Management of Common Eye & ENT Conditions
A Comprehensive Guide for Community Health Nursing
This guide provides essential information for community health nurses on screening, diagnosing, managing, and referring common eye and ENT conditions.
Table of Contents
Introduction to Community Screening for Eye & ENT Conditions
Eye and Ear, Nose, and Throat (ENT) conditions represent some of the most common health issues encountered in community settings. These conditions can significantly impact quality of life and, if left untreated, may lead to serious complications including permanent vision or hearing loss. Community health nurses play a pivotal role in early detection, management, and referral of these conditions.
Effective community screening programs for eye and ENT conditions help identify health issues at early stages when interventions are most effective. These programs are particularly important in underserved areas where access to specialized healthcare may be limited. By implementing standardized screening protocols, community health nurses can significantly improve health outcomes for their populations.
This guide provides comprehensive information on common eye and ENT conditions, including their identification, primary care management, and appropriate referral pathways. It also outlines standing orders and first aid measures that community health nurses can implement in various settings.
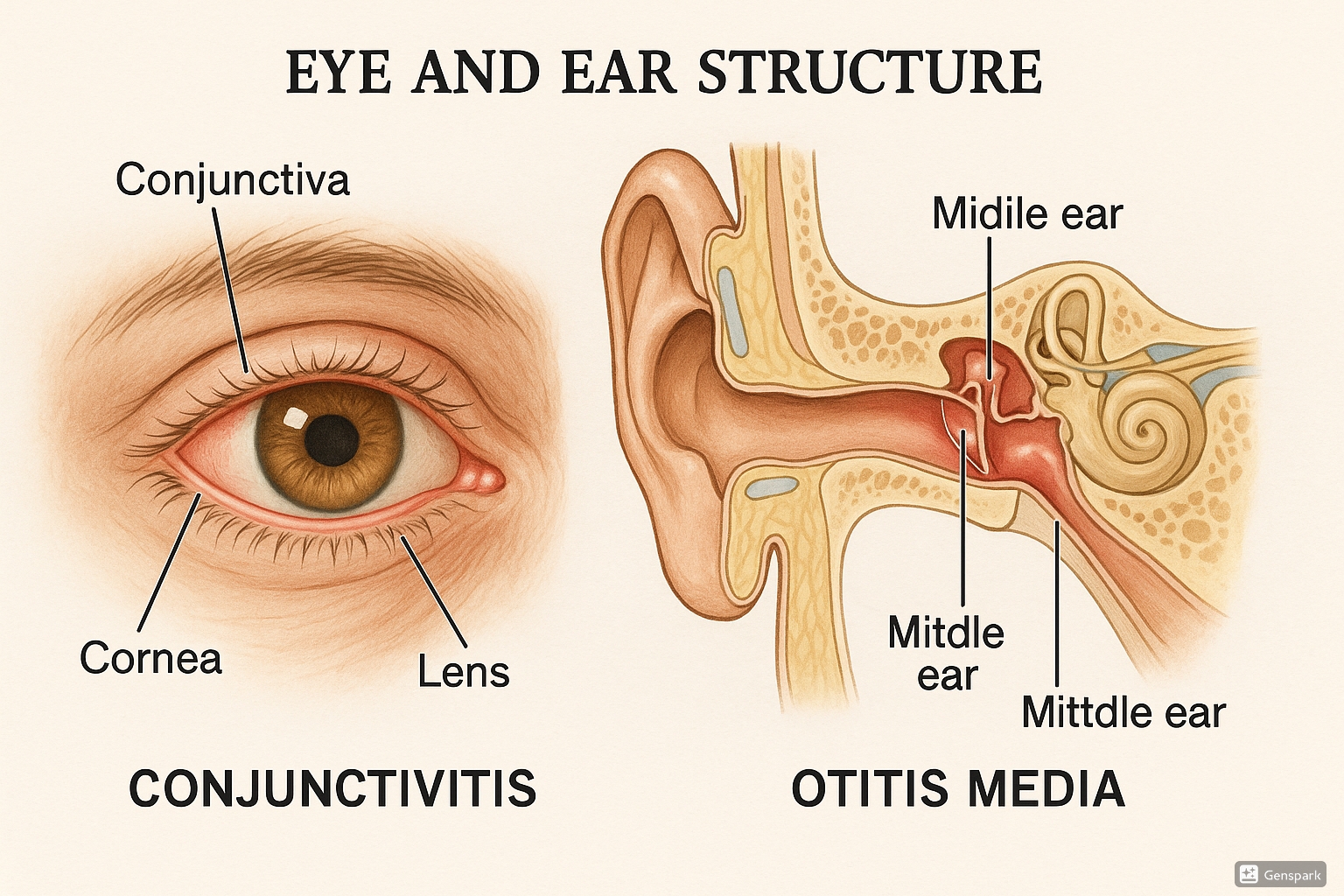
Anatomical illustration of eye and ear structures, highlighting areas commonly affected by conditions discussed in this guide.
