Meeting Nutritional Needs: Oral Nutrition
Comprehensive Nursing Notes
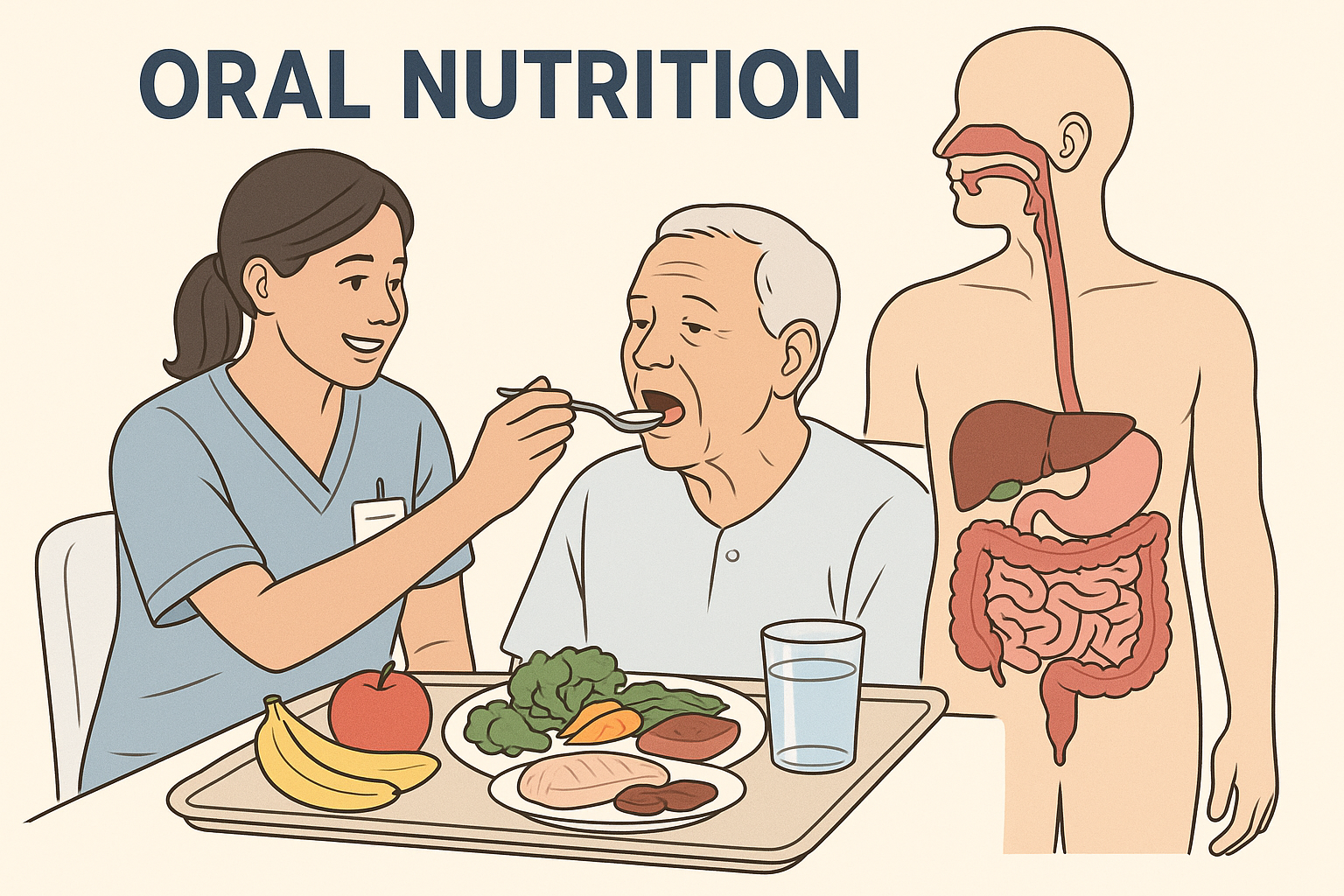
Professional nursing care in oral nutrition management
Learning Objectives
Principles of Oral Nutrition
MNEMONIC: “NOURISH”
Core Principles
Nutritional Balance
Ensuring adequate intake of macronutrients (carbohydrates, proteins, fats) and micronutrients (vitamins, minerals) to meet individual metabolic needs.
Safety First
Preventing aspiration, choking, and foodborne illness through proper assessment, positioning, and food handling techniques.
Patient-Centered Care
Incorporating cultural preferences, dietary restrictions, and individual needs into nutritional planning and implementation.
Physiological Considerations
Hierarchy of Nutritional Needs
Evidence-Based Practice
Clinical Pearl
Research demonstrates that maintaining oral nutrition whenever possible leads to better patient outcomes compared to alternative feeding methods. The gastrointestinal tract should be used when it functions properly, following the principle “if the gut works, use it.”
