Normal Labour and Birth
Comprehensive Guide for Nursing Students
Table of Contents
Introduction
Normal labor is the physiological process by which regular uterine contractions cause progressive cervical dilation and effacement, resulting in the delivery of the fetus, placenta, and membranes through the birth canal. This process typically occurs around 40 weeks of gestation and is considered a normal labor when it begins spontaneously, progresses without complications, and results in a vaginal birth without major interventions.
Understanding the normal labor process is essential for nursing students to provide appropriate care, recognize deviations from normal patterns, and support the birthing person through this significant life event. This comprehensive guide covers the physiological processes, stages, assessment, management, and care approaches for normal labor.
Physiology of Labor
The Onset of Labor
While the exact trigger for the onset of normal labor remains not fully understood, several physiological processes are believed to contribute:
- Fetal Factors: Increased production of cortisol and other hormones by the maturing fetal adrenal glands
- Placental Factors: Changes in estrogen and progesterone levels as the placenta ages
- Uterine Factors: Increased sensitivity to oxytocin due to higher numbers of oxytocin receptors
- Mechanical Factors: Stretching of the uterus and cervix
The Three P’s of Labor
Successful normal labor depends on the interaction of three key components:
Powers
Uterine contractions and maternal pushing efforts
Passage
Size and shape of the maternal pelvis
Passenger
Size, position, and presentation of the fetus
Hormonal Influences
| Hormone | Source | Function in Labor |
|---|---|---|
| Oxytocin | Posterior pituitary gland | Stimulates uterine contractions; increases in frequency and intensity throughout labor |
| Prostaglandins | Uterine decidua, fetal membranes | Soften and efface the cervix; enhance uterine contractions |
| Estrogen | Placenta | Increases uterine sensitivity to oxytocin; promotes prostaglandin synthesis |
| Progesterone | Placenta | Decreases prior to labor onset, removing inhibition of uterine contractions |
| Relaxin | Corpus luteum, placenta | Softens cervix; relaxes pelvic ligaments |
| Endorphins | Pituitary gland | Natural pain relief; levels increase with labor progression |
Uterine Activity
Uterine contractions in normal labor have specific characteristics:
- Frequency: Measured from the beginning of one contraction to the beginning of the next
- Duration: Length of time a single contraction lasts
- Intensity: Strength of the contraction, assessed by palpation or intrauterine pressure catheter (measured in mmHg)
- Resting Tone: Pressure within the uterus between contractions (normally 5-15 mmHg)
Stages of Normal Labor
Normal labor is divided into three distinct stages, with some sources recognizing a fourth recovery stage.
First Stage: Dilation
The first stage begins with the onset of regular uterine contractions that cause cervical change and ends with full cervical dilation (10 cm). It is divided into two phases:
Latent Phase
- Cervical dilation: 0-6 cm
- Duration: Variable and typically longer (up to 20 hours in nulliparous women, up to 14 hours in multiparous women)
- Contractions: Mild to moderate intensity, irregular becoming regular (every 5-30 minutes)
- Maternal experience: Generally able to talk through contractions
Active Phase
- Cervical dilation: 6-10 cm
- Duration: More predictable (average rate of dilation 1-2 cm/hour for nulliparous, faster for multiparous)
- Contractions: Regular, strong (every 2-3 minutes), lasting 60-90 seconds
- Maternal experience: Increased discomfort, focused on breathing through contractions
Clinical Note: Active phase arrest is diagnosed when there is no cervical change for at least 4 hours with adequate contractions, or 6 hours with inadequate contractions despite oxytocin administration.
Second Stage: Delivery of Fetus
The second stage begins when the cervix is fully dilated (10 cm) and ends with the delivery of the neonate.
