Comprehensive Nursing Care Plan for Gastric Gavage
Evidence-Based Approach to Enteral Nutrition Management
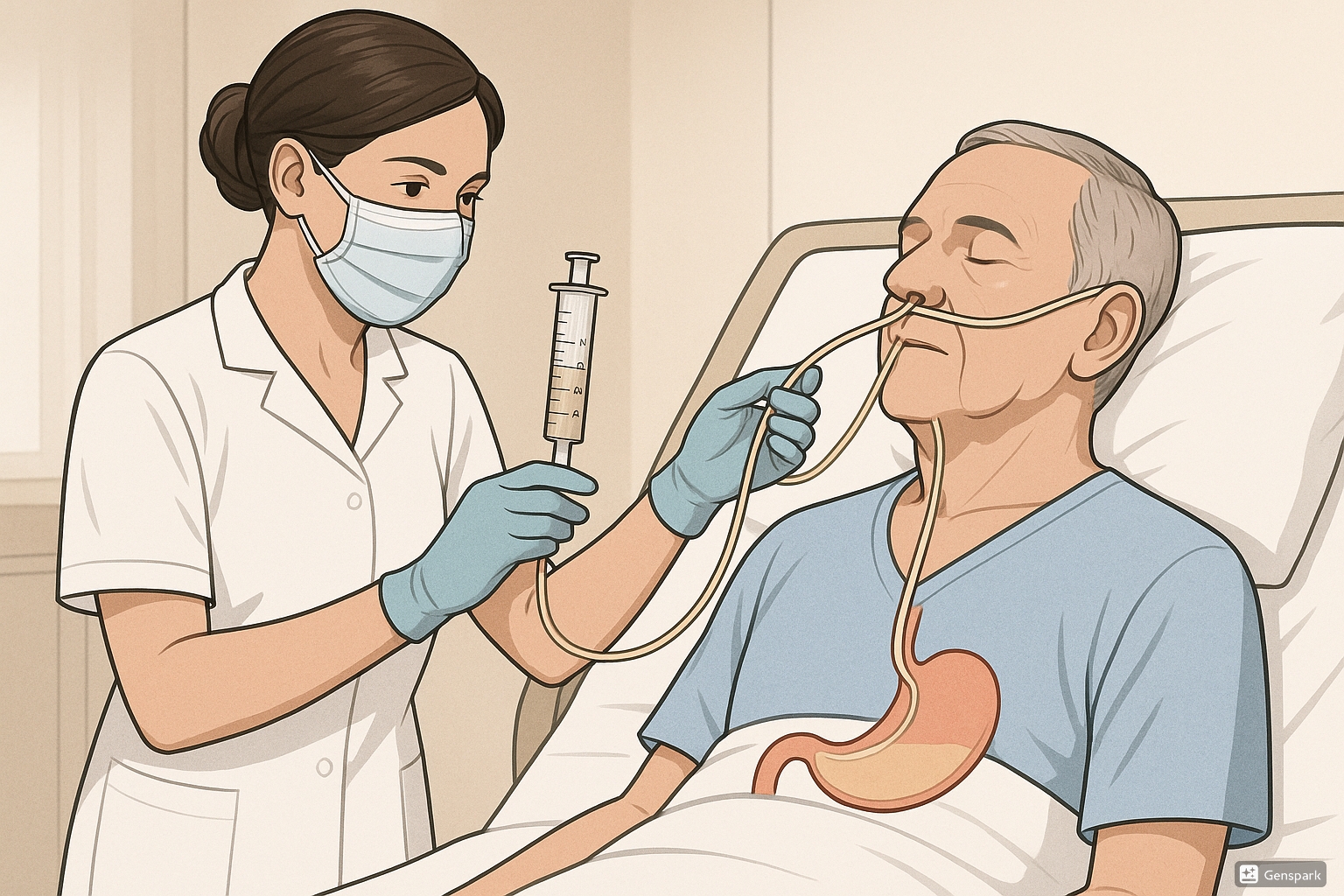
Medical illustration showing gastric gavage feeding procedure with a nurse administering feeding through a nasogastric tube
Table of Contents
Introduction to Gastric Gavage
The nursing care plan for gastric gavage is essential for healthcare professionals to deliver safe, effective, and holistic care to patients requiring this feeding method. Gastric gavage is a fundamental nursing procedure that involves delivering nutritional substances directly into a patient’s stomach via a feeding tube. This method is primarily used when oral feeding is not possible or insufficient for meeting the patient’s nutritional needs.
