Nasal and Throat Spraying & Inhalation Therapy
Complete Nursing Guide
Master the art of respiratory medication administration
Table of Contents
Introduction to Respiratory Administration
Respiratory medication administration through nasal and throat spraying, along with various inhalation therapies, represents a critical component of modern nursing practice. These techniques provide direct access to the respiratory system, enabling rapid medication absorption and therapeutic effects. Understanding proper inhalation techniques, equipment usage, and patient safety measures is essential for delivering quality respiratory care.
Primary Purposes
- Direct medication delivery to respiratory tract
- Rapid therapeutic onset through mucosal absorption
- Localized treatment with minimal systemic effects
- Emergency respiratory interventions
Key Considerations
- Patient positioning and comfort
- Proper technique demonstration
- Equipment sterility and maintenance
- Adverse reaction monitoring
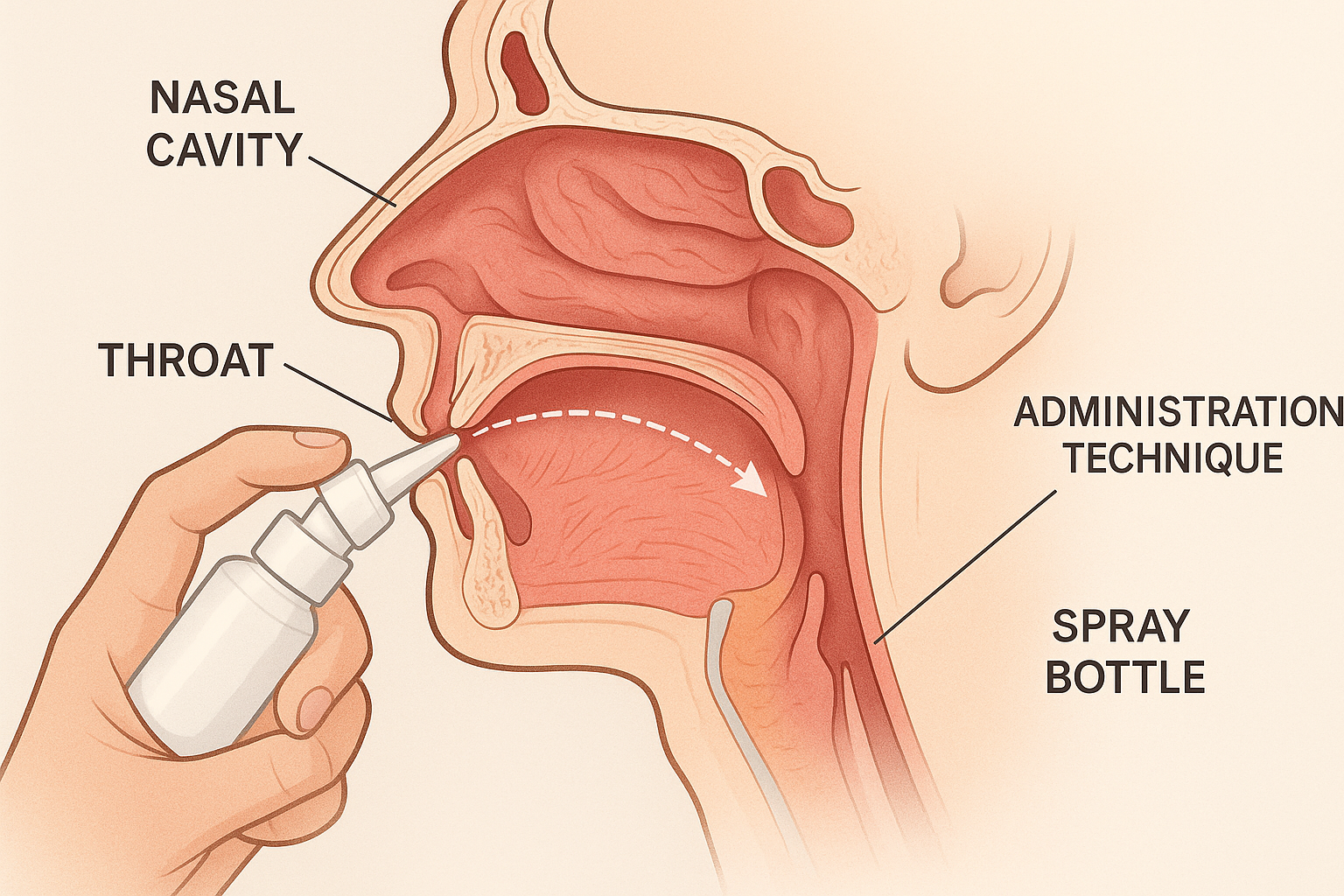
Proper nasal spray administration technique with anatomical positioning
Nasal Spraying Techniques
Memory Aid: NASAL
Nose position upright
Aim away from nasal septum
Squeeze bottle gently
Avoid sniffing immediately
Lean head slightly forward
Step-by-Step Procedure
Explain procedure and obtain patient consent
Perform hand hygiene and don gloves if necessary
Check medication label against prescription
Position patient sitting upright or standing
Have patient blow nose gently to clear passages
Insert spray tip into nostril, aim toward ear
Compress spray bottle while patient inhales gently
Remove spray tip and have patient breathe normally
Types of Nasal Medications
| Medication Type | Primary Use | Onset Time |
|---|---|---|
| Decongestants | Reduce nasal congestion | 5-10 minutes |
| Corticosteroids | Anti-inflammatory effects | 1-3 days |
| Antihistamines | Allergy symptom relief | 15-30 minutes |
| Antibiotics | Treat bacterial infections | 24-48 hours |
| Emergency medications | Rapid systemic absorption | 2-5 minutes |
Throat Spraying Methods
Common Throat Spray Indications
- Sore throat and pharyngitis
- Local anesthesia before procedures
- Antiseptic treatment for oral infections
- Pain relief and inflammation reduction
- Moisturizing dry throat tissues
Safety Precautions
- Check for allergies to spray components
- Avoid spraying directly into larynx
- Monitor for gag reflex and choking
- Ensure proper lighting and visualization
- Have suction equipment readily available
Throat Spray Administration Protocol
Preparation Phase
- • Verify patient identity and medication order
- • Assess patient’s ability to cooperate
- • Position patient comfortably
- • Prepare adequate lighting source
Administration Phase
- • Ask patient to open mouth wide
- • Direct spray toward affected area
- • Apply prescribed number of sprays
- • Advise patient to avoid swallowing immediately
Inhalation Therapy Overview
Inhalation therapy encompasses various methods of delivering medications, oxygen, and therapeutic agents directly to the respiratory system. This approach maximizes therapeutic benefits while minimizing systemic side effects. The three primary routes include nasal inhalation, oral inhalation, and endotracheal inhalation, each serving specific clinical purposes and patient populations.
Physiological Benefits
