Abdominal Distension
Management and Care from Community Health Nursing Perspective
Table of Contents
Introduction to Abdominal Distension
Abdominal distension is defined as an enlargement of the abdomen, usually caused by the accumulation of fluid or gas. This symptom can be caused by anything from poor diet habits to underlying medical conditions. In community health nursing, proper assessment and management of abdominal distension are essential for providing appropriate care and preventing complications.
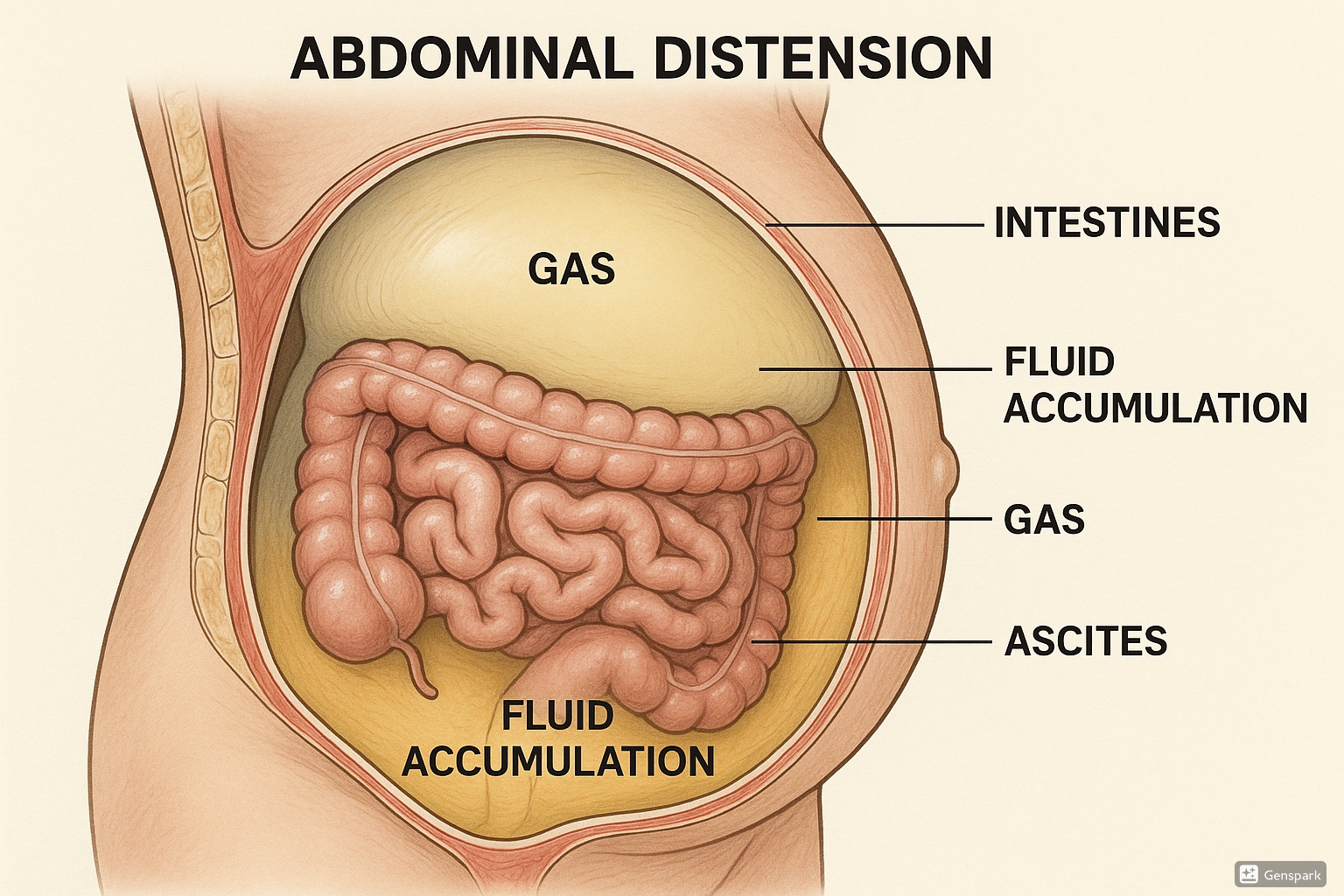
Figure 1: Anatomical illustration of abdominal distension showing fluid accumulation, gas, and affected organs.
