Normal Puerperium: Physiology and Duration
Comprehensive notes for nursing students
Table of Contents
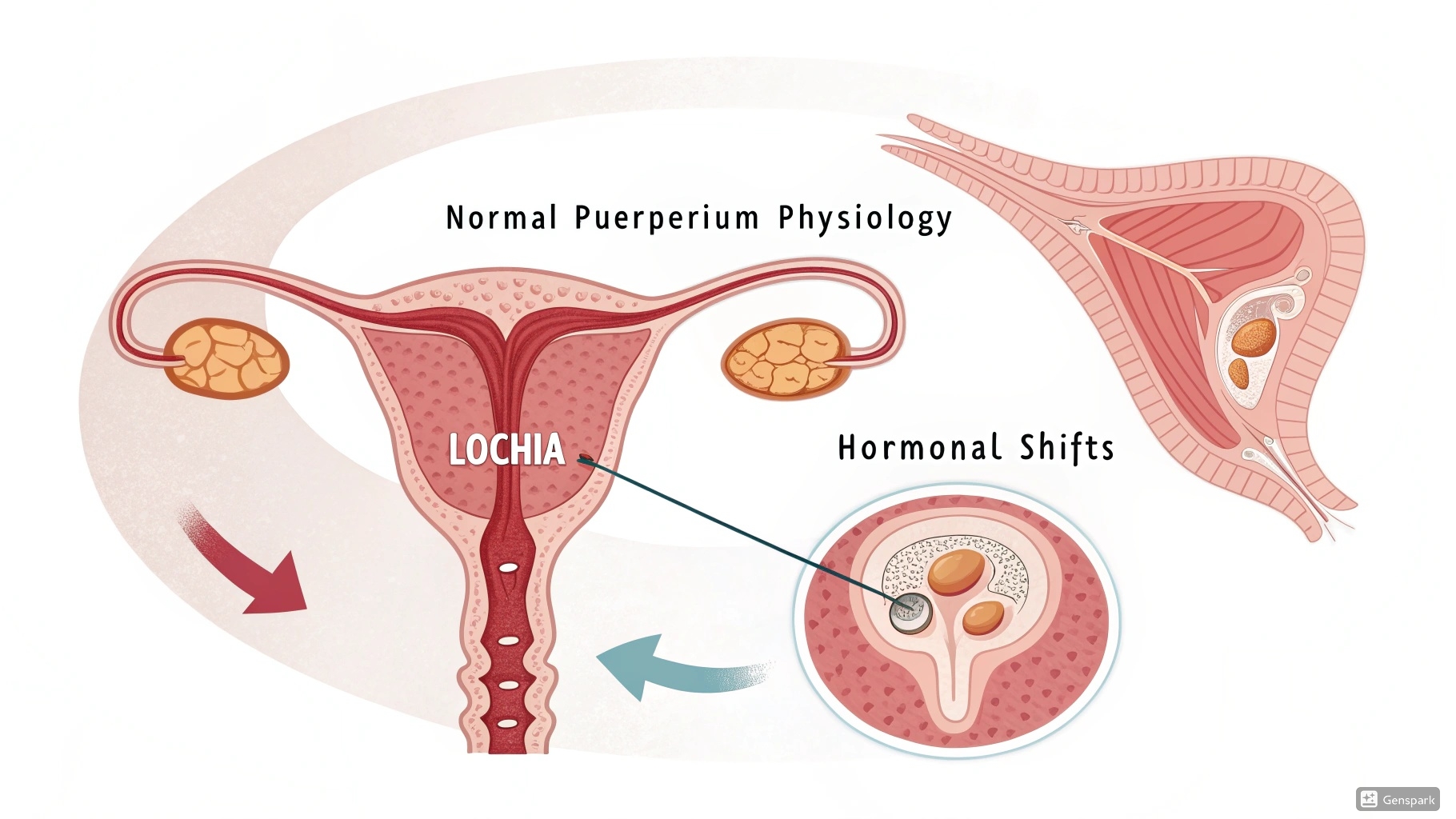
Normal puerperium physiological changes illustration
Definition and Duration of Normal Puerperium
Puerperium is the period following childbirth during which the maternal body returns to its non-pregnant state. It begins immediately after the delivery of the placenta and typically lasts for 6 weeks.
During this time, significant physiological and anatomical changes occur as the woman’s body recovers from pregnancy and prepares for lactation. Although traditionally defined as 6 weeks, the complete resolution of all pregnancy-induced changes may take up to 12 weeks or longer for some systems.