Standing Orders: Definition and Uses
Definition
Standing orders are written protocols approved by a qualified healthcare provider that authorize nurses and other appropriate healthcare staff to provide specific services or interventions without direct physician supervision at the time of service.
Key Components of Standing Orders
Effective standing orders should include:
- Specific conditions or symptoms that trigger the order
- Detailed protocols for assessment
- Clear intervention guidelines
- Medication administration protocols (if applicable)
- Documentation requirements
- Criteria for physician notification or patient referral
Uses in Community Health Nursing
Standing orders for eye and ENT conditions serve several important purposes in community health settings:
| Purpose | Application in Community Screening |
|---|---|
| Standardization of Care | Ensures consistent assessment and treatment approaches across different community health workers |
| Timely Intervention | Allows immediate initiation of appropriate treatment for common conditions |
| Resource Optimization | Maximizes the scope of practice for community health nurses while preserving physician time for complex cases |
| Care Accessibility | Expands healthcare access in underserved areas where physician availability may be limited |
| Quality Control | Provides a framework for maintaining consistent quality standards in community health services |
Standing orders particularly enhance community screening programs by allowing community health nurses to independently assess, provide initial treatment, and make appropriate referral decisions for common eye and ENT conditions.
Screening and Identification Methods
Effective community screening relies on systematic approaches to identify eye and ENT conditions at early stages. The following tools and techniques are essential components of a comprehensive screening program:
Vision Screening Tools
| Screening Tool | Application | Procedure | Interpretation |
|---|---|---|---|
| Snellen Chart | Distance vision assessment | Patient stands 20 feet (6 meters) from chart and reads smallest visible line | Normal vision: 20/20 (6/6); Values like 20/40 indicate individual can see at 20 feet what a person with normal vision sees at 40 feet |
| Near Vision Chart | Reading and close-work vision assessment | Patient holds chart at 14-16 inches (35-40 cm) and reads smallest visible text | Normal near vision correlates with age; presbyopia common after age 40 |
| Ishihara Plates | Color vision testing | Patient identifies numbers or patterns within colored dots | Inability to identify patterns suggests color vision deficiency |
| Penlight Examination | Basic eye structure assessment | External examination of eye structures and pupillary response | Abnormalities in external structures or pupillary response require further evaluation |
ENT Screening Tools
| Screening Tool | Application | Procedure | Interpretation |
|---|---|---|---|
| Otoscope | Ear canal and tympanic membrane examination | Visualize ear canal and tympanic membrane with otoscope | Normal TM: pearly gray, transparent, intact; Abnormalities include redness, bulging, retraction, or perforation |
| Whispered Voice Test | Basic hearing assessment | Examiner whispers words at arm’s length behind patient; patient repeats words | Inability to repeat correctly suggests hearing impairment |
| Tuning Fork Tests (Rinne and Weber) | Differentiation between conductive and sensorineural hearing loss |
Rinne: Compare air and bone conduction Weber: Tuning fork placed on midline of forehead |
Rinne: Normal = air conduction > bone conduction Weber: Normal = sound heard equally in both ears |
| Throat Examination | Assessment of oropharynx | Visual inspection with penlight and tongue depressor | Observe for redness, swelling, exudates, or structural abnormalities |
Comprehensive Screening Approach
An effective community screening program integrates multiple assessment components:
1. History Taking
- Chief complaint and duration
- Associated symptoms
- Previous episodes and treatments
- Family history
- Environmental and occupational factors
2. Physical Examination
- Systematic assessment using appropriate tools
- Documentation of findings
- Comparison with normal parameters
- Assessment of impact on daily functioning
3. Risk Factor Assessment
- Age-related factors
- Comorbid conditions
- Lifestyle factors
- Environmental exposures
4. Documentation and Referral
- Standardized recording of findings
- Decision-making based on protocols
- Clear communication of findings
- Appropriate follow-up planning
Mnemonic: “SCREEN” for Community Screening Process
- S – Systematic assessment using standardized tools
- C – Collect comprehensive history
- R – Record findings accurately
- E – Evaluate against normal parameters
- E – Educate patient about findings
- N – Navigate to appropriate care level (treat or refer)
Common Eye Conditions
Community health nurses frequently encounter various eye conditions during community screening activities. Understanding their presentation, management, and referral criteria is essential for effective primary care.