Equipment and Supplies
Essential Equipment
Adaptive Utensils
Built-up handles, weighted utensils, angled spoons
Drinking Aids
Straws, sippy cups, specialized cups
Positioning Aids
Bed tables, supportive cushions
Monitoring Tools
Food thermometers, portion scales
Safety Equipment
Bibs, napkins, suction equipment
Documentation
Intake charts, assessment forms
Specialized Equipment for Different Conditions
| Condition | Equipment | Purpose |
|---|---|---|
| Dysphagia | Thickening agents, texture-modified foods | Prevent aspiration, facilitate swallowing |
| Tremor/Parkinson’s | Weighted utensils, non-slip mats | Improve stability and control |
| Arthritis | Built-up handles, lever-style can openers | Reduce joint stress and pain |
| Visual impairment | Tactile markers, contrasting colors | Enhance independence and safety |
| Cognitive impairment | Simplified utensils, finger foods | Maintain dignity and autonomy |
Equipment Safety Alert
Always inspect equipment before use for cracks, wear, or damage. Ensure all adaptive equipment is properly cleaned and sanitized between uses. Match equipment to patient’s specific needs and abilities.
Procedures and Techniques
Pre-Feeding Assessment
Check for swallowing disorders, allergies, dietary restrictions
Ensure patient is alert and oriented
Perform swallow screen if indicated
Ensure proper positioning for safe feeding
Assess mouth, teeth, and oral moisture
Feeding Procedure
Preparation Phase
- • Wash hands thoroughly
- • Gather necessary equipment
- • Verify patient identity
- • Explain procedure to patient
- • Ensure privacy and comfort
Positioning
- • Elevate head of bed 45-90 degrees
- • Support arms and shoulders
- • Ensure feet are supported
- • Position over-bed table appropriately
- • Provide adequate lighting
During Feeding
Best Practice Guidelines
Pacing
Allow adequate time between bites (5-10 seconds) to ensure complete swallowing
Observation
Monitor for signs of aspiration, fatigue, or distress throughout feeding
Encouragement
Provide positive reinforcement and maintain conversation to promote normalcy
Flexibility
Adapt approach based on patient’s energy level and preferences
Post-Feeding Care
Essential Post-Feeding Steps
Immediate (0-30 minutes)
- • Keep patient upright
- • Provide oral hygiene
- • Monitor for reflux
- • Document intake
Short-term (30-60 minutes)
- • Continue position monitoring
- • Assess comfort level
- • Check for delayed reactions
- • Plan next feeding
Long-term (1-24 hours)
- • Monitor weight trends
- • Assess overall nutrition status
- • Evaluate feeding tolerance
- • Adjust care plan as needed
Indications and Contraindications
Indications for Oral Nutrition
- Intact swallowing reflex – Normal or manageable dysphagia
- Adequate consciousness – Alert and oriented patient
- Functioning GI tract – Normal digestion and absorption
- Stable medical condition – No acute distress
- Nutritional maintenance – Adequate intake possible
Contraindications
- Severe dysphagia – High aspiration risk
- Altered consciousness – Coma, severe confusion
- GI obstruction – Bowel obstruction or severe ileus
- Severe nausea/vomiting – Persistent symptoms
- Respiratory distress – Compromised airway
Relative Contraindications
These conditions require careful assessment and may necessitate modified approaches:
Neurological Conditions
- • Stroke with mild dysphagia
- • Parkinson’s disease
- • Multiple sclerosis
- • Traumatic brain injury
Medical Conditions
- • Chronic kidney disease
- • Liver disease
- • Inflammatory bowel disease
- • Diabetes with gastroparesis
Assessment and Monitoring
Comprehensive Nutritional Assessment
MNEMONIC: “ABCDE Assessment”
Assessment Checklist
Pre-Feeding Assessment
Physical Assessment
Functional Assessment
Monitoring Parameters
| Parameter | Frequency | Normal Range/Expected | Action if Abnormal |
|---|---|---|---|
| Weight | Daily to weekly | Stable ± 2 lbs | Assess intake, adjust plan |
| Intake/Output | Each meal/shift | 75-100% of prescribed | Document, investigate causes |
| Albumin | Weekly | 3.5-5.0 g/dL | Nutritional consultation |
| Prealbumin | 2-3 times weekly | 15-35 mg/dL | Adjust protein intake |
| Hydration status | Each shift | Moist mucous membranes | Increase fluid intake |
Clinical Pearl: Early Warning Signs
Watch for these subtle indicators of nutritional compromise:
Physical Signs
- • Fatigue or weakness
- • Poor wound healing
- • Dry, brittle hair
- • Pale skin color
Behavioral Changes
- • Decreased appetite
- • Food aversion
- • Increased sleepiness
- • Confusion or irritability
Functional Decline
- • Difficulty chewing
- • Slower eating pace
- • Increased dependence
- • Frequent infections
Special Populations and Considerations
Elderly Patients
Unique Considerations:
- • Decreased taste and smell
- • Dental problems
- • Medication interactions
- • Slower gastric emptying
- • Increased risk of dehydration
Nursing Strategies:
- • Enhance food flavors safely
- • Provide smaller, frequent meals
- • Ensure adequate hydration
- • Monitor for drug-nutrient interactions
Pediatric Patients
Unique Considerations:
- • Rapid growth requirements
- • Developing eating skills
- • Fear and anxiety
- • Parental involvement