Memory Aid: “6-6-6 Rule”
Remember the duration and key changes with the 6-6-6 rule:
- 6 hours: Immediate postpartum period (critical monitoring)
- 6 days: Early puerperium (rapid physiological changes)
- 6 weeks: Complete puerperium (return to non-pregnant state)
Reproductive System Changes
Uterine Involution
Uterine involution is the process by which the uterus returns to its pre-pregnancy size and condition. This remarkable transformation involves both a reduction in size (from approximately 1000g to 50-100g) and structural reorganization.
| Time After Delivery | Uterine Fundal Height | Clinical Assessment |
|---|---|---|
| Immediately after delivery | At umbilicus level | Firm, midline position |
| 24 hours | 1 cm below umbilicus | Firm on palpation |
| Day 2-3 | 2-3 cm below umbilicus | Should remain firm and midline |
| Day 5-7 | Halfway between umbilicus and symphysis pubis | Beginning to descend into pelvis |
| Day 10 | At symphysis pubis | Difficult to palpate abdominally |
| By week 6 | Returns to non-pregnant size | Not palpable abdominally |
The rapid decrease in uterine size occurs primarily through autolysis (self-digestion) of excess tissue. The myometrial cells do not decrease in number but rather decrease dramatically in size. This process is driven by the withdrawal of estrogen and progesterone after placental delivery.
Memory Aid: “The Descending Fundus”
To remember the rate of uterine involution, think:
- The uterine fundus descends approximately 1 finger-breadth (1 cm) per day
- By day 10, it should no longer be palpable abdominally
- Mnemonic: U-DROP (Uterus Descends Rapidly: One-finger Per day)
Lochia
Lochia is the vaginal discharge that occurs after childbirth, consisting of blood, mucus, and uterine tissue. The characteristics of lochia change over time and are important clinical indicators of normal healing.
Lochia Rubra
Days 1-3: Red, primarily blood with some fetal membranes, decidua, vernix, and meconium. Flow is moderate to heavy, similar to a menstrual period. Small clots may be present but should not be larger than a plum.
Lochia Serosa
Days 4-10: Pinkish-brown to pale brown discharge. Contains serous fluid, erythrocytes, leukocytes, cervical mucus, and microorganisms. Flow is light to moderate.
Lochia Alba
Days 10-14 to week 6: Yellowish-white or creamy discharge. Primarily composed of leukocytes, decidua, epithelial cells, fat, cervical mucus, and bacteria. Flow is scanty.
Clinical Alert:
Abnormal lochia characteristics that require immediate assessment include:
- Bright red bleeding beyond day 3-4
- Large clots (larger than a plum)
- Foul-smelling discharge (indication of infection)
- Sudden increase in amount of bleeding
- Return of bright red bleeding after it had changed to serosa or alba
Memory Aid: “The Colors of Recovery”
Remember lochia progression using the colors of a traffic light (backward):
- Red (Rubra) – Stop and rest (Days 1-3)
- Yellow/Pink (Serosa) – Proceed with caution (Days 4-10)
- White (Alba) – Good to go (Days 10+ to week 6)
Cervix and Vagina
The cervix and vagina undergo significant changes during puerperium:
Cervical Changes
- Immediately after birth, the cervix is soft, edematous, and may have small lacerations
- By 1 week, the external os narrows to admit one finger (previously dilated to 10cm)
- By 3 weeks, the cervix has regained its firmness
- The cervical canal remains slightly wider than pre-pregnancy
- The external os changes from circular (nulliparous) to a transverse slit (multiparous)
Vaginal Changes
- Initially, the vagina is edematous, hyperemic, and lacks rugae
- Gradual reduction in size occurs over 3 weeks
- Rugae reappear by week 3, but never fully return to nulliparous state
- The hymen is permanently changed, appearing as irregular tags called carunculae myrtiformes
- Full epithelialization takes approximately 6 weeks
- Estrogen deficiency may cause vaginal dryness, especially in breastfeeding mothers
Hormonal Changes
The postpartum period involves dramatic hormonal shifts that affect multiple body systems. The removal of the placenta triggers most of these changes.
| Hormone | Change During Puerperium | Physiological Effects |
|---|---|---|
| Estrogen | Sharp drop after placenta delivery, reaching pre-pregnancy levels by day 5 | – Vaginal epithelium changes – May contribute to postpartum blues – Reduced impact on fluid retention |
| Progesterone | Rapid decline after placenta delivery | – Allows uterine contractions – Enables lactation initiation – Decreased body temperature |
| Prolactin | Increases significantly in breastfeeding mothers | – Stimulates milk production – Suppresses ovulation in breastfeeding mothers – Peaks during night feedings |
| Oxytocin | Released during nipple stimulation | – Causes milk ejection (let-down) – Promotes uterine contractions – May enhance maternal bonding |
| Human Placental Lactogen | Disappears after placenta removal | – Insulin resistance resolves – Blood glucose regulation normalizes |
| Human Chorionic Gonadotropin (hCG) | Rapid decline, undetectable by day 14 | – Pregnancy tests become negative – Corpus luteum regression |
Memory Aid: “PROPE” for Puerperal Hormonal Changes
Placenta removal leads to:
- Progesterone plummets
- Rapid estrogen reduction
- Oxytocin oscillates with breastfeeding
- Prolactin peaks for milk production
- Elimination of hPL and hCG
Cardiovascular Changes
The cardiovascular system undergoes significant adjustments during the puerperium as it returns to the pre-pregnancy state.