Abdominal distension occurs in approximately 10-30% of the general population and is one of the most common symptoms reported by patients with gastrointestinal disorders. It’s particularly prevalent in patients with irritable bowel syndrome (IBS), where it affects up to 96% of cases. Understanding abdominal distension from a community health nursing perspective involves recognizing its impact on patient quality of life and implementing appropriate assessment, screening, and management strategies.
Assessment and Screening
Subjective Assessment
A focused gastrointestinal and genitourinary subjective assessment collects data about signs and symptoms of GI and GU diseases, including any digestive or nutritional issues, relevant medical or family history, and any current treatment for related issues.
| Interview Questions | Follow-up Questions |
|---|---|
| Do you have any abdominal pain? |
– Are there any associated symptoms such as fever, nausea, vomiting, or change in bowel pattern? – When did the pain start to occur? (Onset) – Where is the pain? (Location) – How long does the pain last? (Duration) – Can you describe what the pain feels like? (Characteristics) – What brings on the pain? (Aggravating factors) – What relieves the pain? (Alleviating factors) – How severe is the pain from 0-10 when it occurs? (Severity) |
| Have you noticed any changes in your abdomen? |
– When did you first notice your abdomen was distended? – Has the distension been getting better, worse, or staying the same? – Do you notice any patterns related to eating, drinking, or time of day? |
| When was your last bowel movement? |
– Have there been any changes in pattern or consistency of your stool? – Are you passing any gas? – Have you had any issues with constipation or diarrhea? |
Objective Assessment
Physical examination of the abdomen includes inspection, auscultation, palpation, and percussion. Note that for abdominal assessment, auscultation should be performed before palpation to prevent alteration of bowel sounds.
Inspection
- Observe the general contour and symmetry of the entire abdominal wall
- Assess for distention
- Assess for masses or bulges
- Note the shape of the umbilicus
- Document any abnormal movement or pulsations
Auscultation
- Begin in the right lower quadrant (RLQ)
- Move clockwise around the abdomen
- Note frequency and characteristics of bowel sounds
- Listen for vascular sounds
Palpation
- Lightly palpate the four quadrants
- Palpate the suprapubic area for bladder distention
- Note patient response to palpation (pain, guarding, rigidity)
- If the patient reports abdominal pain, palpate that area last
Percussion
- May be used to assess liver and spleen
- Can determine if costovertebral angle (CVA) tenderness is present
- Helps identify fluid vs. gas in the abdomen
Assessment Tip:
Encourage the patient to empty their bladder prior to palpation. When palpating the abdomen, ask the patient to bend their knees when lying in a supine position to enhance relaxation of abdominal muscles.
Screening Tools for Abdominal Distension
In community health settings, several screening approaches may be used to assess abdominal distension:
- Abdominal girth measurement: Measuring abdominal circumference at the umbilicus level to track changes over time
- Dietary and elimination patterns assessment: Tracking food intake, bowel movements, and fluid balance
- Symptom severity scales: Using standardized scales to rate distension severity
- Physical examination findings: Documenting objective findings related to distension
Causes and Clinical Features
The 6 F’s of Abdominal Distension
A useful mnemonic for remembering the causes of abdominal distension is the “6 F’s”:
The 6 F’s of Abdominal Distension
- Flatus: Gas accumulation in the gastrointestinal tract
- Fluid: Ascites, often due to liver disease or heart failure
- Fat: Obesity or adipose tissue accumulation
- Feces: Constipation or bowel obstruction
- Fetus: Pregnancy
- Fatal growth: Tumors or malignancies
Common Causes
| Category | Causes | Clinical Features |
|---|---|---|
| Gastrointestinal |
– Irritable bowel syndrome – Constipation – Intestinal obstruction – Gastroparesis |
– Bloating after meals – Changes in bowel movements – Abdominal pain – Nausea/vomiting |
| Fluid Accumulation |
– Liver cirrhosis – Heart failure – Kidney disease – Peritonitis |
– Progressive distension – Weight gain – Shifting dullness on percussion – Fluid wave sign |
| Malignancy |
– Ovarian cancer – Colorectal cancer – Pancreatic cancer – Peritoneal carcinomatosis |
– Progressive distension – Weight loss – Night sweats – Early satiety |
Distinguishing Between Bloating and Distension
Though often used interchangeably, bloating and distension are not identical:
- Bloating: A sensation of increased abdominal pressure, often described as a feeling of excessive gas.