Characteristics
- Duration:
- Nulliparous without epidural: average 0.6 hours (upper limit 2.8 hours)
- Nulliparous with epidural: average 1.1 hours (upper limit 3.6 hours)
- Multiparous without epidural: 0.1-0.2 hours (upper limit 1.1-1.3 hours)
- Multiparous with epidural: 0.3-0.4 hours (upper limit 1.6-2.0 hours)
- Contractions: Regular and strong, every 2-3 minutes, lasting 60-90 seconds
- Maternal sensation: Strong urge to push, rectal pressure
Phases of Second Stage
- Passive descent (Laboring down): Period between full dilation and active pushing
- Active pushing: Maternal expulsive efforts
Important: Prolonged second stage is defined as pushing for more than 3 hours in nulliparous patients and more than 2 hours in multiparous patients, according to ACOG guidelines.
Third Stage: Delivery of Placenta
The third stage begins immediately after the delivery of the fetus and ends with the delivery of the placenta.
Characteristics
- Duration: Typically 5-30 minutes
- Signs of placental separation:
- Gush of blood from the vagina
- Lengthening of the umbilical cord
- Change in uterine shape (globular)
- Firm contraction of the uterus
- Methods of management:
- Active management: Administration of uterotonic drugs (typically oxytocin), controlled cord traction, and uterine massage
- Expectant management: Awaiting spontaneous placental separation and delivery without intervention
Nursing Tip: Active management of the third stage reduces the risk of postpartum hemorrhage by up to 60% and is the recommended approach in most settings.
Fourth Stage: Recovery
The fourth stage is the first 1-3 hours after delivery of the placenta. While not traditionally recognized in all sources, this period is crucial for maternal recovery and requires close monitoring.
Clinical Focus
- Vital signs: Regular monitoring for postpartum complications
- Uterine tone: Assessing firmness and position
- Bleeding: Evaluating quantity and character of lochia
- Maternal well-being: Pain management, voiding, recovery from anesthesia if applicable
- Bonding: Supporting skin-to-skin contact and breastfeeding initiation
Nursing Tip: The “Rule of 4s” can help guide assessment: check fundus, lochia, vital signs, and comfort every 15 minutes for the first hour, then every 30 minutes for the second hour, and then hourly.
Cardinal Movements of Labor
During normal labor, the fetus undergoes a series of passive movements to navigate through the maternal pelvis. These are known as the cardinal movements or mechanisms of labor.
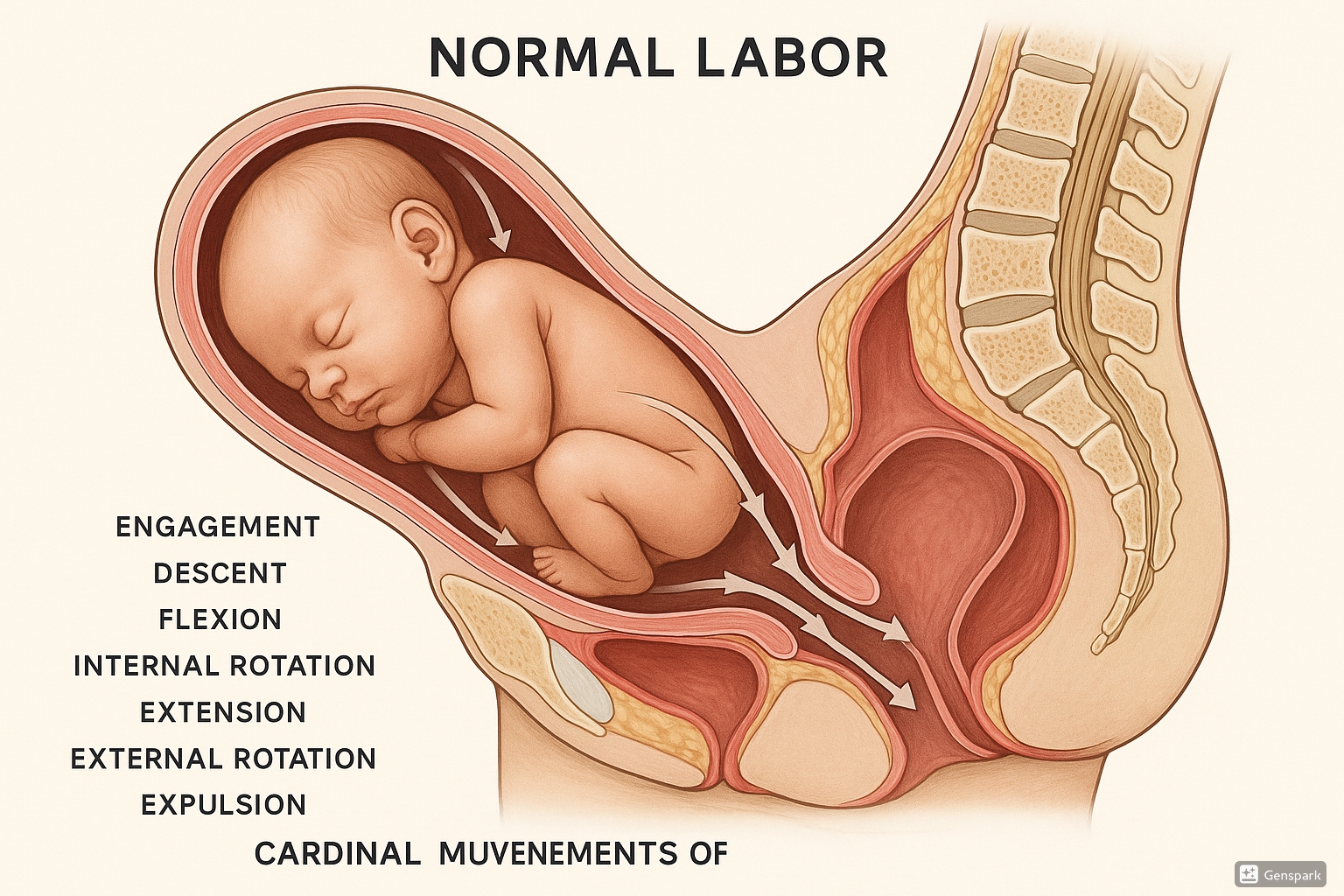
Figure 1: Cardinal Movements of Normal Labor showing the sequence of fetal positioning during birth.
| Movement | Description | Significance |
|---|---|---|
| 1. Engagement | The biparietal diameter of the fetal head passes through the pelvic inlet | Signals the beginning of the passage through the birth canal |