- • Direct medication delivery to target tissues
- • Rapid onset of therapeutic action
- • Reduced systemic medication exposure
- • Lower risk of systemic adverse effects
Therapeutic Applications
- • Bronchodilation for asthma and COPD
- • Anti-inflammatory treatment
- • Mucolytic therapy for secretion management
- • Antimicrobial treatment for respiratory infections
Patient Considerations
- • Age and developmental status
- • Cognitive ability and cooperation
- • Manual dexterity and coordination
- • Severity of respiratory compromise
| Inhalation Route | Primary Indications | Equipment Required | Patient Population |
|---|---|---|---|
| Nasal Inhalation | Systemic medication delivery, emergency drugs | Nasal cannula, mask, nebulizer | All ages, conscious patients |
| Oral Inhalation | Bronchodilation, anti-inflammatory | MDI, DPI, nebulizer with mask | Cooperative patients, age-appropriate |
| Endotracheal Inhalation | Critical care, mechanical ventilation | Ventilator circuit, inline nebulizer | Intubated patients, ICU settings |
Nasal Inhalation Procedures
Memory Aid: BREATHE
Blow nose gently before treatment
Relax and breathe normally
Ensure proper positioning
Allow medication to settle
Time intervals between doses
Hold breath momentarily
Evaluate patient response
Equipment for Nasal Inhalation
- Nasal cannula or prongs
- Oxygen flow meter
- Humidifier bottle
- Nebulizer chamber
- Connecting tubing
- Pulse oximeter for monitoring
Comprehensive Nasal Inhalation Protocol
Pre-Administration
- • Verify physician’s order and medication
- • Check patient allergies and contraindications
- • Assess baseline vital signs and oxygen saturation
- • Explain procedure and obtain consent
- • Position patient in semi-Fowler’s or upright position
During Administration
- • Insert nasal cannula properly into nares
- • Set prescribed flow rate and concentration
- • Monitor patient comfort and tolerance
- • Observe for signs of improvement or adverse effects
- • Document start time and initial patient response
Post-Administration
- • Monitor vital signs and oxygen saturation
- • Assess effectiveness of treatment
- • Check for nasal irritation or dryness
- • Provide patient education on home use if applicable
- • Complete documentation requirements
Oral Inhalation Techniques
Oral inhalation represents the most common method of respiratory medication delivery, particularly for patients with asthma, COPD, and other chronic respiratory conditions. Proper inhalation technique is crucial for medication effectiveness, requiring patient education and regular assessment to ensure optimal therapeutic outcomes.
Metered Dose Inhaler (MDI) Technique
Remove cap and shake inhaler vigorously 5-10 times
Exhale normally, away from the inhaler
Form tight seal around mouthpiece with lips
Begin slow, deep inhalation and press canister once
Continue inhaling slowly and deeply
Hold breath for 10 seconds or as long as comfortable
Exhale slowly and repeat if second dose prescribed
Dry Powder Inhaler (DPI) Technique
Check dose counter and prepare inhaler per instructions
Load dose by turning or clicking mechanism
Exhale fully away from the device
Place lips firmly around mouthpiece
Inhale forcefully and deeply through mouth
Remove inhaler and hold breath for 10 seconds
Exhale slowly and rinse mouth if using corticosteroids
Common Inhalation Technique Errors