- Distension: Observable enlargement of the abdomen due to accumulation of gas, fluid, or solids.
About 50% of patients with a sensation of bloating also describe abdominal distension. Bloating is more common in patients with IBS, whereas distension is more readily seen in patients with constipation and pelvic floor dysfunction.
Management Approaches
Effective management of abdominal distension depends on identifying and treating the underlying cause. In community health settings, several evidence-based approaches can be implemented:
Dietary Interventions
Low-FODMAP Diet
The low-FODMAP (Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols) diet has shown significant success in relieving symptoms of bloating and abdominal distension, decreasing symptoms in at least 75% of patients.
FODMAPs include:
- Fructo-oligosaccharides (fructans)
- Galacto-oligosaccharides
- Lactose
- Fructose
- Sorbitol and mannitol
Other Dietary Modifications
- Avoid carbonated beverages
- Choose fiber carefully (slowly fermented fibers like psyllium/ispaghula husk are better tolerated)
- Small, frequent meals instead of large meals
- Adequate hydration
- Identify and eliminate food intolerances
Pharmacological Interventions
| Category | Examples | Use in Abdominal Distension |
|---|---|---|
| Prosecretory and Promotility Agents | Linaclotide, Prucalopride, Lubiprostone | Effective for reducing bloating in patients with constipation and IBS-C by improving intestinal transit |
| Antibiotics | Rifaximin, Neomycin | May help when small intestinal bacterial overgrowth (SIBO) is suspected |
| Probiotics | Bifidobacterium infantis, Bifidobacterium lactis | Some evidence of benefit for reducing bloating, particularly with bifidobacteria strains |
| Antispasmodics | Dicyclomine, Hyoscyamine | Can relieve abdominal pain and spasms that contribute to distension |
| Gas-reducing agents | Simethicone, Activated charcoal | May provide symptomatic relief for gas-related distension |
Non-pharmacological Interventions
Physical Activity
- Regular exercise improves digestive function
- Stimulates intestinal contractions and gas clearance
- Helps reduce constipation
- Maintains healthy abdominal muscle tone
Behavioral Therapies
- Biofeedback for pelvic floor dyssynergia
- Diaphragmatic breathing techniques
- Stress management strategies
- Hypnotherapy for IBS-related symptoms
Management Tip:
Treatment of abdominal distension should focus on addressing the underlying cause rather than just treating the symptom. For example, if constipation is causing distension, focus on improving bowel motility through diet, hydration, and appropriate medications.
Standing Orders for Abdominal Distension
Definition and Uses
Standing orders are written documents containing rules, policies, procedures, regulations, and orders for the conduct of patient care in various situations. They are specifically designed for a group of patients with the same condition or procedure.
In community health settings, standing orders allow for consistency in the assessment and management of patients with abdominal distension, enabling nurses to initiate appropriate interventions without requiring immediate physician orders for each step.
Sample Standing Order for Abdominal Distension
STANDING ORDER: ABDOMINAL DISTENSION
I. INITIATE IMMEDIATE SUPPORTIVE CARE
- Position patient for comfort
- Monitor vital signs
- Apply oxygen if SpO2 < 90% or respiratory distress is present
- Cardiac monitoring as appropriate
II. INCLUSIONS
Adults (>16 years) presenting with abdominal distension
III. EXCLUSIONS
Do not implement standing order for patients with:
- Pregnancy
- Meeting trauma triage criteria
- Abdominal trauma
- Mixed symptoms (chest pain, shortness of breath, altered consciousness)
- Known history of cardiac disease
IV. ASSESSMENT AND INTERVENTIONS
STABLE (SBP >90 or HR <110)
- Assess acuity and severity of distension
- Transport in position of comfort
- Provide supportive measures as indicated
UNSTABLE (SBP <90 or HR >110)
- Initiate large bore IV of Normal Saline
- If patient is pale/diaphoretic, administer fluid bolus (20 ml/kg)
- For nausea or vomiting, administer antiemetics
- Notify receiving facility if condition deteriorates
V. NURSING INTERVENTIONS
- Monitor vital signs every 15 minutes for unstable patients, every 30 minutes for stable patients
- Maintain accurate intake and output records
- Measure abdominal girth at umbilicus level (document time and measurement)
- Assess bowel sounds in all four quadrants
- Implement comfort measures (positioning, warm blankets)
- Restrict oral intake as appropriate
- Prepare for possible diagnostic tests (abdominal x-ray, CT scan)
VI. DOCUMENTATION
Document all assessment findings, interventions, and patient responses, including:
- Vital signs and abdominal girth measurements
- Character of bowel sounds
- Patient’s description of symptoms
- Interventions performed and responses
- Notification of physician/provider
Important Note:
Standing orders should be reviewed and approved by the healthcare facility’s medical director and updated regularly to reflect current evidence-based practice. Community health nurses should be thoroughly trained in the implementation of these standing orders.
