Fourth Stage of Labor: Maternal Assessment and Documentation
Comprehensive guide for nursing students on maternal monitoring during the recovery phase
Table of Contents
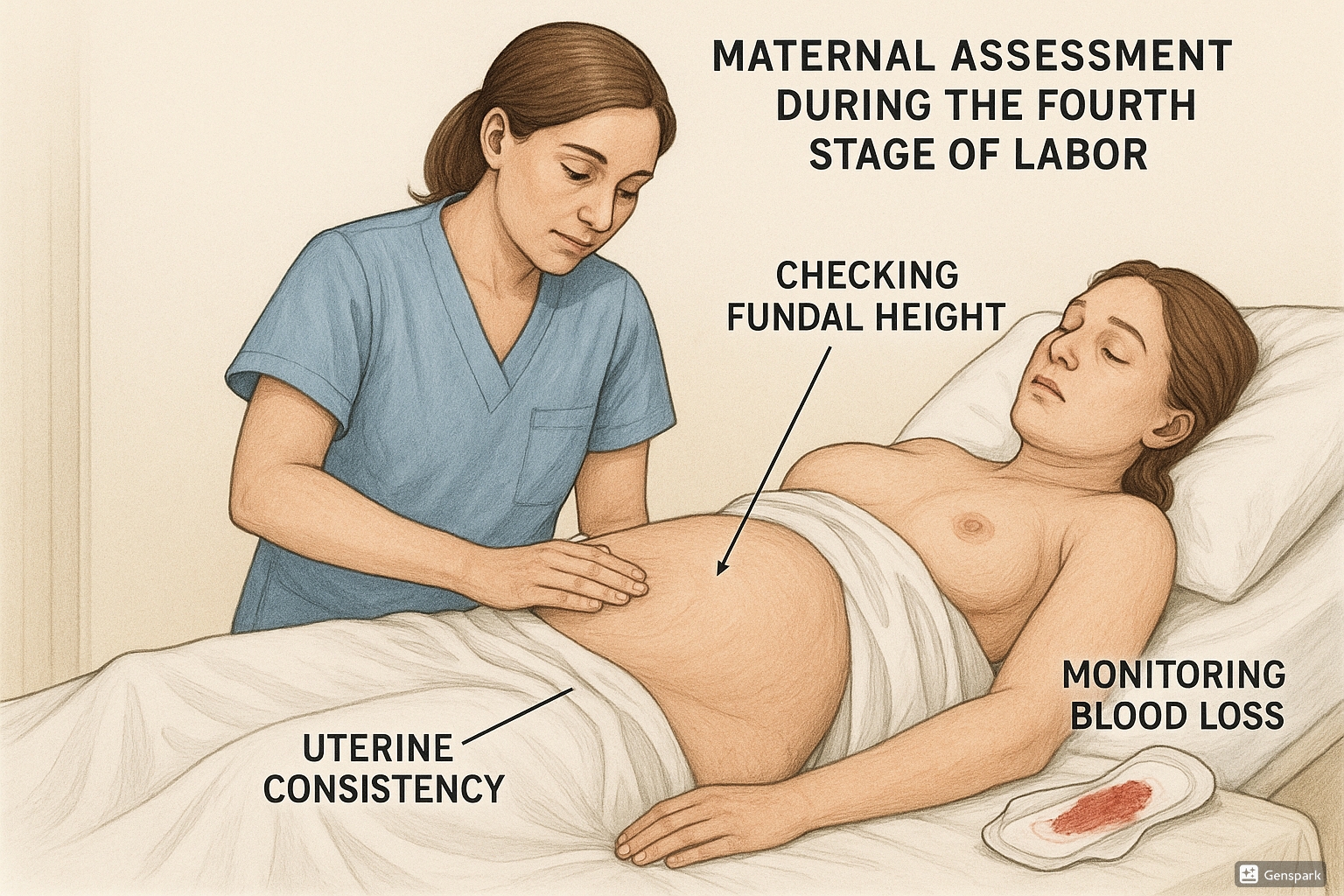
Figure 1: Visual representation of maternal assessment during the fourth stage of labor
Introduction to the Fourth Stage of Labor
The fourth stage of labor is a critical period that extends from the delivery of the placenta to approximately 1-4 hours postpartum. During this time, the mother’s body begins its recovery process, and careful monitoring is essential to ensure physiological stability and prevent complications.
The fourth stage requires vigilant nursing assessment as it represents a period of significant physiological adjustment. The maternal body undergoes rapid changes as it begins the transition from pregnancy to the postpartum state. This stage is characterized by potential hemodynamic fluctuations, uterine changes, and the risk of immediate postpartum complications such as hemorrhage.