Local Infections
Local eye infections involve inflammation of various external eye structures and are commonly encountered during community screening.
| Type | Clinical Features | Primary Care Management | Referral Criteria |
|---|---|---|---|
| Blepharitis (eyelid infection) |
|
|
|
| Hordeolum (external stye) |
|
|
|
| Dacryocystitis (lacrimal sac infection) |
|
|
|
Important Note:
Local eye infections may be contagious. Educate patients about proper hand hygiene, avoiding sharing of towels and makeup, and refraining from touching or rubbing eyes.
Redness of Eye
Red eye is a common presentation in community screening settings and can indicate various underlying conditions from minor irritation to serious ocular emergencies.
Differential Diagnosis of Red Eye
| Condition | Pattern of Redness | Associated Symptoms | Primary Care Management | Urgency Level |
|---|---|---|---|---|
| Conjunctivitis | Diffuse, more pronounced in fornices | Discharge, grittiness, mild discomfort | See conjunctivitis section | Non-urgent |
| Subconjunctival Hemorrhage | Bright red, well-demarcated patch | Usually asymptomatic, no pain or vision changes | Reassurance, check BP, investigate if recurrent | Non-urgent |
| Acute Glaucoma | Ciliary flush (redness around iris) | Severe pain, blurred vision, halos around lights, nausea | Immediate referral | Emergency |
| Iritis/Uveitis | Ciliary flush | Photophobia, pain, small pupil, blurred vision | Urgent referral | Urgent |
| Foreign Body | Localized redness | Pain, foreign body sensation, tearing | Irrigation if visible and loosely adhering; otherwise refer | Semi-urgent |
| Corneal Abrasion | Localized or diffuse | Pain, photophobia, foreign body sensation | Referral for fluorescein staining and treatment | Semi-urgent |
Mnemonic: “REDNESS” for Assessing Red Eye
- R – Redness pattern (diffuse or localized)
- E – Exudate or discharge (type and amount)
- D – Discomfort level (mild to severe)
- N – Neurological symptoms (headache, nausea)
- E – Eye structures involved (conjunctiva, cornea, etc.)
- S – Systemic symptoms (fever, malaise)
- S – Sight affected (visual acuity changes)
Warning Signs Requiring Immediate Referral:
- Severe pain
- Vision loss or significant blurring
- Halos around lights
- Associated nausea/vomiting
- Pupil abnormalities
- History of trauma or chemical exposure
Conjunctivitis
Conjunctivitis (pink eye) is a common eye condition frequently identified during community screening. It involves inflammation of the conjunctiva, the thin transparent layer covering the white of the eye and inner eyelid.
Types of Conjunctivitis
| Type | Causes | Clinical Features | Management |
|---|---|---|---|
| Bacterial Conjunctivitis |
|
|
|
| Viral Conjunctivitis |
|
|
|
| Allergic Conjunctivitis |
|
|
|
Prevention and Education
Community health nurses should educate patients on:
- Proper hand hygiene
- Avoiding eye touching and sharing of personal items
- Proper application of eye medications
- Isolation measures for infectious conjunctivitis
- When to seek further medical attention
Conjunctivitis in Schools and Community Settings
Conjunctivitis can spread rapidly in community settings. Community screening programs should include protocols for identifying potential outbreaks and implementing control measures. Children with bacterial or viral conjunctivitis should avoid school until 24 hours after beginning treatment or until no longer contagious.
Stye (Hordeolum)
A stye is an acute infection of the oil glands of the eyelid that presents as a painful, localized swelling. During community screening, styes are commonly identified conditions that can typically be managed with primary care interventions.
Types of Styes
- External Hordeolum: Infection of the sebaceous (Zeis) glands or sweat (Moll) glands at the eyelid margin
- Internal Hordeolum: Infection of the meibomian glands within the tarsal plate of the eyelid
Causes
- Bacterial infection (usually Staphylococcus aureus)
- Blocked oil glands
- Poor eyelid hygiene
- Underlying blepharitis
- Use of contaminated cosmetics
Clinical Features
- Painful, red, localized swelling on eyelid margin or within eyelid
- Tenderness to touch
- May develop a yellowish spot at the center (pointing)
- Tearing and mild photophobia
- Foreign body sensation
- Usually unilateral
Management
Primary Care
- Warm compresses for 10-15 minutes, 4-6 times daily
- Gentle massage to promote drainage (once pointing appears)
- Analgesics for pain relief
- Proper eyelid hygiene instruction
Medication (per standing orders)
- Topical antibiotic ointment (erythromycin or bacitracin) for external styes
- Oral antibiotics rarely needed unless cellulitis develops
- Avoid eye makeup until resolved
Referral Criteria
- No improvement after 48 hours of treatment
- Spreading redness or cellulitis
- Recurrent styes
- Internal hordeolum not responding to treatment
- Visual changes
Important:
Patients should be advised never to squeeze or attempt to drain a stye manually, as this can spread the infection and potentially cause serious complications.
