Crucial Nursing Skills: Master Rectal & Vaginal Drug Insertion for Optimal Patient Care
Comprehensive Guide for Nursing Students in India – Safe, Effective, and Patient-Centered Medication Administration
Table of Contents
Introduction to Drug Administration Routes
Rectal and vaginal drug administration represent crucial alternative routes when oral medication is not feasible or when local therapeutic effects are desired. These methods provide reliable absorption pathways while offering unique advantages in specific clinical scenarios. Understanding proper suppository insertion techniques and medication administration protocols is fundamental for nursing practice in India’s diverse healthcare settings.
Advantages of Rectal Route
- Bypasses hepatic first-pass metabolism
- Useful when oral route is contraindicated
- Rapid onset for emergency medications
- Suitable for unconscious patients
Advantages of Vaginal Route
- Direct local therapeutic action
- Minimal systemic absorption
- Excellent for gynecological conditions
- Convenient for hormone replacement
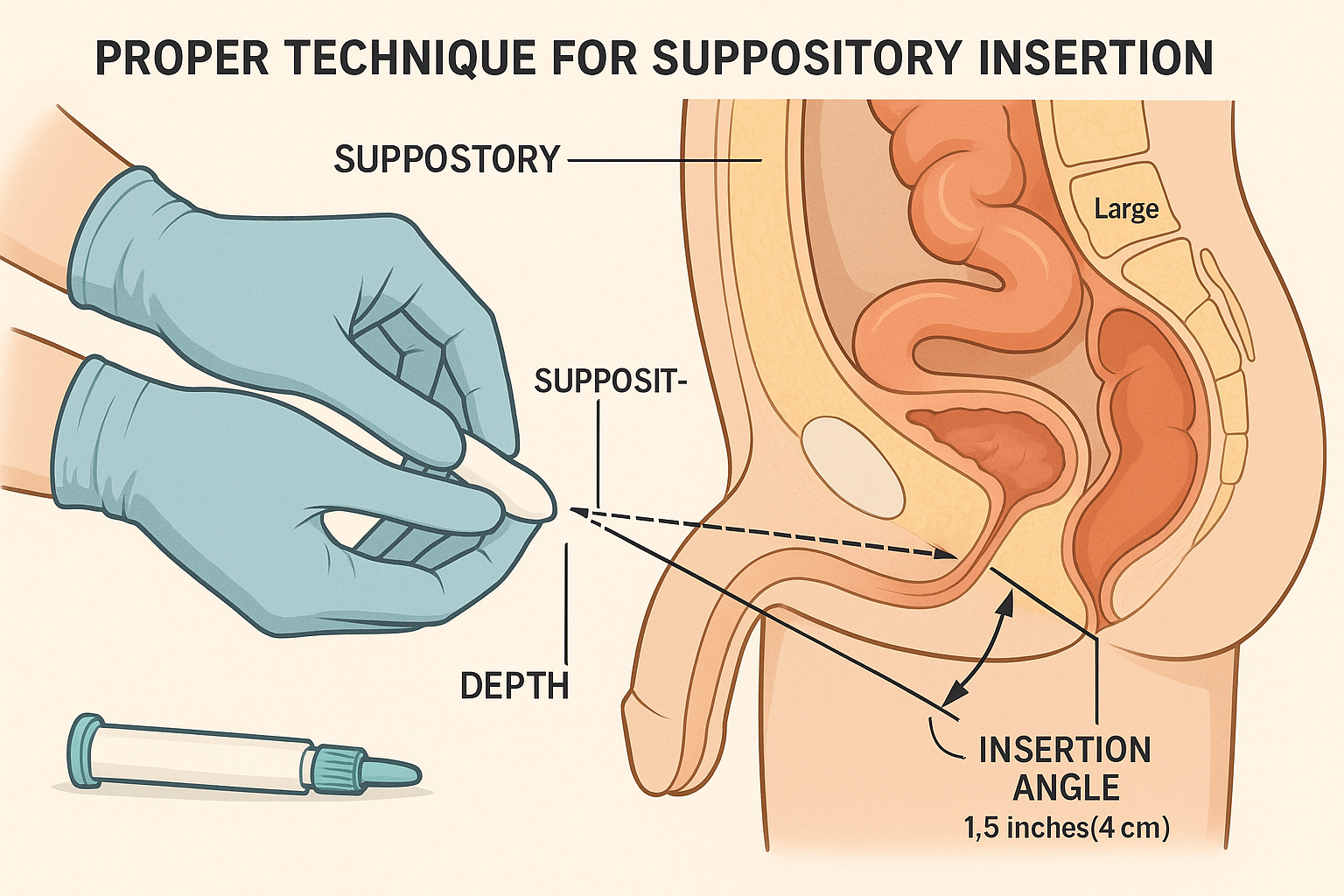
Professional demonstration of proper suppository insertion technique with anatomical guidance
Anatomical Considerations
Rectal Anatomy
Length: Approximately 12-15 cm in adults
Capacity: Can accommodate 20-30 ml of liquid medication
Blood Supply: Rich vascular network ensures rapid absorption
Nerve Supply: Sensitive anal canal requires gentle technique
Memory Aid: “RECTAL”
- R – Rich blood supply
- E – Easy absorption
- C – Comfortable position needed
- T – Temperature matters (body warmth)
- A – Angle of insertion important
- L – Lubrication essential
Vaginal Anatomy
Length: Approximately 8-12 cm in adults
pH Level: Acidic environment (3.8-4.5)
Elasticity: Highly distensible tissue
Absorption: Variable based on hormonal status
Memory Aid: “VAGINAL”
- V – Variable absorption rates
- A – Acidic environment
- G – Gentle insertion required
- I – Individual patient differences
- N – Natural lubrication varies
- A – Anatomical position matters