Memory Aid: “STABLE”
Remember the key assessment priorities during the fourth stage with the acronym STABLE:
- Signs vital (monitor closely)
- Tone of uterus (should be firm)
- Amount of bleeding (quantify accurately)
- Bladder emptying (prevent distention)
- Lochia assessment (color, amount, odor)
- Emotional status (initial bonding period)
Fundal Height Assessment
Assessing fundal height is a critical component of the fourth stage maternal assessment. The fundus, or the top of the uterus, provides important information about uterine involution and potential complications like uterine atony or retained placental fragments.
1Proper Positioning for Assessment
Before assessing fundal height, ensure the mother is in a supine position with knees slightly flexed. Ask her to empty her bladder if she hasn’t recently done so, as a full bladder can displace the uterus and lead to inaccurate measurements.
2Technique for Measuring Fundal Height
Place one hand just above the symphysis pubis to stabilize the lower uterine segment. Using your other hand, palpate the abdomen to locate the fundus of the uterus. Measure the distance from the top of the symphysis pubis to the top of the fundus in centimeters or in relation to the umbilicus.
3Expected Findings
During the fourth stage of labor, the fundus is typically located at the level of the umbilicus or 1-2 cm below. The fundal height should decrease by approximately 1 cm every 24 hours (about one finger breadth) as the uterus undergoes involution.
Clinical Pearl
A fundus that is higher than expected or deviated from midline may indicate a full bladder, uterine atony, or retained placental fragments. Always assess bladder distention before concluding there is a problem with uterine involution.
| Finding | Interpretation | Nursing Action |
|---|---|---|
| Fundus at umbilicus, midline | Normal finding immediately after birth | Continue routine assessment |
| Fundus above umbilicus | Possible full bladder or uterine atony | Assess bladder, encourage voiding, reassess |
| Fundus deviated from midline | Usually indicates full bladder | Assist with voiding, catheterize if necessary |
| Fundus not palpable | Possible uterine inversion (emergency) | Notify provider immediately, prepare for intervention |
Uterine Consistency Evaluation
Assessing uterine consistency is essential for detecting signs of uterine atony, the leading cause of primary postpartum hemorrhage. A well-contracted uterus helps control bleeding from the placental site and promotes normal involution.
1Palpation Technique
Using the palm side of your hand, gently but firmly palpate the fundus in a circular motion. Note the consistency of the uterus, which should feel firm like a “grapefruit” or “softball” when properly contracted.
2Frequency of Assessment
During the fourth stage, assess uterine consistency every 15 minutes for the first hour, every 30 minutes during the second hour, and then hourly for the next 2 hours if all findings remain normal.
Memory Aid: “ROCK HARD”
To remember the characteristics of proper uterine consistency:
- Round shape
- Observably firm to touch
- Centered in the midline
- Keep checking regularly
- Hard like a grapefruit
- At the level of the umbilicus
- Resistant to indentation
- Decreasing in height over time
Normal Findings
- Firm uterus (“grapefruit-like”)
- Uterus responds to massage
- Minimal to moderate lochia
- Uterus remains contracted after massage
Abnormal Findings
- Soft, “boggy” uterus
- Uterus does not remain firm after massage
- Excessive lochia or presence of large clots
- Persistent uterine relaxation despite massage
Nursing Interventions
- Gentle fundal massage if uterus is soft
- Encourage early breastfeeding to release oxytocin
- Administer uterotonics as prescribed
- Document findings and response to interventions
Urine Output Monitoring
Monitoring urine output during the fourth stage of labor is crucial for assessing renal function, fluid balance, and preventing bladder distention that could interfere with uterine contraction.
1Assessing Bladder Fullness
Palpate the lower abdomen above the symphysis pubis to check for bladder distention. A full bladder may feel like a round, fluctuant mass and can displace the uterus upward and to the right.
2Monitoring First Void
Document the time of the first postpartum void, which should occur within 4-6 hours of delivery. The first void should be at least 150-200 mL. Inability to void or voiding small amounts may indicate urinary retention or renal issues.