Prevention
During community screening, educate patients on preventive measures:
- Good hand hygiene before touching eyes
- Proper eyelid cleansing for those with oily skin or blepharitis
- Regular replacement of eye makeup (every 3-6 months)
- Never sharing eye makeup
- Removing eye makeup before sleeping
Trachoma
Trachoma is a chronic contagious eye infection caused by Chlamydia trachomatis. It remains the leading infectious cause of blindness worldwide and is a critical target for community screening programs in endemic areas.
Public Health Significance
Trachoma is prevalent in areas with poor sanitation, limited access to clean water, and overcrowded living conditions. Effective community screening and early intervention can significantly reduce the burden of trachoma-related blindness.
Etiology and Transmission
- Causative agent: Chlamydia trachomatis (serotypes A, B, Ba, and C)
- Transmission: Direct contact with eye and nose discharges of infected persons
- Indirect transmission: Via contaminated towels, clothing, or flies
- Risk factors: Poor personal hygiene, limited water access, overcrowding
Clinical Stages (WHO Simplified Grading System)
| Stage | Description | Clinical Features | Management |
|---|---|---|---|
| Trachomatous Inflammation – Follicular (TF) | Early active infection |
|
|
| Trachomatous Inflammation – Intense (TI) | More severe inflammation |
|
|
| Trachomatous Scarring (TS) | Cicatricial stage |
|
|
| Trachomatous Trichiasis (TT) | Inturned eyelashes |
|
|
| Corneal Opacity (CO) | End-stage disease |
|
|
Community Screening and Management Strategy: SAFE
S – Surgery
For advanced cases with trichiasis to prevent corneal damage and blindness
A – Antibiotics
Mass treatment in endemic communities or individual treatment for active cases
F – Facial cleanliness
Promotion of face washing to reduce transmission
E – Environmental improvements
Access to clean water, sanitation, and reducing fly breeding sites
Role of Community Health Nurses
- Conduct regular community screening in endemic areas using simplified grading system
- Identify and treat active cases according to standing orders
- Refer advanced cases for surgical management
- Implement health education regarding facial hygiene and environmental factors
- Coordinate with public health authorities for community-wide interventions
- Follow up treated cases to assess response and prevent recurrence
Refractive Errors
Refractive errors are common vision problems that occur when the shape of the eye prevents light from focusing correctly on the retina. Community screening for refractive errors is essential for early detection and intervention, particularly in school-aged children and older adults.
Types of Refractive Errors
| Type | Description | Clinical Features | Screening Methods | Management |
|---|---|---|---|---|
| Myopia (Nearsightedness) | Distant objects appear blurry while near objects remain clear |
|
|
|
| Hyperopia (Farsightedness) | Near objects appear blurry while distant objects may be clearer |
|
|
|
| Astigmatism | Irregular curvature of cornea or lens causing distorted vision |
|
|
|
| Presbyopia | Age-related loss of near focusing ability |
|
|
|
Community Screening Approaches
School-Based Screening
- Annual visual acuity testing using age-appropriate charts
- Assessment of eye alignment and movement
- Screening for color vision deficiencies (usually grades 1-2)
- Documentation and referral system for failed screenings
- Follow-up mechanism to ensure compliance with referrals
Adult Screening (40+ years)
- Distance visual acuity testing
- Near vision assessment for presbyopia
- Basic ocular health screening
- Glaucoma risk assessment
- Education about age-related vision changes
- Referral protocols for comprehensive eye examinations
Mnemonic: “VISION” for Refractive Error Screening
- V – Visual acuity measurement (distance and near)
- I – Identify risk factors (family history, age, symptoms)
- S – Screen using appropriate tools (Snellen, near cards)
- I – Interview for symptoms (headaches, eye strain, squinting)
- O – Observe behavior (reading distance, head tilting)
- N – Note findings and make appropriate referrals
Importance in Community Health
Uncorrected refractive errors can have significant impacts on:
- Educational achievement in children
- Occupational performance in adults
- Quality of life in older adults
- Safety (e.g., driving, preventing falls)
- Psychosocial well-being
Community Health Nurse’s Role
Community health nurses should advocate for regular vision screening across the lifespan, educate communities about the importance of eye care, and facilitate access to vision correction resources, especially for underserved populations.