- Cardiac Output: Initially elevated by up to 80% above pre-labor values immediately after birth, gradually decreases over 2-3 weeks, but may take up to 24 weeks to fully normalize
- Blood Volume: Rapid diuresis reduces blood volume by 1000-1500 mL in the first week
- Blood Pressure: Usually normal but may be temporarily elevated due to pain or anxiety
- Heart Rate: May be elevated for the first 24 hours, then returns to pre-pregnancy levels
- Peripheral Vascular Resistance: Remains elevated at 6 weeks postpartum compared to pre-pregnancy values
- Venous System: Gradual resolution of pregnancy-related venous dilation and increased risk of thrombosis in the immediate postpartum period
Clinical Consideration: Orthostatic Hypotension
The rapid fluid shifts in early puerperium can predispose women to orthostatic hypotension, especially upon first ambulation after delivery. Nurses should monitor vital signs and assist with first ambulation to prevent falls.
Venous Thromboembolism Risk
The postpartum period carries a 5-fold increased risk of venous thromboembolism compared to pregnancy, with highest risk in the first 3 weeks. Early ambulation and proper hydration are crucial preventive measures.
Other Body Systems
Urinary System
- Diuresis: Significant diuresis occurs in the first 2-5 days as the body eliminates excess fluid and sodium retained during pregnancy
- Bladder Capacity: Increased immediately after birth due to decreased tone and sensation
- Urinary Retention: Common in the first 24 hours due to perineal edema, pain, or effects of anesthesia
- Glucosuria: Resolves within days as renal threshold for glucose returns to normal
- Renal Function: Glomerular filtration rate returns to normal by 6 weeks
- Urinary Tract Infections: Increased risk due to catheterization, trauma, and urinary stasis
Clinical Tip:
Ensure first void within 6-8 hours after delivery. Volume should be at least 150-200 mL. Document time and amount.
Gastrointestinal System
- Appetite: Often increased, especially in breastfeeding mothers
- Constipation: Common due to decreased intestinal tone, dehydration, perineal pain, and fear of straining
- Hemorrhoids: May persist or develop due to pushing during labor
- Abdominal Wall: Muscle tone gradually returns, but diastasis recti may persist
Memory Aid: “BOWEL”
For addressing gastrointestinal issues postpartum:
- Bulk – Increase dietary fiber
- Orange juice and hydration – Fluids help prevent constipation
- Walking – Early ambulation stimulates peristalsis
- Emotional support – Reduce anxiety about first bowel movement
- Laxatives as needed – Stool softeners may be indicated
Musculoskeletal System
- Ligaments and Joints: Gradually regain pre-pregnancy stability as relaxin levels decrease
- Abdominal Muscles: Stretched during pregnancy, may take 6-8 weeks to regain tone
- Diastasis Recti: Separation of the rectus abdominis muscles may persist in some women
- Pelvic Floor: May be weakened, especially after vaginal delivery
- Weight Loss: Initial 5-6 kg loss from baby, placenta, amniotic fluid; additional 2-3 kg in the first week from fluid loss
Lactation
Lactation is a significant physiological process during puerperium that involves complex hormonal regulation.
Stages of Lactation
Lactogenesis I
Mid-pregnancy to 2 days postpartum: Mammary gland development and initial colostrum production. The high levels of progesterone during pregnancy inhibit milk production despite increasing prolactin.
Lactogenesis II
Days 2-5 postpartum: “Milk coming in.” Triggered by the drop in progesterone after placenta delivery, while prolactin levels remain high. Characterized by breast fullness, increased vascular flow, and transition from colostrum to mature milk.
Lactogenesis III (Galactopoiesis)
Day 5 to weaning: Maintained milk production. Regulated primarily by infant suckling and demand, which stimulates prolactin release. Emptying the breast stimulates further milk production.
Hormonal Regulation of Lactation
Two primary processes are involved in lactation:
- Milk Production: Controlled by prolactin
- Milk Ejection (Let-down): Controlled by oxytocin
The Milk Ejection Reflex
When the baby suckles:
- Sensory nerve endings in nipple are stimulated
- Signals travel to hypothalamus
- Posterior pituitary releases oxytocin
- Oxytocin causes myoepithelial cells contraction
- Milk is pushed from alveoli into ducts
- Milk becomes available to infant
This reflex can be inhibited by stress, anxiety, or pain, highlighting the importance of a calm environment for breastfeeding.