- • Choking risk
Nursing Strategies:
- • Age-appropriate foods
- • Involve parents in feeding
- • Use distraction techniques
- • Ensure food safety
Neurological Conditions
Common Challenges:
- • Dysphagia
- • Cognitive impairment
- • Motor control issues
- • Behavioral changes
- • Communication difficulties
Nursing Interventions:
- • Texture modifications
- • Swallowing therapy collaboration
- • Consistent routines
- • Environmental modifications
Chronic Conditions
Disease-Specific Needs:
- • Diabetes: Carbohydrate counting
- • Heart failure: Sodium restriction
- • Kidney disease: Protein/phosphorus limits
- • COPD: High-calorie, small meals
- • Cancer: Symptom management
Collaborative Care:
- • Dietitian consultation
- • Medication timing
- • Symptom monitoring
- • Family education
Complications and Troubleshooting
Common Complications
Aspiration
Signs:
- • Coughing during eating
- • Wet voice after swallowing
- • Chest congestion
- • Fever
Prevention:
- • Proper positioning
- • Texture modifications
- • Slow feeding pace
- • Swallow screening
Malnutrition
Risk Factors:
- • Poor appetite
- • Difficulty chewing/swallowing
- • Chronic illness
- • Medications
Interventions:
- • Nutritional supplements
- • Frequent small meals
- • Favorite foods
- • Dietitian consult
Troubleshooting Guide
Emergency Situations
Know when to stop feeding and seek immediate help:
Stop Feeding If:
- • Choking or severe coughing
- • Difficulty breathing
- • Loss of consciousness
- • Severe nausea/vomiting
Immediate Actions:
- • Position upright
- • Suction if available
- • Call for assistance
- • Monitor vital signs
Follow-up:
- • Document incident
- • Notify physician
- • Reassess feeding plan
- • Consider alternatives
Documentation and Legal Considerations
Essential Documentation
MNEMONIC: “FEAST”
Documentation Requirements
| Category | Required Elements | Frequency |
|---|---|---|
| Intake Assessment | Percentage eaten, types of food, fluid intake | Each meal |
| Tolerance | Swallowing ability, nausea, vomiting, satisfaction | Each feeding |
| Interventions | Positioning, assistance provided, modifications | As performed |
| Patient Response | Cooperation, preferences, complications | Each shift |
| Education | Teaching provided, understanding demonstrated | As provided |
Legal and Ethical Considerations
Patient Rights
- • Right to refuse food/treatment
- • Cultural and religious considerations
- • Informed consent for modifications
- • Privacy during feeding
- • Dignity and respect
Nurse Responsibilities
- • Competent assessment and intervention
- • Accurate documentation
- • Timely communication with team
- • Advocacy for patient needs
- • Continuing education
Evidence-Based Practice and Quality Improvement
Current Research and Guidelines
Key Evidence-Based Practices
Screening and Assessment
- • Use validated screening tools (MNA, MUST)
- • Implement standardized swallow screening
- • Regular nutritional risk assessment
- • Multidisciplinary team approach
Intervention Strategies
- • Texture modification based on IDDSI levels
- • Oral care protocols improve intake
- • Family involvement enhances outcomes
- • Environmental modifications reduce distractions
Quality Indicators
Measuring Success
Process Indicators
- • Screening completion rates
- • Dietitian referral timeliness
- • Staff compliance with protocols
- • Documentation completeness
Outcome Indicators
- • Weight maintenance/gain
- • Reduced aspiration events
- • Improved albumin levels
- • Patient satisfaction scores
Safety Indicators
- • Aspiration pneumonia rates
- • Choking incidents
- • Feeding-related falls
- • Medication errors
Summary and Key Takeaways
Essential Points for Nursing Practice
Assessment is Key
Thorough assessment of swallowing ability, nutritional status, and individual needs forms the foundation of safe and effective oral nutrition support.
Safety First
Preventing aspiration and maintaining airway safety should always be the primary consideration in oral nutrition interventions.
Individualized Care
Each patient’s cultural background, preferences, and medical conditions require personalized approaches to nutrition support.
Team Collaboration
Effective nutrition support requires collaboration with dietitians, speech therapists, physicians, and family members.
Final MNEMONIC: “NUTRITION”
References and Additional Resources
Professional Organizations
- • Academy of Nutrition and Dietetics
- • American Speech-Language-Hearing Association
- • International Dysphagia Diet Standardisation Initiative
- • American Nurses Association
Assessment Tools
- • Mini Nutritional Assessment (MNA)
- • Malnutrition Universal Screening Tool (MUST)
- • Subjective Global Assessment (SGA)
- • 3-Minute Nutrition Screening
Additional Learning Resources
• Consult your institution’s policies and procedures for specific protocols
• Review current evidence-based guidelines from professional organizations
• Participate in continuing education programs on nutrition and dysphagia
• Collaborate with speech-language pathologists and registered dietitians
Comprehensive Nursing Notes – Meeting Nutritional Needs: Oral Nutrition
Created for nursing students following evidence-based practice guidelines