Common ENT Conditions
Ear, Nose, and Throat (ENT) conditions are frequently encountered during community screening activities. Community health nurses must be proficient in assessing, managing, and making appropriate referrals for these conditions.
Epistaxis (Nosebleed)
Epistaxis refers to acute hemorrhage from the nostril, nasal cavity, or nasopharynx. It is a common emergency encountered during community screening and requires prompt assessment and management.
Classification
- Anterior Epistaxis (90-95%): Bleeding from Kiesselbach’s plexus in the anterior nasal septum
- Posterior Epistaxis (5-10%): Bleeding from posterior nasal cavity, often from branches of sphenopalatine artery
Etiology
- Local Causes: Trauma, foreign body, nose picking, digital trauma, mucosal dryness, septal deviation
- Systemic Causes: Hypertension, anticoagulant therapy, coagulopathies, liver disease, alcohol use
- Other Factors: Environmental (dry climate, high altitude), allergic rhinitis, upper respiratory infections
Assessment
| Parameter | Assessment Focus | Significance |
|---|---|---|
| Bleeding Source | Anterior vs. posterior | Determines management approach and urgency |
| Bleeding Severity | Volume, duration, recurrence | Indicates need for emergency referral |
| Vital Signs | BP, pulse, respiratory rate | Assesses hemodynamic stability |
| Medical History | Hypertension, bleeding disorders, medications | Identifies contributing factors |
| Examination | Nasal cavity, throat for posterior bleeding | Localizes bleeding source |
Management of Anterior Epistaxis
First Aid Measures
- Position patient upright with head tilted slightly forward
- Apply firm pressure to the fleshy part of the nose for 10-15 minutes continuously
- Use ice pack or cold compress on the bridge of the nose
- Instruct patient to breathe through mouth and avoid swallowing blood
Advanced Measures (per standing orders)
- Inspect nasal cavity with good light source
- Apply cotton with vasoconstrictor agent (e.g., oxymetazoline)
- Consider chemical cautery with silver nitrate if bleeding point visible
- Anterior nasal packing if bleeding continues
Referral Criteria
- Bleeding not controlled with first aid measures
- Suspected posterior bleeding
- Significant blood loss or hemodynamic instability
- Patient on anticoagulants
- Recurrent epistaxis
Warning Signs Requiring Immediate Referral:
- Bleeding not controlled after 20 minutes of pressure
- Blood flowing down throat (posterior bleeding)
- Signs of significant blood loss (pallor, dizziness, tachycardia)
- Respiratory distress
- Known bleeding disorder or anticoagulant therapy
Patient Education
During community screening and after epistaxis management, education should include:
- Avoiding nose picking, forceful nose blowing, and strenuous activity for 24 hours
- Keeping head elevated when resting
- Using saline nasal spray or water-soluble lubricant to prevent nasal dryness
- Humidifying the home environment
- When to seek medical attention for recurrent episodes
- Importance of blood pressure monitoring for hypertensive patients
Acute Suppurative Otitis Media (ASOM)
Acute Suppurative Otitis Media (ASOM) is an infection of the middle ear characterized by rapid onset of signs and symptoms of infection with middle ear effusion. It is commonly identified during community screening, especially in pediatric populations.