| 2. Descent | The progressive downward movement of the fetus through the pelvis | Occurs throughout labor but is most rapid during the second stage |
| 3. Flexion | The fetal chin tucks onto the chest, presenting the smallest diameter of the head | Optimizes the presenting part to navigate the pelvis |
| 4. Internal Rotation | The fetal head rotates from a transverse position to an anterior-posterior alignment | Aligns the widest part of the fetal head with the widest diameter of the pelvis |
| 5. Extension | The fetal head extends backward as it passes under the pubic symphysis | Allows delivery of the head through an upward curve around the pubic bone |
| 6. External Rotation (Restitution) |
After delivery of the head, it rotates back to align with the shoulders | Represents the natural alignment of the head with the shoulders |
| 7. Expulsion | Delivery of the shoulders and rest of the body | Completes the birth process |
Mnemonic: “EDFIERE”
- Engagement
- Descent
- Flexion
- Internal Rotation
- Extension
- Restitution/External Rotation
- Expulsion
Alternative mnemonic: “Every Day Fine Infants Enter Eager and Excited”
Assessment During Normal Labor
Initial Assessment
History
- Time of onset and pattern of contractions
- Status of membranes (intact or ruptured)
- Presence of bloody show or discharge
- Fetal movement
- Obstetric history (gravidity, parity, previous labor experiences)
- Medical and surgical history
- Allergies
- Medication history
- Birth plan and preferences
Physical Examination
- Vital signs: Temperature, pulse, respiration, blood pressure
- Abdominal examination: Leopold maneuvers to determine fetal lie, presentation, position, and engagement
- Uterine activity: Frequency, duration, and intensity of contractions
- Fetal assessment: Heart rate, position, presentation
- Vaginal examination: Cervical dilation, effacement, station, position, consistency
Ongoing Assessment During Labor
Maternal Assessment
| Parameter | First Stage | Second Stage | Third Stage | Fourth Stage |
|---|---|---|---|---|
| Blood Pressure | Every 1-4 hours | Every 30 minutes | Every 15 minutes | Every 15 minutes x4, then every 30 minutes x2 |
| Temperature | Every 4 hours | Every 4 hours | Once | Once |
| Pulse | Every 1-4 hours | Every 30 minutes | Every 15 minutes | Every 15 minutes x4, then every 30 minutes x2 |
| Contractions | Every 30-60 minutes | Every 15-30 minutes | N/A | N/A |
| Cervical Check | Every 2-4 hours or as needed | As needed | N/A | N/A |
| Uterine Fundus | N/A | N/A | After delivery | Every 15 minutes x4, then every 30 minutes x2 |
| Lochia | N/A | N/A | After delivery | Every 15 minutes x4, then every 30 minutes x2 |
Fetal Assessment
| Risk Status | First Stage | Second Stage |
|---|---|---|
| Low risk with intermittent auscultation | Every 30 minutes in active phase | Every 15 minutes |
| High risk or continuous EFM | Continuous monitoring | Continuous monitoring |