- L – Local effects predominant
Types of Medications and Formulations
| Medication Type | Rectal Route | Vaginal Route | Common Uses |
|---|---|---|---|
| Suppository | Solid dosage form that melts at body temperature | Bullet-shaped or oval for easy insertion | Pain relief, fever reduction, laxatives |
| Enemas | Liquid formulations for bowel preparation | Not applicable | Constipation, diagnostic procedures |
| Creams & Gels | Topical application for local effects | Hormonal treatments, antifungals | Local inflammation, infections |
| Tablets/Inserts | Less common, specialized formulations | Dissolve gradually for sustained release | Contraception, hormone therapy |
| Foams | Specialized applications | Easy application, patient comfort | Contraceptive, anti-inflammatory |
Storage Requirements
- • Most suppository medications stored at 15-25°C
- • Refrigeration may be required for some formulations
- • Protect from light and moisture
- • Check expiration dates regularly
Onset Times
- • Rectal suppository: 15-30 minutes
- • Vaginal medications: 30-60 minutes
- • Enemas: 5-15 minutes
- • Topical applications: Variable
Bioavailability
- • Rectal route: 50-80% systemic absorption
- • Vaginal route: 10-30% systemic absorption
- • Varies with patient factors
- • Local effects often primary goal
Safety Protocols & Infection Control
Universal Precautions
Hand Hygiene: Wash hands thoroughly before and after each procedure using antiseptic solution
Personal Protective Equipment: Use disposable gloves, gowns when necessary
Waste Disposal: Follow institutional protocols for medical waste management
Patient Safety Measures
Patient Identification: Verify patient identity using two identifiers
Allergy Assessment: Check for medication allergies and contraindications
Informed Consent: Explain procedure, obtain verbal consent
Critical Safety Alert
Never force suppository insertion. If resistance is encountered, stop the procedure and reassess. Forcing insertion can cause tissue trauma, bleeding, or perforation.