Etiology and Risk Factors
Common Pathogens
- Streptococcus pneumoniae (30-40%)
- Haemophilus influenzae (20-30%)
- Moraxella catarrhalis (10-15%)
- Group A Streptococcus (5%)
- Viruses (Respiratory Syncytial Virus, Rhinovirus)
Risk Factors
- Young age (peak incidence 6-18 months)
- Eustachian tube dysfunction
- Upper respiratory infections
- Daycare attendance
- Passive smoke exposure
- Bottle feeding while lying down
- Craniofacial abnormalities
- Immunodeficiency
Clinical Stages of ASOM
| Stage | Pathophysiology | Clinical Features | Otoscopic Findings |
|---|---|---|---|
| Stage 1: Tubal Occlusion | Eustachian tube dysfunction with negative middle ear pressure | Ear fullness, popping, mild discomfort, mild hearing loss | Retracted tympanic membrane (TM), prominent landmarks, amber color |
| Stage 2: Hydrops | Sterile effusion in middle ear | Increased pressure sensation, increased hearing loss | Retracted TM, fluid level or bubbles visible, decreased mobility |
| Stage 3: Suppuration | Bacterial infection of middle ear fluid | Ear pain, fever, irritability, hearing loss, possible systemic symptoms | Bulging, erythematous TM, obscured landmarks, decreased mobility |
| Stage 4: Resolution or Complications | Spontaneous resolution or progression to complications | Pain reduction or worsening with complications | TM perforation with discharge or progression of inflammatory signs |
Mnemonic: “ASOM” for ASOM Assessment
- A – Appearance of tympanic membrane (color, position, landmarks)
- S – Symptoms (pain, fever, hearing loss, irritability)
- O – Otorrhea (presence and characteristics if present)
- M – Mobility of tympanic membrane (using pneumatic otoscopy)
Management
Primary Care (per standing orders)
- Pain Management:
- Acetaminophen or ibuprofen for pain and fever
- Topical analgesics (if TM intact)
- Antibiotics:
- First-line: Amoxicillin (80-90 mg/kg/day in divided doses)
- Alternative: Amoxicillin-clavulanate for treatment failure or high-risk
- Supportive Care:
- Adequate hydration
- Elevated head position
Referral Criteria
- Age less than 3 months
- Severe symptoms or toxic appearance
- Immunocompromised status
- Complications suspected:
- Mastoiditis (swelling/tenderness behind ear)
- Facial nerve paralysis
- Meningeal signs
- Labyrinthitis (vertigo, nystagmus)
- Recurrent ASOM (3+ episodes in 6 months)
- Persistent effusion > 3 months
Watchful Waiting vs. Immediate Antibiotics
Current guidelines allow for observation without antibiotics in select cases:
| Age Group | Severity | Recommendation |
|---|---|---|
| 6 months to 2 years | Unilateral, mild-moderate symptoms | Observation option if reliable follow-up |
| 6 months to 2 years | Bilateral or severe symptoms | Immediate antibiotics |
| ≥ 2 years | Mild to moderate symptoms | Observation option with adequate follow-up |
| ≥ 2 years | Severe symptoms | Immediate antibiotics |
Follow-up for ASOM
During community screening programs, establish follow-up protocols:
- For observation approach: Follow-up in 48-72 hours
- For antibiotic treatment: Follow-up if no improvement in 48-72 hours
- Routine follow-up in 4-6 weeks to ensure resolution of effusion
- Hearing assessment for children with persistent effusion
Prevention Strategies
- Pneumococcal vaccination
- Annual influenza vaccination
- Breastfeeding for at least 6 months
- Avoiding bottle-feeding in supine position
- Eliminating passive smoke exposure
- Proper hand hygiene to reduce URI transmission
Sore Throat
Sore throat (pharyngitis) is a common complaint encountered during community screening activities. Accurate assessment and differentiation between viral and bacterial causes are essential for appropriate management.
Etiology
Viral (70-85%)
- Rhinovirus
- Coronavirus
- Adenovirus
- Epstein-Barr virus (mononucleosis)
- Influenza virus
- Parainfluenza virus
Bacterial (15-30%)
- Group A Streptococcus (most common)
- Group C and G Streptococcus
- Neisseria gonorrhoeae
- Mycoplasma pneumoniae
- Chlamydia pneumoniae
- Corynebacterium diphtheriae (rare)
Non-Infectious
- Allergic rhinitis with post-nasal drip
- Gastroesophageal reflux disease
- Environmental irritants
- Trauma
- Excessive voice use
- Dry air
Clinical Assessment
| Feature | Viral Pharyngitis | Streptococcal Pharyngitis |
|---|---|---|
| Onset | Gradual | Sudden |
| Age Group | Any age | Primarily 5-15 years |
| Season | Year-round, peaks in winter | Winter and early spring |
| Throat Appearance | Mild to moderate erythema, patchy exudates possible | Intense erythema, tonsillar exudates, petechiae on palate |
| Lymph Nodes | Variable, usually minimal enlargement | Tender anterior cervical lymphadenopathy |
| Temperature | Low-grade fever or none | Fever >38°C (100.4°F) |
| Cough | Common | Uncommon |
