters
- Optimize duration based on tolerance
- Coordinate KMC with feeding and care routines
- Acknowledge and address parent concerns
- Record and document outcomes
- Encourage continuation after discharge
Developmental Care Integration
Integrating Kangaroo Care with Developmental Care Principles
Kangaroo care should be implemented as part of a comprehensive developmental care approach for LBW infants:
- Environmental Modifications: Dim lighting during KMC; reduce noise levels; maintain day-night cycles
- Positioning: Support physiological flexion during KMC; ensure containment
- Clustering Care: Schedule nursing interventions around KMC sessions to minimize disruptions
- Pain Management: Implement KMC before, during, or after painful procedures as appropriate
- Family-Centered Care: Include both parents and other family members in KMC; respect cultural preferences
- Individualized Care: Adapt KMC implementation based on infant’s behavioral cues and tolerance
Discharge Planning and Home Care
| Discharge Planning Component | Nursing Interventions |
|---|---|
| Home KMC Preparation |
|
| Education for Warning Signs |
|
| Follow-up Coordination |
|
Challenges in Implementing Kangaroo Mother Care
Despite its proven benefits, implementing kangaroo care faces various challenges across different healthcare settings. Understanding these barriers is essential for developing effective strategies to overcome them.
Healthcare Provider Barriers
- Insufficient knowledge about KMC benefits and techniques
- Concerns about infant safety and stability
- Resistance to practice change
- Perception of increased workload
- Lack of standardized protocols
- Insufficient training opportunities
Institutional Barriers
- Limited physical space and privacy
- Inadequate comfortable seating/beds
- Restrictive visitation policies
- Insufficient staffing levels
- Lack of administrative support
- Competing priorities in care delivery
Family Barriers
- Fear of harming the fragile infant
- Distance from hospital limiting visitation
- Competing demands from other children/work
- Cultural beliefs and practices
- Discomfort in hospital environment
- Limited understanding of KMC benefits
Overcoming Implementation Challenges
| Challenge | Solutions and Strategies |
|---|---|
| Staff Knowledge Gaps |
|
| Environmental Limitations |
|
| Policy Barriers |
|
| Parent Participation Barriers |
|
Case Example: Overcoming Barriers
A tertiary NICU in an urban hospital increased kangaroo care implementation from 8% to 63% of eligible infants through:
- Developing a KMC champion team with representatives from nursing, medicine, and family support
- Creating standardized protocols with clear eligibility criteria
- Implementing staff training that included hands-on practice with transfer techniques
- Redesigning the physical space to provide comfortable chairs and privacy screens
- Establishing a parent mentor program using experienced NICU families
- Incorporating KMC documentation into electronic health records
- Regular data collection and feedback on implementation rates
Key outcome: 40% reduction in length of stay for infants receiving regular kangaroo care compared to historical controls.
Mnemonics for Nursing Students
Mnemonics are valuable tools for nursing students to remember key concepts related to low birth weight infants and kangaroo care. Here are several practical memory aids to enhance learning and clinical application.
WARM HUGS: Benefits of Kangaroo Care
- Weight gain improvement
- Attachment enhancement
- Respiratory stability
- Maternal confidence increase
- Hypothermia prevention
- Uninterrupted sleep promotion
- Gut function optimization
- Stress reduction
STABLE: Assessment of LBW Infants
- Sugar and Safe care
- Temperature regulation
- Airway maintenance
- Blood pressure monitoring
- Lab work evaluation
- Emotional support for family
POSITION: Proper KMC Technique
- Place infant skin-to-skin on parent’s chest
- Observe airway – head turned slightly
- Secure with wrap or binder
- Insure temperature stability
- Turn parent semi-upright (30-45°)
- Infant in vertical position
- Organize tubes and lines safely
- Note infant’s tolerance and vital signs
TINY: Risk Factors for LBW
- Toxins (smoking, alcohol, drugs)
- Infections (TORCH, UTI, etc.)
- Nutritional deficiencies
- Young age/advanced maternal age
CARE: Parent Education for KMC
- Continuous skin-to-skin contact
- Awareness of infant cues
- Recognition of warning signs
- Exclusive breastfeeding when possible
PRETERM: Complications of LBW
- Pulmonary issues (RDS, BPD)
- Retinopathy of prematurity
- Electrolyte imbalances
- Thermoregulation problems
- Enteral feeding difficulties
- Risk of infection
- Metabolic issues (hypoglycemia)
DAILY CHECK: KMC Nursing Documentation
- Duration of KMC session
- Assessment of vital signs before, during, after
- Infant’s tolerance and behavior
- Lines and equipment management
- Yield (benefits observed)
- Care provided during KMC
- How parents performed and felt
- Education provided
- Challenges encountered
- Key follow-up points
Global Best Practices
Different regions worldwide have developed innovative approaches to implementing kangaroo care for low birth weight infants. These global best practices offer valuable insights that can be adapted to various healthcare settings.
Regional Implementations and Innovations
Colombia (Birthplace of KMC)
- Kangaroo Foundation Model: Comprehensive ambulatory KMC program with dedicated follow-up
- Mother-Centered Approach: Mothers trained as primary caregivers with continuous KMC
- Training Center: International training hub for healthcare professionals
- Research Integration: Ongoing research with long-term follow-up studies
India
- Community KMC: Implementation in rural areas with limited healthcare access
- Grandmother Integration: Including extended family in KMC implementation
- Mobile Health Support: SMS reminders and telemedicine follow-up
- ASHA Worker Training: Community health workers as KMC promoters
Sweden
- Family-Centered NICU Design: Single-family rooms supporting 24/7 KMC
- Father Involvement: Emphasis on paternal KMC with parental leave support
- Technology Integration: Monitoring systems compatible with KMC
- Early Implementation: KMC initiated within hours of birth when stable
Malawi
- Dedicated KMC Wards: Purpose-built facilities for continuous KMC
- Peer Support System: Experienced mothers mentor new KMC mothers
- Community Follow-up: Village health workers track discharged KMC babies
- Integration with EPI: KMC follow-up aligned with immunization visits
Australia
- Indigenous Adaptations: Culturally adapted KMC for Aboriginal communities
- Family-Integrated Care: Parents as primary caregivers in NICU
- Transport KMC: Protocols for maintaining KMC during transfers
- Technology Support: Virtual connectivity for isolated families
United States
- Quality Improvement Initiatives: Structured implementation programs
- Multidisciplinary Approach: KMC teams with various specialists
- Medical Complexity: Protocols for KMC with complex medical equipment
- Parent Navigation: Dedicated staff for supporting KMC practice
WHO Kangaroo Mother Care Acceleration Initiative
The World Health Organization launched a global initiative in 2020 to accelerate KMC implementation worldwide, with these key components:
- Policy Integration: Including KMC in national maternal-newborn health policies
- Standardized Training: Global curriculum for healthcare providers
- Implementation Support: Technical assistance for scaling up programs
- Monitoring Framework: Standardized indicators for measuring KMC coverage
- Research Agenda: Addressing implementation barriers and enhancing effectiveness
Goal: Increase KMC coverage to at least 75% of eligible infants globally by 2025, potentially saving over 150,000 newborn lives annually.
Transferable Lessons from Global Experience
| Key Principle | Practical Application |
|---|---|
| Context Adaptation |
|
| Integration with Existing Systems |
|
| Continuous Support Systems |