Documentation Guidelines
Document all assessments including:
- Maternal vital signs
- Contraction pattern (frequency, duration, intensity)
- Fetal heart rate patterns
- Cervical changes
- Fluid status (IV, oral intake, output)
- Pain level and management techniques used
- Emotional state
- Support persons present
- Interventions performed
Management of Normal Labor
General Principles
The management of normal labor focuses on supporting the physiological process while ensuring maternal and fetal well-being. The approach should respect the birthing person’s preferences while maintaining safety.
Key Principles
- Support the normal physiological process
- Avoid unnecessary interventions
- Provide continuous support
- Respect patient autonomy and preferences
- Maintain maternal and fetal safety
- Promote comfort and dignity
Management During First Stage
Latent Phase (0-6 cm)
- Encourage rest, hydration, and nutrition
- Support early ambulation and position changes
- Provide emotional support and information
- Offer non-pharmacological comfort measures
- Monitor maternal and fetal well-being
- Consider delaying admission to hospital until active labor if appropriate
Active Phase (6-10 cm)
- Continue support for ambulation and position changes
- Offer hydrotherapy if available and desired
- Provide continuous labor support
- Monitor for signs of progress and maternal/fetal well-being
- Offer pain management options as requested
- Maintain hydration (oral or IV as appropriate)
- Monitor bladder fullness and encourage voiding
Management During Second Stage
Positioning
Encourage upright or gravity-assisted positions when possible:
- Squatting
- Semi-sitting
- Side-lying
- Hands and knees
- Supported standing
Pushing Techniques
- Spontaneous pushing: Following the urge to push without specific direction
- Directed pushing: Instructing the patient to push during contractions (open-glottis pushing preferred over Valsalva maneuver)
- Delayed pushing: Waiting for the passive descent of the fetus before initiating active pushing efforts
Perineal Support
- Apply warm compresses to the perineum
- Perform perineal massage during contractions
- Provide perineal support during crowning (“hands-on” technique)
- Avoid routine episiotomy
Evidence-Based Practice: Warm compresses applied to the perineum during the second stage can reduce the risk of perineal trauma.
Management During Third Stage
Active Management
- Administration of uterotonic drugs (typically oxytocin 10 units IM or IV)
- Controlled cord traction with counter-pressure on the uterus
- Uterine massage after placental delivery
Expectant Management
- Await signs of placental separation
- Allow spontaneous delivery of the placenta with maternal effort
- Avoid cord traction
Cord Clamping
Delayed cord clamping (waiting 30-60 seconds before clamping) is recommended when maternal and neonatal condition permits.