| Rhinorrhea | Common | Uncommon |
| Headache | Variable | Common |
| Abdominal Pain | Uncommon | Common in children |
| Rash | Variable (depends on virus) | Scarlatiniform rash (scarlet fever) in some cases |
Diagnostic Tools for Community Screening
Clinical Decision Rules: Centor/McIsaac Criteria
One point each for:
- Tonsillar exudates
- Tender anterior cervical lymphadenopathy
- Absence of cough
- History of fever (>38°C/100.4°F)
- Age 3-14 years (+1 point) or Age 15-44 years (0 points) or Age ≥45 years (-1 point)
Score Interpretation:
- 0-1: No testing or antibiotics
- 2-3: Test and treat if positive
- 4-5: Consider empiric treatment or test and treat
Rapid Strep Test (RST)
Procedure:
- Visualize posterior pharynx with adequate light
- Swab both tonsillar pillars and posterior pharynx
- Avoid touching tongue, uvula, or buccal mucosa
- Process according to test kit instructions
Interpretation:
- Sensitivity: 70-90%
- Specificity: 95-100%
- Positive result: Treat with antibiotics
- Negative result: Consider throat culture in high-risk patients
Management
Viral Pharyngitis
- Symptomatic Treatment:
- Adequate hydration
- Acetaminophen or ibuprofen for pain and fever
- Warm salt water gargles
- Throat lozenges (for ages >4 years)
- Cool mist humidifier
- Education:
- Expected course (5-7 days)
- No antibiotics needed
- Return if worsening symptoms
Streptococcal Pharyngitis (per standing orders)
- Antibiotic Options:
- First-line: Penicillin V (children: 250mg BID-TID; adults: 500mg BID) for 10 days
- Alternative: Amoxicillin (50mg/kg/day, max 1000mg) once daily for 10 days
- Penicillin-allergic: Cephalexin (non-anaphylactic) or clindamycin/macrolide (anaphylactic)
- Symptomatic treatment as for viral pharyngitis
- Follow-up:
- If symptoms persist >48 hours after antibiotics
- For recurrent streptococcal infections
Warning Signs Requiring Immediate Referral:
- Difficulty breathing or swallowing
- Drooling or inability to handle secretions
- Stridor or voice changes
- Severe throat pain with minimal visible inflammation
- Unilateral peritonsillar swelling (possible abscess)
- Trismus (difficulty opening mouth)
- Toxic appearance
- Immunocompromised status
Prevention in Community Settings
- Hand hygiene education
- Respiratory etiquette (covering coughs and sneezes)
- Avoiding sharing of utensils and drinks
- Proper disposal of tissues
- Staying home when ill with fever and sore throat
- Completing full course of antibiotics if prescribed
Deafness
Hearing loss or deafness is a significant health concern that affects individuals across the lifespan. Community screening for hearing impairment is essential for early identification and intervention, especially in vulnerable populations.
Classification of Hearing Loss
| Type | Mechanism | Common Causes | Characteristics | Screening Identification |
|---|---|---|---|---|
| Conductive Hearing Loss | Disruption in transmission of sound through outer or middle ear |
|
|
|
| Sensorineural Hearing Loss | Damage to inner ear (cochlea) or auditory nerve pathways |
|
|
|
| Mixed Hearing Loss | Combination of conductive and sensorineural components |
|
|
|
Degrees of Hearing Loss
| Degree | Hearing Level (dB HL) | Functional Impact |
|---|---|---|
| Normal | -10 to 15 dB | No significant difficulty |
| Slight | 16 to 25 dB | Difficulty with faint speech, subtle communication issues |
| Mild | 26 to 40 dB | Difficulty with soft speech, especially in noise |
| Moderate | 41 to 55 dB | Difficulty with conversation speech; benefits from hearing aids |
| Moderately Severe | 56 to 70 dB | Misses most conversational speech without amplification |
| Severe | 71 to 90 dB | Cannot hear conversational speech; requires powerful amplification |
| Profound | 91+ dB | Cannot rely on hearing as primary modality; may use sign language |
Community Screening Approaches
Infants and Young Children
- Newborn Screening: Otoacoustic emissions (OAE) or Automated Auditory Brainstem Response (AABR)
- Risk Assessment: History of risk factors
- Developmental Milestones: Speech and language monitoring
- Symptom Surveillance: Parent/caregiver concerns
- Visual Reinforcement Audiometry: For children 6 months to 2 years
School-Age Children
- Pure Tone Audiometry: At 1000, 2000, and 4000 Hz
- Tympanometry: To assess middle ear function
- Otoscopic Examination: For structural abnormalities
- Academic Performance: Assessment for potential relation to hearing
- High-Risk Screening: Children with recurrent ear infections, learning difficulties, or speech delays
Adults and Elderly
- Whispered Voice Test: Simple screening in primary care
- Questionnaires: Hearing Handicap Inventory for Adults/Elderly
- Pure Tone Audiometry: For quantitative assessment