Clinical Pearl
A full bladder can lead to uterine atony by preventing proper uterine contraction through mechanical obstruction. Always assess and address bladder fullness when the uterus is boggy or deviated from midline before administering additional uterotonics.
| Parameter | Normal Finding | Concerning Finding |
|---|---|---|
| First void timing | Within 4-6 hours after delivery | Unable to void after 6 hours |
| Void volume | At least 150-200 mL | <150 mL or dribbling |
| Urinary symptoms | Comfortable voiding, no pain | Painful urination, urgency without output |
| Bladder distention | No palpable bladder above symphysis | Palpable, tense bladder |
Memory Aid: “VOID”
Remember the key aspects of urine output assessment with:
- Volume (should be ≥150-200 mL)
- Obstruction (assess for inability to void)
- Initial timing (within 4-6 hours)
- Distention (check for bladder fullness)
Blood Loss Assessment
Accurate assessment of blood loss during the fourth stage of labor is essential for early detection and management of postpartum hemorrhage. Both quantitative and qualitative methods should be employed to ensure comprehensive evaluation.
1Quantitative Blood Loss Measurement
Rather than relying solely on visual estimation, which is often inaccurate, implement quantitative methods such as weighing blood-soaked materials (1g = 1mL of blood) or using calibrated drapes and collection devices. Subtract the dry weight of materials before use to determine actual blood loss.
2Lochia Assessment
Assess and document the characteristics of lochia, including:
- Color: Lochia rubra (bright red) is expected during the fourth stage
- Amount: Should saturate no more than one pad per hour
- Odor: Should have no foul smell
- Consistency: May contain small clots (<2cm), but large clots warrant investigation
3Clinical Signs of Excessive Blood Loss
Monitor for signs that may indicate significant blood loss even when visible bleeding appears normal:
- Tachycardia (heart rate >100 beats/minute)
- Hypotension (systolic BP <90 mmHg or drop of >20% from baseline)
- Tachypnea (respiratory rate >20 breaths/minute)
- Decreasing urine output (<30 mL/hour)
- Pallor, dizziness, or altered consciousness
Clinical Pearl
Visual estimation of blood loss typically underestimates actual blood loss by 30-50%. Physiological changes of pregnancy (increased blood volume) may mask signs of significant hemorrhage until 1500-2000 mL of blood has been lost.
| Blood Loss Classification | Volume | Signs & Symptoms | Nursing Action |
|---|---|---|---|
| Normal | <500 mL vaginal delivery | Stable vital signs, normal skin color | Routine monitoring |
| Stage 1 PPH | 500-1000 mL | Mild tachycardia, normal BP | Increase monitoring, assess uterine tone, notify provider |
| Stage 2 PPH | 1000-1500 mL | Tachycardia, hypotension, oliguria | Activate hemorrhage protocol, IV access, fluid resuscitation |
| Stage 3 PPH | >1500 mL | Shock, altered consciousness | Emergency response, blood products, surgical intervention may be needed |
Memory Aid: “CLOTS”
Remember the key assessments for blood loss with:
- Color of lochia
- Large clots (concerning if >2cm)
- Odor (should not be foul)
- Timing of pad saturation (should not soak one pad in less than 1 hour)
- Signs of hypovolemia (tachycardia, hypotension)
Documentation and Birth Records
Comprehensive and accurate documentation during the fourth stage of labor is not only a legal requirement but also ensures continuity of care and proper communication among healthcare providers. Proper record-keeping facilitates early identification of complications and guides appropriate interventions.
1Essential Elements for Documentation
Include the following elements in your fourth stage documentation:
- Maternal vital signs: Record BP, pulse, respiration, and temperature at the recommended intervals
- Fundal assessment: Document height, position, and consistency
- Lochia: Note color, amount, odor, and presence of clots
- Urine output: Record time and amount of first void and subsequent eliminations
- Pain assessment: Use a standardized pain scale
- Interventions: Document all interventions and the mother’s response
- Medications: Record all medications administered, including time, dose, route, and effect
2Frequency of Documentation
During the fourth stage, documentation should occur:
- Every 15 minutes for the first hour
- Every 30 minutes for the second hour
- Every hour for the subsequent 2 hours
- Immediately upon any abnormal findings or changes in maternal condition
3Birth Record Completion
Ensure the birth record includes:
- Complete delivery information (time, method, complications)
- Placental delivery (time, method, completeness, appearance)
- Estimation of blood loss during delivery and fourth stage
- Perineal status (intact, lacerations, episiotomy, repair details)
- Infant information (weight, Apgar scores, initial assessments)
- Maternal-infant bonding observations
- Breastfeeding initiation and assessment
Clinical Pearl
Remember the saying: “If it wasn’t documented, it wasn’t done.” Thorough documentation not only protects you legally but also ensures appropriate follow-up care. Use objective language and avoid subjective interpretations when documenting maternal assessments.