As nursing professionals, understanding the comprehensive approach to gastric gavage administration is crucial for preventing complications, promoting patient comfort, and ensuring optimal nutritional outcomes. This document provides a detailed nursing care plan for gastric gavage that covers the entire process from assessment to evaluation.
Definition and Purpose of Gastric Gavage
Gastric gavage is defined as the process of delivering nutritional substances via a small tube directly into the stomach, bypassing the normal oral-pharyngeal route of feeding. It is a means of alimentation when the oral route is inaccessible or inadequate.
Key Purposes of Gastric Gavage:
- Provide essential nutrition to patients who cannot eat orally
- Maintain or improve nutritional status in compromised patients
- Deliver medications when oral administration is not possible
- Support growth and development in premature infants
- Prevent malnutrition in patients with prolonged inability to consume food orally
Developing a nursing care plan for gastric gavage requires an understanding of the anatomy and physiology of the gastrointestinal system, as well as the principles of enteral nutrition and the potential complications that may arise during the procedure.
Indications and Contraindications
Indications for Gastric Gavage
- Gastrointestinal diseases and surgeries that prevent normal feeding
- Hypermetabolic states (burns, multiple trauma, sepsis, cancer)
- Neurological disorders affecting swallowing (stroke, coma)
- Post-surgical care (head and neck, esophagus)
- Premature infants with underdeveloped sucking reflex
- Unconscious patients requiring nutritional support
- Severe facial trauma affecting oral intake
- Mechanical ventilation requiring bypassing of oral route
Contraindications for Gastric Gavage
- Absent bowel sounds (indicating paralytic ileus)
- Intestinal obstruction
- Severe gastrointestinal bleeding
- Intractable vomiting
- Peritonitis
- Recent gastrointestinal anastomosis
- Severe pancreatitis
- Hemodynamic instability requiring vasopressor support
Equipment Needed for Gastric Gavage
| Equipment | Purpose |
|---|---|
| Feeding formula | Provides necessary nutrients to the patient |
| Nasogastric tube (appropriate size) | Delivers feeding directly to the stomach |
| Calibrated feeding container | Measures and holds the feeding formula |
| Asepto syringe or Toomey syringe | For administering feeding and checking residual volume |
| Feeding pump (if using continuous feeding) | Regulates the rate of feeding administration |
| pH testing strips | Verifies tube placement in the stomach |
| Stethoscope | Auscultates for placement verification and bowel sounds |
| Clean gloves | Maintains aseptic technique during procedure |
| Water for flushing | Clears tube before and after feeding |
| Tape or tube securing device | Secures tube to prevent displacement |
| Lubricant (water-soluble) | Facilitates tube insertion if needed |
| Towel or absorbent pad | Protects patient and bedding from spills |
Proper preparation of equipment is a critical component of a comprehensive nursing care plan for gastric gavage. All equipment should be assembled and checked before beginning the procedure to ensure efficiency and patient safety.
Nursing Diagnoses and Care Plans
The following section outlines 12 key nursing diagnoses relevant to patients receiving gastric gavage feeding. Each diagnosis includes assessment data, nursing interventions with rationales, and expected outcomes to guide comprehensive care delivery.
1. Risk for Aspiration
Definition/Related Factors:
Vulnerable to entry of gastrointestinal secretions, oropharyngeal secretions, solids, or fluids into the tracheobronchial passages due to dysfunction or absence of normal protective mechanisms, related to presence of feeding tube and impaired swallowing reflexes.