- Risk Factor Assessment: Occupational noise, family history, medications
- Targeted Screening: For those with diabetes, cardiovascular disease, or cognitive concerns
Basic Hearing Assessment Techniques for Community Screening
Whispered Voice Test
- Stand arm’s length (0.6 m) behind the patient, out of view
- Mask the non-test ear by gently occluding the canal and rubbing the tragus
- Exhale fully before whispering to ensure consistent soft volume
- Whisper a combination of numbers and letters (e.g., “4-K-2”)
- Ask patient to repeat what they heard
- Test is passed if patient correctly repeats at least 50% of items
- Repeat with other ear
Tuning Fork Tests
Weber Test:
- Strike tuning fork (512 Hz) gently and place on midline of forehead
- Ask patient where sound is heard (midline, left, or right)
- Normal: Sound heard equally in both ears
- Conductive loss: Sound lateralizes to affected ear
- Sensorineural loss: Sound lateralizes to unaffected ear
Rinne Test:
- Strike tuning fork and place on mastoid process (bone conduction)
- When patient no longer hears, move to in front of ear canal (air conduction)
- Ask if patient can still hear the sound
- Normal or sensorineural loss: Air conduction > bone conduction
- Conductive loss: Bone conduction > air conduction
Management and Referral
| Condition | Primary Care Management | Referral Criteria |
|---|---|---|
| Cerumen Impaction |
|
|
| Otitis Media with Effusion |
|
|
| Sensorineural Hearing Loss |
|
|
| Age-Related Hearing Loss |
|
|
Mnemonic: “HEARING” for Community Screening
- H – History of risk factors and symptoms
- E – Examine ear structures with otoscope
- A – Assess hearing with appropriate screening tools
- R – Recognize early signs of hearing loss
- I – Intervene with primary care measures when appropriate
- N – Navigate patient to appropriate specialists when needed
- G – Guide patients on communication strategies and prevention
Prevention and Education
During community screening activities, provide education on:
- Noise protection in occupational and recreational settings
- Signs and symptoms requiring medical attention
- Avoidance of inserting objects into ears
- Appropriate use and care of hearing aids
- Communication strategies for those with hearing loss
- Available community resources for hearing-impaired individuals
- Importance of regular hearing screening across the lifespan
First Aid and Emergency Management
Community health nurses must be prepared to provide first aid for eye and ENT emergencies during community screening activities or in other community settings. Prompt and appropriate first aid can prevent complications and preserve function.
Eye Emergencies
| Condition | First Aid Measures | Do Not | Follow-up Requirements |
|---|---|---|---|
| Chemical Exposure |
|
|
All chemical exposures require immediate medical evaluation after first aid |
| Foreign Body |
|
|
|
| Eye Trauma/Contusion |
|
|
All significant eye trauma requires immediate referral |
| Penetrating Injury |
|
|
Requires immediate emergency referral |
| Acute Visual Loss |
|
|
Requires immediate emergency referral |
ENT Emergencies
| Condition | First Aid Measures | Do Not | Follow-up Requirements |
|---|---|---|---|
| Epistaxis (Nosebleed) |
|
|
|
| Foreign Body in Ear |
|
|
|
| Foreign Body in Nose |
|
|
|
| Sudden Hearing Loss |
|
|
|
| Severe Throat Pain/Difficulty Swallowing |
|
|
|
Important First Aid Supplies for Eye and ENT Emergencies
Community health nurses conducting community screening should have access to:
- Sterile saline solution or eye wash
- Eye shields or paper cups
- Gauze pads and medical tape
- Penlight and magnifying glass
- Otoscope with various specula sizes
- Blunt-tipped tweezers
- Cotton-tipped applicators
- Ice packs or cold compresses
- Tuning forks (512 Hz)
- Basic analgesics (acetaminophen)
- Epinephrine auto-injector for allergic reactions
- Referral forms and emergency contact information
Primary Care and Referral Guidelines
A critical component of community screening programs for eye and ENT conditions is establishing clear guidelines for primary care management versus referral to specialized services. Community health nurses must be able to make appropriate decisions based on assessment findings.
General Principles for Referral Decision-Making
Urgency Assessment
- Emergency: Immediate threat to vision, hearing, or life
- Urgent: Needs specialist care within 24-48 hours
- Semi-urgent: Needs specialist care within 1-2 weeks
- Routine: Can be scheduled at next available appointment
Standing Order Considerations
- Is condition covered in standing orders?
- Do assessment findings match criteria for primary care management?
- Are there any exclusions or special considerations?
- Is patient in a high-risk category?
- Is follow-up assured?