Pre-procedure Safety Checklist
Patient Assessment
- Verify patient identity
- Check medication orders
- Assess allergies
- Review contraindications
- Obtain consent
Equipment Preparation
- Gather supplies
- Check medication integrity
- Prepare lubricant
- Ensure privacy
- Position patient safely
Rectal Drug Administration Procedures
Suppository Insertion Technique
Step 1: Position
Left lateral position with knees flexed toward chest
Step 2: Prepare
Lubricate suppository and gloved finger
Step 3: Insert
Insert suppository past anal sphincter
Detailed Procedure Steps
Patient Preparation
Explain procedure to patient, ensure privacy with curtains or door closure. Position patient in left lateral (Sims) position with upper leg flexed. This position facilitates easy access and follows natural curve of rectum.
Hand Hygiene & Gloving
Perform thorough hand washing with antiseptic soap. Don non-sterile disposable gloves. Ensure suppository is at room temperature for easier insertion.
Suppository Preparation
Remove suppository from wrapper. Apply water-soluble lubricant to the tapered end and your gloved index finger. This reduces friction and patient discomfort during insertion.
Insertion Process
Gently separate buttocks with non-dominant hand. Insert suppository tapered end first, using index finger to push it approximately 7-10 cm (3-4 inches) into rectum, past the internal anal sphincter. This ensures proper retention and absorption.
Post-insertion Care
Withdraw finger gently. Encourage patient to remain lying down for 15-20 minutes to prevent expulsion. Provide tissues for patient comfort. Remove gloves and perform hand hygiene.
Professional Tips for Effective Suppository Administration
- • Temperature Matters: Cold suppository may be uncomfortable and difficult to insert
- • Timing: Best administered when patient has not had recent bowel movement
- • Patient Comfort: Use warm lubricant when possible to enhance comfort
- • Retention: Instruct patient to avoid bearing down or attempting bowel movement for at least 30 minutes
| Common Rectal Medications | Indication | Onset Time | Special Considerations |
|---|---|---|---|
| Paracetamol Suppository | Fever, pain relief | 30-60 minutes | Safe for children, hepatic metabolism |
| Diclofenac Suppository | Pain, inflammation | 15-30 minutes | Monitor for GI side effects |
| Glycerin Suppository | Constipation | 5-15 minutes | Osmotic laxative, safe for elderly |
| Ondansetron Suppository | Nausea, vomiting | 30-45 minutes | Useful when oral route compromised |
Vaginal Drug Administration Procedures
Cultural Sensitivity in Indian Healthcare Settings
Vaginal drug administration requires exceptional cultural sensitivity in Indian healthcare environments. Always ensure female nurse availability when possible, maintain strict privacy, explain procedures thoroughly, and respect patient preferences regarding gender of healthcare provider. Family involvement in decision-making should be considered while maintaining patient confidentiality.
Preparation Steps
Patient Assessment: Verify menstrual history, pregnancy status, and current symptoms
Privacy Assurance: Ensure complete privacy with proper draping and door closure
Medication Preparation: Bring medication to room temperature for comfort
Equipment Needed
- Prescribed vaginal medication
- Disposable gloves (non-sterile)
- Water-soluble lubricant
- Applicator (if required)
- Tissues and pad
- Proper draping materials
Step-by-Step Insertion Procedure
Patient Positioning
Position patient in dorsal recumbent position (supine with knees bent and feet flat) or left lateral position. Ensure proper draping to maintain dignity while allowing access. Some patients may prefer self-administration with guidance.
Hygiene and Gloving
Perform thorough hand hygiene and don non-sterile gloves. Inspect the medication for any damage or expiration. If using applicator, ensure it is clean and assembled properly according to manufacturer instructions.
Medication Preparation
For suppository: Apply small amount of water-soluble lubricant to tapered end. For creams/gels: Fill applicator according to prescribed dose. For tablets: May require slight moistening for easier insertion.
Insertion Technique
Gently separate labia with non-dominant hand. Insert medication into vaginal canal, directing towards the posterior fornix (back and down towards spine). For suppository, insert 7-10 cm deep. For applicator, insert according to manufacturer guidelines, usually 5-7 cm.
Post-Administration Care
Remove applicator gently if used. Provide tissues for patient comfort. Advise patient to remain lying down for 15-30 minutes to prevent medication leakage. Provide pantiliner or pad as medication may leak slightly.