Technical Errors
- • Inadequate shaking of MDI device
- • Poor coordination of actuation and inhalation
- • Too rapid or too slow inhalation rate
- • Insufficient breath-holding time
- • Multiple actuations in single breath
Preparation Errors
- • Not removing cap from inhaler
- • Failure to prime new inhaler
- • Incorrect positioning of device
- • Not exhaling before inhalation
- • Using expired or empty inhaler
Endotracheal and Tracheal Inhalation
Endotracheal and tracheal inhalation therapy provides direct medication delivery to intubated patients or those with tracheostomies. This method ensures precise drug delivery to the lower respiratory tract and is essential in critical care settings where conventional inhalation methods are not feasible.
Clinical Indications
- Mechanically ventilated patients
- Patients with artificial airways
- Severe respiratory compromise requiring direct delivery
- Emergency medication administration
- Pulmonary edema treatment
Safety Considerations
- Maintain sterile technique throughout procedure
- Monitor for ventilator alarm activation
- Assess for signs of respiratory distress
- Ensure proper medication dosage for direct delivery
- Monitor hemodynamic stability during administration
Endotracheal Medication Administration Protocol
Preparation
- • Verify medication order
- • Gather sterile supplies
- • Check ventilator settings
- • Position patient appropriately
- • Don protective equipment
Medication Setup
- • Prepare medication per protocol
- • Use appropriate delivery device
- • Check medication concentration
- • Prime inline nebulizer if used
- • Ensure sterile connections
Administration
- • Connect to ventilator circuit
- • Administer over prescribed time
- • Monitor patient response
- • Maintain ventilator support
- • Document administration
Post-Care
- • Monitor vital signs
- • Assess therapeutic response
- • Clean equipment properly
- • Continue respiratory support
- • Complete documentation
Equipment and Supplies
Nasal and Throat Spraying Equipment
| Equipment | Purpose |
|---|---|
| Metered spray bottles | Precise dose delivery |
| Atomizers | Fine mist generation |
| Tongue depressors | Throat visualization |
| Penlight | Adequate illumination |
| Tissues | Patient comfort |
Inhalation Therapy Equipment
Equipment Check: SECURE
Sterilize all reusable equipment
Expire dates checked on medications
Calibrate flow meters and devices
Uniformity of spray pattern verified
Replace worn or damaged components
Ensure backup equipment available
Maintenance Requirements
- Daily cleaning of reusable components
- Weekly deep cleaning and disinfection
- Monthly calibration of flow meters
- Quarterly replacement of filters
- Annual professional servicing
Infection Control Measures
- • Single-use items must never be reused between patients
- • Nebulizer chambers require thorough disinfection after each use
- • Hand hygiene before and after equipment handling
- • Personal protective equipment use as indicated
- • Proper disposal of contaminated materials
Documentation and Reporting
Comprehensive documentation of nasal, throat, and inhalation therapy administration is essential for legal compliance, continuity of care, and quality improvement initiatives. Proper recording ensures healthcare team communication and supports evidence-based practice adjustments based on patient response patterns.