Stages of Puerperium
The puerperium period can be divided into three distinct phases, each with its own clinical significance:
| Stage | Duration | Key Physiological Events | Nursing Focus |
|---|---|---|---|
| Immediate Puerperium | First 24 hours | – Rapid hemodynamic changes – Initial uterine involution – Risk of hemorrhage – Onset of lochia rubra |
– Vital sign monitoring – Uterine tone assessment – Bleeding assessment – Pain management – First void monitoring |
| Early Puerperium | Days 2-7 | – Diuresis – Lactogenesis II – Transition to lochia serosa – Progressive uterine involution |
– Breastfeeding support – Perineal care – Ambulation promotion – Self-care education – Emotional support |
| Late Puerperium | Week 2 to week 6 | – Complete uterine involution – Lochia alba and cessation – Hormonal stabilization – Return of ovulation (variable) |
– Postpartum follow-up – Activity resumption guidance – Contraception counseling – Mental health screening – Ongoing breastfeeding support |
Memory Aid: “The 3 Rs of Puerperal Stages”
- React: Immediate puerperium – Body reacts to birth with rapid physiological changes
- Rebound: Early puerperium – Systems rebound with diuresis, milk production
- Restore: Late puerperium – Complete restoration to non-pregnant state
Nursing Management during Puerperium
Comprehensive nursing care during the puerperium focuses on monitoring physiological adaptation, preventing complications, supporting lactation, and promoting maternal-infant bonding.
Assessment and Monitoring
- Vital Signs: Monitor temperature, pulse, respirations, and blood pressure regularly during the immediate postpartum period
- Fundal Assessment: Check uterine tone, position, and height regularly
- Lochia: Assess amount, color, and odor
- Perineum: Assess for edema, ecchymosis, discharge, and pain
- Breasts: Assess for engorgement, nipple condition, and effective breastfeeding
- Elimination: Monitor first void and bowel movement
- Lower Extremities: Check for edema, Homans’ sign, and pain
- Emotional Status: Assess for signs of postpartum blues or depression
BUBBLE-HE Assessment Mnemonic
Use this mnemonic for comprehensive postpartum assessment:
- Breasts
- Uterus
- Bladder
- Bowels
- Lochia
- Episiotomy (or perineum)
- Homans’ sign
- Emotional status
Interventions
Physical Care
- Promote comfort with appropriate pain management
- Teach perineal care and hygiene measures
- Encourage early ambulation to prevent complications
- Support adequate rest and nutrition
- Provide ice packs for perineal edema
- Administer prescribed medications
Lactation Support
- Assist with positioning and latch
- Educate on breast care and milk expression
- Manage engorgement and nipple soreness
- Support feeding frequency and duration
- Provide resources for continued support
Education
- Postpartum recovery expectations
- Warning signs requiring medical attention
- Self-care practices and activity restrictions
- Newborn care basics
- Family planning and contraception options
Psychosocial Support
- Promote maternal-infant bonding
- Assess for postpartum mood disorders
- Include partner/family in education
- Provide information on community resources
- Support adjustment to parenting role
Postpartum Warning Signs – “REDS”
Teach mothers to seek immediate care for:
- R – Red flag bleeding (soaking a pad within an hour)
- E – Edema and extreme pain in legs
- D – Dizziness, visual changes, severe headache
- S – Signs of infection (fever ≥100.4°F, foul odor, severe pain)
Best Practices and Recent Updates
Contemporary nursing care has evolved to incorporate evidence-based practices and updated guidelines for postpartum care.
1. Postpartum Care as a Continuum
The American College of Obstetricians and Gynecologists (ACOG) now recommends that postpartum care should be an ongoing process rather than a single encounter, with services tailored to each woman’s individual needs.
- Initial assessment within 3 weeks postpartum
- Ongoing care as needed
- Comprehensive visit no later than 12 weeks after birth
- Development of a postpartum care plan during pregnancy
2. Enhanced Postpartum Depression Screening
Current guidelines emphasize universal screening for depression and anxiety during the comprehensive postpartum visit, with earlier screening if concerning symptoms arise.
- Use validated tools like Edinburgh Postnatal Depression Scale (EPDS)
- Implement screening protocols with clear referral pathways
- Consider cultural factors affecting mental health reporting
- Include assessment for anxiety disorders, which may be equally prevalent
3. Quantitative Blood Loss Assessment
Moving away from subjective assessment of postpartum blood loss to more accurate quantitative measurement:
- Implementation of calibrated drapes and weighing of materials
- Earlier identification of excessive bleeding
- Standardized responses based on measured blood loss
- Integration of measurement into electronic health records
- Reduction in maternal morbidity through earlier intervention