Optimal Timing Considerations
- • Bedtime Administration: Reduces medication leakage and improves retention
- • Menstrual Cycle: Avoid during heavy menstrual flow unless specifically indicated
- • Post-void: Encourage urination before administration to improve comfort
- • Sexual Activity: Advise avoiding intercourse for duration specified by medication
Important Contraindications
- • Active Bleeding: Heavy menstrual or abnormal vaginal bleeding
- • Pregnancy Concerns: Verify pregnancy status for certain medications
- • Active Infections: Untreated pelvic infections may require different approach
- • Recent Surgery: Vaginal or pelvic surgery may contraindicate use
| Medication Type | Common Uses | Duration | Patient Instructions |
|---|---|---|---|
| Antifungal Suppository | Candidiasis, yeast infections | 3-7 days | Complete full course, avoid douching |
| Estrogen Cream | Postmenopausal atrophy | Ongoing therapy | Regular follow-up, monitor bleeding |
| Antibiotic Suppository | Bacterial vaginosis | 5-7 days | Avoid alcohol, complete course |
| Contraceptive Foam | Birth control | Before each intercourse | Insert before activity, remain supine |
Complications & Management
Rectal Administration Complications
Immediate Complications
- • Rectal bleeding: Stop procedure, assess severity, notify physician
- • Severe discomfort: Re-evaluate technique, consider alternative route
- • Medication expulsion: Wait 30 minutes before readministration
- • Allergic reaction: Monitor vital signs, prepare emergency treatment
Long-term Concerns
- • Tissue irritation: Rotate administration schedule if chronic use
- • Dependency issues: Monitor for laxative dependency with chronic use
- • Infection risk: Maintain strict aseptic technique
Vaginal Administration Complications
Immediate Complications
- • Vaginal irritation: Discontinue medication, assess for allergic reaction
- • Burning sensation: Normal initially, but monitor intensity
- • Excessive discharge: Differentiate between medication and infection
- • Insertion difficulty: Use adequate lubrication, consider patient positioning
Ongoing Monitoring
- • Secondary infections: Monitor for signs of secondary bacterial growth
- • Hormonal effects: Systemic absorption may cause hormonal changes
- • Partner effects: Advise regarding medication transfer during intimacy
Emergency Management Protocol
Severe Allergic Reaction
- Stop medication administration immediately
- Remove any remaining medication if possible
- Assess airway, breathing, circulation
- Notify physician immediately
- Prepare emergency medications (epinephrine, steroids)
- Monitor vital signs every 5 minutes
- Document all interventions thoroughly
Significant Bleeding
- Apply gentle pressure if external bleeding
- Position patient to prevent shock
- Monitor vital signs for hypovolemia
- Notify physician immediately
- Prepare for possible surgical intervention
- Maintain IV access if available
- Provide emotional support to patient
Monitoring and Follow-up Guidelines
Immediate (0-2 hours)
- • Monitor for immediate allergic reactions
- • Assess patient comfort and pain levels
- • Check for medication retention
- • Document patient response
Short-term (24-48 hours)
- • Evaluate therapeutic effectiveness
- • Monitor for side effects
- • Assess patient compliance
- • Review administration technique
Long-term (weekly)
- • Review treatment outcomes
- • Adjust medication regimen if needed
- • Screen for complications
- • Patient education reinforcement
Documentation & Legal Aspects
Essential Documentation Elements
Pre-Administration
- • Patient identification verification
- • Medication verification (name, dose, route, time)
- • Patient consent documentation
- • Allergy and contraindication assessment
- • Baseline vital signs and symptoms
During Administration
- • Exact time of administration
- • Administration technique used
- • Patient position and cooperation
- • Any complications encountered
- • Patient response during procedure
Post-Administration
- • Patient response and comfort level
- • Any adverse reactions observed
- • Patient education provided
- • Follow-up instructions given
- • Next scheduled administration
Legal Considerations in India
Consent Requirements
For vaginal drug administration, informed consent is crucial. Document verbal consent at minimum, written consent for complex procedures. Respect cultural preferences regarding gender of healthcare provider.