Assessment Data:
- Verify tube placement before each feeding
- Assess residual gastric contents
- Evaluate level of consciousness
- Auscultate lung sounds for abnormal breath sounds
- Monitor respiratory rate and pattern
- Assess presence of gag reflex and ability to swallow
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Confirm tube placement before each feeding by checking pH of aspirate (should be 1-5.5) or using institutional protocol. | Ensures the tube is properly positioned in the stomach to prevent inadvertent administration into the lungs. |
| Elevate the head of the bed 30-45 degrees during and for 30-60 minutes after feeding. | Reduces risk of reflux and minimizes possibility of aspiration using gravity. |
| Check gastric residual volume before intermittent feedings. Hold feeding if residual exceeds institutional guidelines (typically 200-250 mL or 50% of previous feeding). | High residual volumes indicate delayed gastric emptying and increase risk for regurgitation and aspiration. |
| Maintain cuff inflation on endotracheal or tracheostomy tubes if present. | Provides barrier protection to help prevent aspiration around the artificial airway. |
| Keep suction equipment readily available at bedside. | Allows for prompt intervention if aspiration occurs. |
| Administer prescribed antiemetics if nausea or vomiting present. | Reduces risk of vomiting which can lead to aspiration. |
Expected Outcomes:
- Patient will demonstrate clear lung fields with normal breath sounds
- Patient will maintain normal respiratory rate and pattern
- Patient will not exhibit signs of respiratory distress
- Patient will not develop aspiration pneumonia
2. Imbalanced Nutrition: Less than Body Requirements
Definition/Related Factors:
Intake of nutrients insufficient to meet metabolic needs, related to inability to ingest food orally due to neuromuscular impairment, dysphagia, or decreased level of consciousness.
Assessment Data:
- Monitor weight trends (daily or weekly as appropriate)
- Assess laboratory values (protein, albumin, prealbumin, electrolytes)
- Evaluate skin turgor and mucous membranes
- Monitor intake and output
- Assess for edema or dehydration
- Evaluate tolerance to enteral feeding
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Collaborate with dietitian to determine appropriate formula and caloric requirements. | Ensures nutritional needs are met based on individual patient requirements and condition. |
| Administer enteral feeding as prescribed (continuous, intermittent, or bolus). | Provides consistent delivery of nutrients based on patient’s tolerance and metabolic needs. |
| Monitor and document tolerance to feeding (absence of nausea, vomiting, diarrhea, abdominal distension). | Early identification of intolerance allows for prompt intervention and formula adjustment. |
| Weigh patient at same time daily or weekly using same scale and clothing conditions. | Provides consistent measurement to evaluate effectiveness of nutritional support. |
| Monitor laboratory values and report significant changes. | Helps evaluate nutritional status and effectiveness of the feeding regimen. |
| Administer tube feedings at room temperature. | Cold feedings may cause cramping and discomfort. |
Expected Outcomes:
- Patient will maintain or achieve weight within target range
- Patient will demonstrate improved or stabilized lab values
- Patient will tolerate prescribed feeding regimen without complications
- Patient will show no signs of malnutrition
3. Risk for Impaired Skin Integrity
Definition/Related Factors:
Vulnerable to alteration in epidermis and/or dermis, related to external factors such as pressure from tube, adhesive tape, or mechanical factors at insertion site.
Assessment Data:
- Inspect nares and tube entry site for signs of irritation or breakdown
- Assess the facial skin where tube is secured
- Evaluate for any drainage or discharge at insertion site
- Check for signs of pressure areas around tube placement
- Monitor nutritional status that may affect skin healing
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Clean nares and tube insertion site daily with mild soap and water. | Removes secretions and debris that can irritate skin. |
| Rotate nasogastric tube to opposite naris every 24-48 hours per facility policy. | Prevents pressure necrosis in one area. |
| Use hypoallergenic tape or commercial tube securing device. | Reduces risk of adhesive-related skin damage while maintaining tube position. |
| Reposition tape or tube holder daily and assess skin underneath. | Allows evaluation of skin condition and relieves pressure on the same area. |
| Apply water-soluble lubricant to nares if dryness or irritation is present. | Maintains moisture and reduces friction. |
| For gastrostomy or jejunostomy tubes, clean skin around stoma site with mild soap and water, pat dry, and apply barrier cream as needed. | Prevents irritation from gastric secretions and promotes skin integrity around stoma site. |
Expected Outcomes:
- Patient will maintain intact skin at tube insertion site and surrounding areas
- Patient will not develop pressure ulcers or skin breakdown related to tube placement
- If skin irritation occurs, it will resolve promptly with interventions
4. Risk for Infection
Definition/Related Factors:
Vulnerable to invasion and multiplication of pathogenic organisms, related to break in skin integrity from tube insertion, contaminated equipment, or formula.