Essential Documentation Elements
Patient Information
- • Patient identification and allergies
- • Baseline vital signs and assessments
- • Pre-existing respiratory conditions
Medication Details
- • Medication name, dose, and concentration
- • Route of administration and technique used
- • Time and duration of treatment
Patient Response
- • Immediate and ongoing patient responses
- • Adverse reactions or complications
- • Effectiveness of treatment
Monitoring Parameters
| Parameter | Frequency | Normal Range |
|---|---|---|
| Oxygen Saturation | Continuous | 95-100% |
| Respiratory Rate | Every 15 minutes | 12-20/min |
| Heart Rate | Every 15 minutes | 60-100 bpm |
| Blood Pressure | Pre/post treatment | 120/80 mmHg |
| Peak Flow | As indicated | Variable by age |
Reporting Requirements and Alert Conditions
Immediate Reporting Required
- Severe allergic reactions or anaphylaxis
- Significant respiratory distress or failure
- Hemodynamic instability following treatment
- Equipment malfunction or medication errors
Documentation Timeframes
- Immediate: Critical events and adverse reactions
- Within 1 hour: Routine medication administration
- End of shift: Complete assessment and response data
- 24 hours: Follow-up effectiveness evaluation
Sample Documentation Template
Date/Time: [Current date and time]
Medication: [Drug name, dose, route]
Indication: [Reason for administration]
Pre-treatment Assessment: [Vital signs, symptoms]
Administration Details: [Technique, patient cooperation]
Post-treatment Response: [Patient tolerance, effectiveness]
Patient Education: [Teaching provided, understanding demonstrated]
Nurse Signature: [Name and credentials]
Global Best Practices and Innovations
International Standards and Guidelines
Innovative Technologies and Approaches
Excellence in Practice: Canadian Model
Healthcare institutions in Canada have pioneered a comprehensive approach to inhalation therapy that combines evidence-based protocols with patient-centered care. Their model emphasizes multidisciplinary collaboration between respiratory therapists, nurses, and pharmacists to optimize medication delivery outcomes.
Patient Education
Standardized teach-back methods with video demonstrations and multilingual resources
Quality Assurance
Regular competency assessments and peer review processes for all healthcare providers
Technology Integration
Electronic health records with automated alerts for technique reinforcement needs
Continuing Education Trends
- Simulation-based learning for complex inhalation procedures
- Interprofessional education programs promoting team-based care
- Online competency modules with interactive case studies
- Annual certification requirements for specialized inhalation therapy
Patient-Centered Care Models
- Shared decision-making in device selection and treatment plans
- Cultural competency training for diverse patient populations
- Home care transition programs with follow-up assessments
- Family involvement in education and technique reinforcement
Key Takeaways for Nursing Excellence
Mastering nasal and throat spraying techniques alongside various inhalation therapy methods requires dedication to continuous learning and patient-centered practice. Understanding the nuances of each administration route empowers nurses to provide optimal respiratory care while ensuring patient safety and therapeutic effectiveness.
- Practice evidence-based techniques consistently
- Prioritize patient education and empowerment
- Maintain competency through ongoing education
- Document thoroughly for continuity of care