| Documentation Element | Frequency | Example of Proper Documentation |
|---|---|---|
| Vital signs | Per facility protocol (typically q15min x1hr, q30min x1hr, then q1hr x2hrs) | “1415: BP 118/72, P 82, R 18, T 37.0°C” |
| Fundal assessment | Same as vital signs | “1415: Fundus firm, midline, at umbilicus” |
| Lochia | Same as vital signs | “1415: Moderate lochia rubra, no clots noted, 1/4 pad saturated” |
| Urine output | Each void | “1430: Voided 250mL clear yellow urine without difficulty” |
| Interventions | As performed | “1440: Fundal massage performed x1 due to slight bogginess, fundus firm after massage” |
BUBBLE-HE Assessment Framework
The BUBBLE-HE framework provides a comprehensive, systematic approach to postpartum assessment during the fourth stage of labor. This mnemonic encompasses all critical aspects of maternal evaluation to ensure thorough assessment and early detection of complications.
B – Breasts
Assess for:
- Softness or engorgement
- Nipple condition and evidence of colostrum
- Pain or discomfort
- Early breastfeeding success
U – Uterus
Assess for:
- Fundal height and position
- Consistency (firm vs. boggy)
- Response to massage if needed
- Changes over time
B – Bladder
Assess for:
- Distention
- Ability to void spontaneously
- Adequate volume of first void
- Discomfort or pain with urination
B – Bowels
Assess for:
- Bowel sounds
- Passage of flatus
- Abdominal distention
- Concerns about first bowel movement
L – Lochia
Assess for:
- Color (rubra initially)
- Amount (pad count and saturation)
- Odor (should not be foul)
- Presence and size of clots
E – Episiotomy/Perineum
Assess for:
- Integrity of repairs if present
- Swelling or bruising
- Pain or discomfort
- Signs of infection
H – Homan’s Sign
Assess for:
- Calf pain with dorsiflexion of foot
- Swelling or warmth in legs
- Signs of deep vein thrombosis
- Encourage early ambulation when appropriate
E – Emotional Status
Assess for:
- Mood and affect
- Bonding with the newborn
- Early signs of postpartum blues
- Support system availability
Memory Aid: Visualization Technique
To remember the BUBBLE-HE assessment order, imagine a bubble floating upward from the perineum to the breasts, then extending to the legs (H) and finally to the mind (E). This visual path follows the same direction as your physical assessment.
Best Practices & Latest Updates
The following represent current evidence-based practices and recent updates in maternal assessment during the fourth stage of labor. Incorporating these approaches can enhance care quality and improve maternal outcomes.
Best Practice #1: Quantitative Blood Loss Measurement
Recent guidelines from ACOG and other maternal health organizations now recommend quantitative blood loss (QBL) measurement rather than visual estimation. QBL involves weighing blood-soaked materials or using calibrated collecting devices to accurately measure blood loss.
Implementation strategies include:
- Pre-weighing dry pads and subtracting from wet weight (1g = 1mL)
- Using graduated containers for collecting fluid
- Implementing standardized QBL protocols facility-wide
- Regular staff training on QBL techniques
Impact: QBL has been shown to improve early detection of postpartum hemorrhage, allowing for more timely interventions and reduced maternal morbidity.
Best Practice #2: Early Warning Scoring Systems
Maternal Early Warning Systems (MEWS) or Obstetric Early Warning Scores (OEWS) are now being implemented to improve detection of deterioration during the fourth stage. These scoring systems use vital sign parameters to identify at-risk mothers before critical deterioration occurs.
Key components include:
- Standardized vital sign thresholds that trigger escalation
- Clear protocols for response to concerning scores
- Integration into electronic health records
- Regular reassessment after interventions
Impact: Studies show that implementation of early warning systems can reduce severe maternal morbidity by up to 20% through earlier recognition and intervention.
Best Practice #3: Enhanced Recovery After Delivery
Enhanced Recovery After Delivery (ERAD) protocols are being adapted from surgical enhanced recovery pathways to improve fourth stage outcomes. These protocols focus on early mobilization, appropriate pain management, early oral intake, and bladder management.
Key elements include:
- Early ambulation within 4-6 hours after delivery (if stable)
- Multimodal pain management strategies that minimize opioid use
- Early removal of urinary catheters when present
- Prompt oral hydration and nutrition
- Risk-based thromboembolism prophylaxis
Impact: ERAD protocols have been associated with reduced length of stay, decreased opioid use, improved patient satisfaction, and fewer complications during the fourth stage and beyond.