First Aid Measures
First aid measures for abdominal distension in community settings focus on providing immediate comfort, preventing complications, and determining when medical assistance is needed. These measures vary based on the suspected cause of distension.
Immediate Comfort Measures
Positioning
- Assist to a position of comfort
- Knee-to-chest position may relieve gas pain
- Semi-Fowler’s position (30-45° elevation) may ease breathing if distension is severe
- Left side-lying position can help with gas passage
Environmental Modifications
- Ensure privacy and dignity
- Loosen tight clothing around the waist
- Maintain comfortable room temperature
- Provide easy access to bathroom facilities
Specific First Aid Interventions
| Suspected Cause | First Aid Measures | When to Seek Medical Help |
|---|---|---|
| Gas-Related Distension |
– Encourage walking – Gentle abdominal massage in clockwise direction – Peppermint tea if available – Avoid carbonated beverages |
If severe pain develops or distension worsens despite measures |
| Constipation-Related |
– Increase fluid intake – Warm liquids may stimulate bowel movement – Light activity if tolerated |
If no bowel movement for >3 days or accompanied by severe pain |
| Fluid Accumulation (Ascites) |
– Semi-Fowler’s position – Avoid sodium-rich foods – Monitor for breathing difficulties |
If breathing difficulties, rapid weight gain, or increasing distension |
| Trauma-Related |
– DO NOT apply pressure to distended abdomen – Keep patient still – Nothing by mouth – Monitor vital signs |
Immediate medical attention required |
Warning Signs Requiring Immediate Medical Attention:
- Severe, sudden-onset abdominal pain
- Rigid, board-like abdomen
- Signs of shock (rapid pulse, hypotension, dizziness)
- Fever above 101°F (38.3°C)
- Vomiting blood or passing bloody or black, tarry stools
- Inability to pass gas or stool
- Rapid increase in abdominal girth over short period
- Respiratory distress due to abdominal distension
General First Aid Instructions for Community Health Nurses
- Assess ABCs (Airway, Breathing, Circulation)
- Measure and document vital signs
- Perform focused abdominal assessment
- Position patient for comfort
- Implement appropriate comfort measures based on suspected cause
- Monitor for warning signs requiring medical attention
- Provide clear instructions to patient or caregiver
- Document all findings and interventions
- Arrange appropriate follow-up or referral
Nursing Interventions
Nursing interventions for abdominal distension involve a systematic approach using the nursing process of assessment, diagnosis, planning, implementation, and evaluation. The following interventions are tailored for community health settings where resources may be limited compared to hospital environments.