Privacy Protection
Maintain strict patient privacy during intimate procedures. Ensure proper draping, closed doors, and minimal personnel present. Document privacy measures taken.
Professional Boundaries
Maintain professional behavior throughout procedure. Have witness present when culturally appropriate. Document any concerns about patient behavior or inappropriate requests.
Sample Documentation Template
Date/Time: [DD/MM/YYYY, HH:MM]
Patient: [Name, MRN, DOB verified]
Medication: [Drug name, strength, lot number]
Route: [Rectal/Vaginal]
Indication: [Clinical reason for administration]
Pre-assessment: [Vital signs, symptoms, allergies checked]
Consent: [Verbal consent obtained, procedure explained]
Procedure: [Position, technique, patient cooperation]
Complications: [None noted / specific complications]
Post-administration: [Patient response, instructions given]
Signature: [Nurse name, credentials, date]
Legal Protection Strategies
Proactive Measures
- • Document everything contemporaneously
- • Use clear, objective language
- • Avoid subjective interpretations
- • Include exact quotes when relevant
- • Never alter original documentation
Risk Mitigation
- • Follow institutional protocols exactly
- • Seek supervision when uncertain
- • Report unusual incidents immediately
- • Maintain professional development
- • Keep documentation secure and confidential
Cultural Considerations in Indian Healthcare
India’s diverse cultural landscape requires exceptional sensitivity when performing intimate medical procedures. Understanding regional, religious, and social customs enhances patient care quality while maintaining therapeutic relationships. Nurses must balance medical necessity with cultural respect to achieve optimal outcomes.
Regional and Religious Considerations
Hindu Traditions
- • Modesty highly valued, especially for women
- • Preference for same-gender healthcare providers
- • Family involvement in medical decisions
- • Ritual purity concerns during menstruation
Islamic Guidelines
- • Strict modesty requirements (Hijab considerations)
- • Male healthcare providers for women generally avoided
- • Prayer times and Ramadan fasting considerations
- • Spousal consent may be culturally expected
Regional Variations
- • Urban vs. rural patient expectations differ
- • Language barriers require interpreter services
- • Traditional medicine integration requests
- • Educational level affects understanding
Culturally Sensitive Nursing Practices
Communication Strategies
- • Use respectful titles and formal address initially
- • Employ professional interpreters when needed
- • Allow family members to translate when appropriate
- • Explain procedures using culturally acceptable terms
Physical Considerations
- • Provide extra privacy measures and draping
- • Allow cultural dress modifications when safe
- • Respect personal space and touch preferences
- • Accommodate religious items and practices
Decision-Making Process
- • Include family in discussions when requested
- • Respect hierarchical family decision structures
- • Allow time for cultural consultation
- • Balance autonomy with cultural expectations
Language and Communication Adaptations
Hindi Terms
- • Dawa: Medicine
- • Peeda: Pain
- • Aaraam: Comfort/Rest
- • Suvidha: Convenience
Regional Languages
- • Learn basic medical terms in local languages
- • Use visual aids and demonstrations
- • Employ trained medical interpreters
- • Develop multilingual patient education materials
Non-verbal Communication
- • Understand cultural meanings of gestures
- • Respect eye contact preferences
- • Acknowledge family hierarchy in body language
- • Use appropriate physical positioning
Excellence in Culturally Competent Care
Exceptional nursing care in India requires continuous cultural learning and adaptation. Nurses who demonstrate cultural sensitivity while maintaining clinical excellence create therapeutic environments that honor patient dignity while achieving optimal health outcomes.
Professional Development
- • Attend cultural competency training programs
- • Study regional health beliefs and practices
- • Participate in community health initiatives
- • Collaborate with community leaders
Quality Metrics
- • Patient satisfaction scores
- • Medication compliance rates
- • Cultural incident reporting
- • Community feedback integration
Global Best Practices and Innovations
Healthcare systems worldwide have developed innovative approaches to rectal and vaginal drug administration. These international best practices offer valuable insights for improving patient care standards in Indian healthcare settings. Adopting proven methodologies from global healthcare leaders enhances both safety and efficacy outcomes.