Assessment Data:
- Monitor temperature and vital signs
- Assess insertion site for redness, swelling, warmth, or discharge
- Evaluate formula storage and preparation practices
- Check equipment cleanliness
- Monitor for systemic signs of infection
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Perform hand hygiene before handling tube, feeding equipment, or formula. | Reduces transmission of microorganisms. |
| Use aseptic technique when preparing formula and administering feedings. | Minimizes risk of contamination. |
| Discard opened formula after recommended time period (typically 24 hours for continuous feeding systems or 4 hours at room temperature). | Prevents bacterial growth in formula. |
| Change feeding administration sets according to facility policy (typically every 24 hours). | Reduces buildup of formula residue and bacterial colonization. |
| Store unopened formula in cool, dry place. Refrigerate opened formula and check expiration dates. | Proper storage prevents contamination and bacterial growth. |
| Clean stoma site for gastrostomy tubes daily and as needed using circular motion from center outward. | Removes exudate and microorganisms, moving from cleaner to less clean areas. |
Expected Outcomes:
- Patient will remain free from signs and symptoms of infection
- Tube insertion site will remain clean without signs of infection
- Patient will maintain normal temperature and vital signs
- Feeding equipment will remain clean and free from contamination
5. Deficient Knowledge
Definition/Related Factors:
Absence or deficiency of cognitive information related to gastric gavage feeding, care of feeding tube, monitoring for complications, or home care management.
Assessment Data:
- Assess patient’s and caregiver’s current knowledge of gastric gavage
- Evaluate learning needs and preferred learning style
- Determine patient’s/caregiver’s readiness and ability to learn
- Assess language, literacy, and cultural considerations
- Identify barriers to learning
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Provide clear, concise information about the purpose and process of gastric gavage feeding. | Helps patient/caregiver understand the necessity and benefits of the procedure. |
| Demonstrate feeding technique and tube care using return demonstration method. | Hands-on practice enhances learning and builds confidence in performing the procedure. |
| Provide written instructions with pictures in the patient’s preferred language. | Reinforces verbal teaching and serves as a reference after discharge. |
| Teach signs and symptoms of complications that require medical attention. | Enables early recognition and prompt treatment of potential problems. |
| Instruct on proper formula preparation, storage, and administration. | Ensures safe handling of feeding formula to prevent contamination and infection. |
| Provide information about community resources and support services. | Connects patient/caregiver with additional assistance and resources for ongoing care. |
Expected Outcomes:
- Patient/caregiver will verbalize understanding of gastric gavage purpose and procedure
- Patient/caregiver will demonstrate correct technique for administering tube feeding
- Patient/caregiver will identify signs and symptoms requiring medical attention
- Patient/caregiver will verbalize knowledge of proper formula handling and tube care
6. Anxiety
Definition/Related Factors:
Vague uneasy feeling of discomfort or dread accompanied by an autonomic response, related to unfamiliar equipment, fear of aspiration, body image change from tube placement, or uncertainty about feeding procedure.
Assessment Data:
- Assess verbal and nonverbal signs of anxiety
- Evaluate physiological responses (increased heart rate, respirations, blood pressure)
- Note expressions of fear or concern about the feeding tube
- Identify coping mechanisms
- Assess impact on sleep, appetite, and daily activities
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Establish a trusting relationship through consistent care and open communication. | Creates a safe environment for the patient to express concerns and ask questions. |
| Explain all procedures and equipment before beginning; provide sensory information about what patient will experience. | Reduces fear of the unknown and helps patient prepare for sensations during the procedure. |
| Encourage expression of feelings and concerns about tube feeding. | Validates the patient’s emotional response and provides opportunity for addressing specific fears. |
| Teach relaxation techniques such as deep breathing, guided imagery, or progressive muscle relaxation. | Provides coping strategies to reduce physical manifestations of anxiety. |
| Include patient in decision-making regarding feeding schedule when possible. | Increases sense of control and reduces feelings of helplessness. |
| Connect patient with others who have successfully managed tube feedings. | Peer support can normalize the experience and provide practical coping strategies. |
Expected Outcomes:
- Patient will report decreased anxiety related to tube feeding
- Patient will demonstrate effective coping mechanisms
- Patient will participate in care decisions regarding feeding regimen
- Patient will show reduced physiological signs of anxiety during feeding procedure
7. Risk for Fluid Volume Imbalance
Definition/Related Factors:
Vulnerable to a decrease, increase, or rapid shift from one to the other of intravascular, interstitial, and/or intracellular fluid, related to formula concentration, inadequate free water intake, or excessive gastric losses.