Warning: A delay in placental delivery beyond 30 minutes increases the risk of postpartum hemorrhage and may indicate retention of placental fragments or undiagnosed placenta accreta spectrum.
Management During Fourth Stage
- Monitor vital signs per protocol
- Assess uterine tone, position, and lochia
- Facilitate skin-to-skin contact between parent and newborn
- Support early initiation of breastfeeding if desired
- Assess for perineal trauma and provide appropriate care
- Monitor for urinary retention and encourage early voiding
- Provide comfort measures for afterpains
- Administer any prescribed medications
Pain Management Options
Non-Pharmacological Methods
| Method | Description | Benefits |
|---|---|---|
| Breathing techniques | Patterned breathing to promote relaxation and distraction | No side effects; can be used throughout labor; promotes oxygenation |
| Hydrotherapy | Immersion in warm water (shower or tub) | Reduces pain perception; promotes relaxation; may shorten first stage |
| Massage | Therapeutic touch to relieve tension | Reduces pain; promotes relaxation; enhances partner involvement |
| Heat and cold therapy | Application of warm packs or cold compresses | Reduces discomfort; easy to apply; no side effects |
| TENS unit | Transcutaneous electrical nerve stimulation | Non-invasive; patient-controlled; minimal side effects |
| Sterile water injections | Intradermal injections at four points around sacrum | Effective for back labor; lasts 60-90 minutes |
| Acupuncture/Acupressure | Stimulation of specific points to relieve pain | Minimal side effects; may reduce need for pharmacological interventions |
| Visualization/Hypnosis | Mental techniques to alter pain perception | Promotes relaxation; enhances sense of control |
Pharmacological Methods
| Method | Description | Benefits | Considerations |
|---|---|---|---|
| Epidural analgesia | Local anesthetic delivered into epidural space | Most effective pain relief; allows for rest; can be used for cesarean if needed | May prolong second stage; may require bladder catheterization; possibility of hypotension |
| Spinal analgesia | Single injection of anesthetic into subarachnoid space | Rapid onset; effective pain relief | Limited duration; risk of post-dural puncture headache |
| Combined spinal-epidural | Combination of spinal and epidural techniques | Rapid onset with ability to continue as needed | Higher technical difficulty; same risks as individual methods |
| Nitrous oxide | Inhaled analgesic gas | Self-administered; rapid onset and offset; minimal systemic effects | Less effective than neuraxial methods; may cause nausea, dizziness |
| Parenteral opioids | Intravenous or intramuscular pain medications | Option when neuraxial methods unavailable; easy administration | Limited efficacy; maternal and neonatal side effects; timing restrictions near delivery |
| Pudendal block | Local anesthetic injected near pudendal nerves | Effective for perineal pain during second stage | Does not relieve contraction pain; requires skilled provider |
Decision-Making Factors: Choice of pain management should consider:
- Patient preference and birth plan
- Stage and progress of labor
- Medical history and contraindications
- Available resources and provider skills
- Potential impact on labor progress and maternal-fetal well-being
Potential Complications
Even in normal labor, healthcare providers must remain vigilant for potential complications that may arise:
Maternal Complications
| Complication | Warning Signs | Preventive Measures |
|---|---|---|
| Postpartum hemorrhage | Excessive bleeding, uterine atony, tachycardia, hypotension | Active management of third stage, monitoring uterine tone |
| Genital tract trauma | Lacerations, hematoma formation, pain disproportionate to delivery | Controlled delivery, perineal support, selective episiotomy |
| Uterine rupture | Sudden severe pain, fetal distress, vaginal bleeding, loss of contraction pattern | Appropriate management of labor in patients with uterine scar |
| Amniotic fluid embolism | Sudden respiratory distress, cardiovascular collapse, DIC | Recognition and rapid response to symptoms |
| Retained placenta | Failure of placenta to deliver within 30 minutes | Assessment for complete placental delivery |
Fetal/Neonatal Complications
| Complication | Warning Signs | Preventive Measures |
|---|---|---|
| Fetal distress | Abnormal fetal heart rate patterns, meconium-stained fluid | Regular fetal monitoring, prompt intervention for concerning patterns |
| Shoulder dystocia | Difficulty delivering shoulders after head delivery | Recognition of risk factors, preparation for maneuvers |
| Umbilical cord prolapse | Palpable cord in vagina, sudden fetal bradycardia | Careful membrane rupture, prompt recognition and management |
| Birth injuries | Bruising, cephalohematoma, fractured clavicle | Controlled delivery, appropriate maternal positioning |
| Neonatal respiratory distress | Poor APGAR scores, respiratory effort, cyanosis | Preparation for neonatal resuscitation |
Early Recognition: Prompt identification of deviations from normal labor patterns is essential for timely intervention and prevention of serious complications.