Nursing Diagnoses Related to Abdominal Distension
| Nursing Diagnosis | Related Factors |
|---|---|
| Acute Pain related to increased abdominal pressure | Gas accumulation, constipation, inflammation |
| Impaired Gas Exchange related to pressure on diaphragm | Severe abdominal distension limiting diaphragmatic movement |
| Constipation related to decreased GI motility | Medication effects, dehydration, immobility |
| Risk for Ineffective Breathing Pattern related to upward pressure on diaphragm | Ascites, severe gaseous distension |
| Imbalanced Nutrition: Less Than Body Requirements related to early satiety | Abdominal pressure causing feeling of fullness |
| Ineffective Management of Therapeutic Regimen related to complexity of dietary changes | Multiple dietary restrictions, lack of understanding |
Practical Nursing Interventions
Assessment and Monitoring
- Measure and document abdominal girth at same location daily
- Monitor vital signs, focusing on respiratory rate and effort
- Assess bowel sounds in all four quadrants
- Evaluate for signs of dehydration
- Document stool frequency, consistency, and characteristics
- Assess pain using appropriate scale
Comfort Measures
- Position patient to minimize pressure on diaphragm
- Apply warmth to abdomen if comfortable for patient
- Provide small, frequent meals to avoid overfilling stomach
- Ensure bathroom accessibility
- Teach patient relaxation techniques
- Maintain adequate environmental temperature
Elimination Management
- Develop individualized bowel management program
- Encourage adequate fluid intake (30-35 ml/kg/day)
- Promote physical activity appropriate to patient’s condition
- Administer prescribed medications for constipation
- Teach proper body mechanics for effective elimination
- Maintain privacy during elimination
Nutritional Support
- Collaborate with dietitian for individualized meal planning
- Advise on low-FODMAP diet if appropriate
- Educate on foods that commonly cause gas
- Teach proper eating habits (slow eating, thorough chewing)
- Monitor weight regularly
- Encourage small, frequent meals
Patient Education
Education is a critical nursing intervention for managing abdominal distension in community settings. Patients should be educated about:
- Understanding the cause of their abdominal distension
- Recognizing warning signs requiring medical attention
- Proper dietary choices to reduce distension
- Medication administration and potential side effects
- Self-monitoring techniques (abdominal girth measurement)
- Activity modifications to promote comfort
- Stress management techniques
- When and how to access medical care
Documentation Guidelines:
Document comprehensive assessment findings, interventions performed, patient’s response to interventions, and education provided. Include specific measurements (abdominal girth), characteristics of distension, pain levels, and bowel patterns to facilitate tracking of improvement or deterioration over time.
Community Health Nursing Considerations
Community health nurses face unique challenges and opportunities when managing abdominal distension outside of hospital settings. The following considerations are important for effective community-based care:
Resource Management
Limited Equipment Considerations
- Use simple measuring tape for abdominal girth
- Teach family members basic monitoring techniques
- Create simple charts for tracking symptoms
- Utilize telehealth services when available
- Develop contingency plans for equipment needs
Home Environment Assessment
- Evaluate food storage and preparation facilities
- Assess bathroom accessibility
- Identify environmental barriers to care
- Evaluate social support systems
- Determine need for home health assistance
Cultural Considerations
Cultural factors can significantly impact management of abdominal distension in community settings:
- Respect cultural dietary practices while making necessary modifications
- Consider cultural beliefs about digestive health and illness
- Acknowledge traditional remedies that may complement medical care
- Ensure educational materials are culturally appropriate and translated if needed
- Be sensitive to privacy concerns during abdominal assessment
Prevention Strategies
Community health nurses play a vital role in preventing abdominal distension through:
Primary Prevention
- Nutritional education
- Hydration promotion
- Physical activity encouragement
- Stress management techniques
Secondary Prevention
- Early symptom recognition
- Screening high-risk populations
- Prompt intervention for minor symptoms
- Regular assessment of chronic conditions
Tertiary Prevention
- Preventing recurrence
- Managing chronic conditions
- Rehabilitation after acute episodes
- Long-term monitoring
Community Resources and Referrals
Community health nurses should be familiar with available resources for patients with abdominal distension:
- Dietitian services for specialized dietary needs
- Support groups for specific conditions (IBS, Crohn’s disease, celiac disease)
- Transportation services to medical appointments
- Home health agencies for ongoing monitoring
- Financial assistance programs for medications and equipment
- Community education programs about digestive health
- Food assistance programs offering appropriate dietary options
Telehealth Applications:
Consider implementing telehealth solutions for remote monitoring of patients with chronic abdominal distension. This can include video consultations, photo documentation of abdominal distension, and virtual support groups. Develop protocols for determining when in-person assessment is necessary versus when telehealth monitoring is sufficient.
Case Studies
The following case studies illustrate common scenarios of abdominal distension encountered in community health nursing practice. Each case highlights assessment findings, interventions, and outcomes.
Case Study 1: Gas-Related Distension
Mrs. Chen, 68-year-old female with chronic constipation
Presentation: Mrs. Chen reports increasing abdominal distension over three days with mild discomfort. She has had no bowel movement for four days. Diet history reveals increased consumption of beans, broccoli, and carbonated beverages at a family gathering.