United States Healthcare Innovations
Technology Integration
- • Electronic medication administration records (eMAR)
- • Barcode scanning for medication verification
- • Smart suppository applicators with dosing precision
- • Patient-controlled administration devices
Quality Assurance
- • Standardized competency assessments
- • Peer review programs for technique validation
- • Patient satisfaction measurement tools
- • Continuous quality improvement initiatives
Canadian Patient-Centered Approaches
Patient Education Programs
- • Multimedia educational resources in multiple languages
- • Virtual reality training for patient preparation
- • Peer support groups for complex medications
- • Home administration training programs
Cultural Integration
- • Indigenous healing practice integration
- • Multicultural healthcare teams
- • Interpreter services for all procedures
- • Cultural liaison specialist programs
United Kingdom NHS Standards
- • Evidence-based clinical guidelines
- • Mandatory competency certifications
- • Patient choice in healthcare provider gender
- • Standardized consent documentation
- • Regular audit and feedback systems
Scandinavian Patient Safety Models
- • Zero-tolerance error reporting systems
- • Interdisciplinary team consultations
- • Patient advocacy integration
- • Continuous professional development mandates
- • Research-practice integration programs
Australian Indigenous Health
- • Traditional medicine integration protocols
- • Community elder consultation processes
- • Remote area telehealth support
- • Cultural safety training requirements
- • Community-controlled health services
Implementation Recommendations for India
Short-term Adaptations
Standardized Protocols: Develop national guidelines for rectal and vaginal drug administration adapted to Indian healthcare infrastructure
Training Programs: Implement mandatory competency assessments for nurses performing these procedures
Quality Metrics: Establish patient satisfaction and safety outcome measurements
Long-term Innovations
Technology Integration: Gradual implementation of electronic documentation and medication tracking systems
Research Integration: Establish clinical research programs to develop India-specific best practices
Community Integration: Develop culturally appropriate patient education and community health programs
Excellence in Global Healthcare Standards
By incorporating international best practices while respecting Indian cultural values, healthcare institutions can achieve world-class standards in medication administration. This approach enhances patient safety, improves therapeutic outcomes, and builds trust in healthcare delivery systems across diverse populations.
Measurable Impact Goals
- • 95% patient satisfaction scores
- • Zero preventable medication errors
- • 100% staff competency certification
- • Reduced medication wastage by 30%
- • Enhanced cultural competency ratings
- • Improved therapeutic compliance rates
Conclusion and Key Takeaways
Mastering rectal and vaginal drug administration represents a crucial competency for nursing professionals in India. These alternative medication routes provide essential therapeutic options when oral administration is not feasible, offering direct local effects and bypassing hepatic metabolism. Success in these procedures requires technical proficiency, cultural sensitivity, and unwavering commitment to patient safety and dignity.
Essential Skills Mastery
- Proper suppository insertion techniques with anatomical understanding
- Cultural sensitivity in intimate medical procedures
- Comprehensive safety protocols and infection control
- Effective patient communication and education
Patient-Centered Excellence
- Dignified care delivery respecting individual preferences
- Thorough documentation and legal compliance
- Complication recognition and emergency management
- Continuous quality improvement commitment
Professional Development Pathway
Nursing excellence in medication administration evolves through continuous learning, practice refinement, and adaptation to emerging healthcare technologies. Indian nursing professionals must balance traditional cultural values with modern evidence-based practices to deliver optimal patient care in increasingly complex healthcare environments.
Future Learning Objectives
- • Advanced pharmacology understanding
- • Cultural competency enhancement
- • Technology integration skills
- • Research methodology knowledge
- • Leadership in quality improvement
- • Patient advocacy development
- • Interdisciplinary collaboration
- • Community health integration
Commitment to Excellence in Indian Healthcare
As nursing professionals in India, our dedication to mastering these essential skills contributes to the advancement of healthcare quality nationwide. Through competent, compassionate, and culturally sensitive care delivery, we honor both our professional responsibilities and the trust placed in us by diverse patient populations seeking healing and comfort.