Mnemonics for Learning
Stages of Labor: “DPPR”
- Dilation (First Stage)
- Pushing (Second Stage)
- Placenta (Third Stage)
- Recovery (Fourth Stage)
Cardinal Movements: “EDFIERE”
- Engagement
- Descent
- Flexion
- Internal rotation
- Extension
- Restitution/External rotation
- Expulsion
Assessment of Labor: “ALPPPS”
- Attitude
- Lie
- Presentation
- Presenting part
- Position
- Station
Signs of Placental Separation: “CUGEL”
- Cord lengthening
- Uterus becomes globular
- Gush of blood
- Easy to palpate (fundus)
- Lighter uterus rises in abdomen
Understanding Labor Pain: “PAIN”
- Purposeful
- Anticipated
- Intermittent
- Normal
Conclusion
Normal labor is a complex physiological process that requires knowledgeable and supportive care from healthcare providers. Understanding the stages of normal labor, cardinal movements, assessment techniques, and appropriate management strategies is essential for nursing students to provide safe and effective care.
By recognizing the normal progress of labor, nurses can detect deviations early, collaborate with the interprofessional team, and implement appropriate interventions. Supporting patients through normal labor also involves respecting their preferences, providing comfort measures, and creating a positive birth experience.
The knowledge gained from these comprehensive notes will help nursing students develop the clinical skills and critical thinking necessary to provide high-quality care during one of the most significant events in a person’s life—the birth of their child.
References
- American College of Obstetricians and Gynecologists. (2019). ACOG Practice Bulletin No. 211: Critical care in pregnancy. Obstetrics & Gynecology.
- Bohren, M. A., Hofmeyr, G. J., Sakala, C., Fukuzawa, R. K., & Cuthbert, A. (2017). Continuous support for women during childbirth. Cochrane Database of Systematic Reviews.
- National Institute for Health and Care Excellence. (2017). Intrapartum care for healthy women and babies. Clinical guideline [CG190].
- King, T. L., Brucker, M. C., Kriebs, J. M., Fahey, J. O., Gegor, C. L., & Varney, H. (2015). Varney’s midwifery (5th ed.). Jones & Bartlett Learning.
- Lothian, J. A. (2009). Safe, healthy birth: What every pregnant woman needs to know. The Journal of Perinatal Education, 18(3), 48-54.
- World Health Organization. (2018). WHO recommendations: Intrapartum care for a positive childbirth experience.
- Zhang, J., Landy, H. J., Branch, D. W., Burkman, R., Haberman, S., Gregory, K. D., Hatjis, C. G., Ramirez, M. M., Bailit, J. L., Gonzalez-Quintero, V. H., Hibbard, J. U., Hoffman, M. K., Kominiarek, M., Learman, L. A., Van Veldhuisen, P., Troendle, J., & Reddy, U. M. (2010). Contemporary patterns of spontaneous labor with normal neonatal outcomes. Obstetrics and Gynecology, 116(6), 1281-1287.