Assessment Findings: Abdomen distended, tympanic on percussion, hyperactive bowel sounds, no tenderness on palpation.
Nursing Interventions:
- Position in left side-lying to facilitate gas passage
- Encourage gentle walking
- Teach abdominal massage technique
- Advise on dietary modifications to reduce gas formation
- Educate on proper hydration and fiber intake
Outcome: After implementing these measures for 24 hours, Mrs. Chen experienced significant relief of distension following passage of flatus and had a bowel movement. Follow-up education focused on prevention strategies.
Case Study 2: Ascites-Related Distension
Mr. Johnson, 58-year-old male with liver cirrhosis
Presentation: Mr. Johnson presents with progressive abdominal distension over two weeks, accompanied by weight gain of 3.5 kg and mild shortness of breath. He reports non-compliance with sodium restriction and diuretic medication.
Assessment Findings: Marked abdominal distension with fluid wave sign, shifting dullness on percussion, abdominal girth 104 cm (baseline 94 cm), respiratory rate 24/min.
Nursing Interventions:
- Position in semi-Fowler’s to ease breathing
- Reinforce importance of medication adherence
- Provide detailed sodium restriction education with culturally appropriate food options
- Implement daily weight and abdominal girth monitoring
- Coordinate with primary physician regarding need for paracentesis
- Arrange for home health monitoring
Outcome: Mr. Johnson required referral for paracentesis due to respiratory compromise. Following the procedure and with improved medication adherence, his abdominal distension gradually decreased. Community health nurse continued weekly monitoring and reinforcement of dietary compliance.
Case Study 3: IBS-Related Distension
Ms. Rivera, 32-year-old female with irritable bowel syndrome
Presentation: Ms. Rivera reports cyclical abdominal distension that worsens throughout the day and with certain foods. She experiences bloating, cramping pain, and alternating constipation and diarrhea. Recent stress at work has exacerbated her symptoms.
Assessment Findings: Moderate abdominal distension that is soft and non-tender, normal bowel sounds, no alarm signs.
Nursing Interventions:
- Initiate food diary to identify trigger foods
- Educate on low-FODMAP diet principles with practical meal planning
- Teach stress reduction techniques including diaphragmatic breathing
- Coordinate referral to dietitian for comprehensive dietary guidance
- Provide resources for IBS support group
- Develop regular exercise plan
Outcome: After six weeks of dietary modification and stress management techniques, Ms. Rivera reported 70% reduction in distension episodes. She identified specific trigger foods and successfully implemented dietary changes. Continued community health nurse support focused on stress management techniques.
Case Analysis Points:
These cases illustrate the importance of identifying the underlying cause of abdominal distension, tailoring interventions to the specific cause, and providing appropriate education and support. Community health nurses must develop comprehensive care plans that address not only the physical symptoms but also the psychosocial aspects of living with conditions that cause abdominal distension.
References
- NCBI Bookshelf. (n.d.). Chapter 12 Abdominal Assessment – Nursing Skills. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK593213/
- SAEMS Council. (2009). ABDOMINAL PAIN STANDING ORDER. Retrieved from http://saemscouncil.com/wp-content/uploads/2014/12/AbdominalPainSLP109a.pdf
- Vaia. (2023). Abdominal Distention: Causes, Bloating & Diarrhoea – Nursing. Retrieved from https://www.vaia.com/en-us/explanations/nursing/human-anatomy/abdominal-distention/
- Nursipedia. (n.d.). Nursing care plan for abdominal distention. Retrieved from https://nursipedia.com/nursing-care-plan-abdominal-distention/
- NCBI/PMC. (2016). Management Strategies for Abdominal Bloating and Distension. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC4991532/
- Cleveland Clinic. (n.d.). Abdominal Distension (Distended Abdomen). Retrieved from https://my.clevelandclinic.org/health/symptoms/21819-abdominal-distension-distended-abdomen
- American Red Cross. (n.d.). Abdominal Injury – First Aid. Retrieved from https://www.redcross.org/take-a-class/resources/learn-first-aid/abdominal-injury
- Nursing.com. (n.d.). Nursing Care Plan (NCP) for Abdominal Pain. Retrieved from https://nursing.com/lesson/nursing-care-plan-for-abdominal-pain