Assessment Data:
- Monitor intake and output
- Assess skin turgor, mucous membranes, and thirst
- Evaluate laboratory values (BUN, creatinine, electrolytes)
- Monitor weight changes
- Assess for edema or signs of dehydration
- Monitor vital signs
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Administer free water flushes as prescribed (typically 30-60 mL before and after feedings or medications). | Provides additional hydration beyond what is contained in formula and prevents tube clogging. |
| Accurately document all fluid intake (formula, water, medications) and output (urine, stool, gastric drainage, wound drainage). | Allows for close monitoring of fluid balance and early identification of imbalances. |
| Monitor for signs of dehydration (dry mucous membranes, poor skin turgor, concentrated urine) or fluid overload (edema, dyspnea, crackles in lungs). | Early detection of fluid imbalance permits prompt intervention. |
| Weigh patient daily at same time and under same conditions. | Significant weight changes over short periods may indicate fluid shifts. |
| Monitor laboratory values and report significant changes. | Abnormal electrolytes or increased BUN/creatinine ratio may indicate dehydration. |
| Adjust water flushes based on patient needs and clinical status as ordered. | Individualized fluid administration helps maintain proper hydration status. |
Expected Outcomes:
- Patient will maintain adequate hydration as evidenced by moist mucous membranes, good skin turgor, and appropriate urine output
- Patient will maintain stable weight without significant day-to-day fluctuations
- Patient will exhibit laboratory values within normal ranges
- Patient will not show signs of dehydration or fluid overload
8. Impaired Comfort
Definition/Related Factors:
Perceived lack of ease, relief, and transcendence in physical, psychospiritual, environmental, and social dimensions, related to tube placement, abdominal distention, or gastrointestinal symptoms from feeding.
Assessment Data:
- Assess patient’s self-report of discomfort
- Observe for nonverbal signs of discomfort (grimacing, restlessness)
- Evaluate abdominal distention, cramping, or bloating
- Assess for tube displacement or irritation at insertion site
- Monitor for symptoms such as nausea, diarrhea, or constipation
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Secure feeding tube properly to prevent pulling or tension on the tube. | Reduces discomfort from tube movement or pressure at insertion site. |
| Administer feedings at room temperature. | Cold feedings can cause cramping and discomfort. |
| Start feedings slowly and increase rate gradually as tolerated. | Allows gastrointestinal tract to adapt to formula and reduces risk of cramping or diarrhea. |
| Administer medications for discomfort as prescribed (antacids, anti-gas medications, etc.). | Provides relief from specific gastrointestinal symptoms. |
| Position patient for comfort during and after feedings. | Proper positioning can reduce reflux and minimize abdominal discomfort. |
| Consider changing formula or administration rate if persistent discomfort occurs (in consultation with healthcare provider). | Different formulations or feeding schedules may be better tolerated. |
Expected Outcomes:
- Patient will report decreased discomfort related to tube feeding
- Patient will show fewer nonverbal signs of distress during feedings
- Patient will maintain normal bowel function without excessive gas, bloating, or diarrhea
- Patient will demonstrate increased tolerance to feeding regimen over time
9. Risk for Tube Displacement
Definition/Related Factors:
Vulnerable to inadvertent movement or removal of feeding tube from intended position, related to inadequate tube securement, confusion, agitation, or self-removal by patient.
Assessment Data:
- Verify tube placement and position marking
- Assess securement method and integrity
- Evaluate patient’s cognitive status and potential for tube manipulation
- Monitor for unexplained changes in tolerance to feeding
- Check for signs of displaced tube (coughing, gagging, respiratory distress)
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Mark tube at exit site with permanent marker or tape and document measurement. | Provides visual reference point to detect if tube has migrated in or out. |
| Secure tube with appropriate device or hypoallergenic tape using proper technique. | Prevents accidental dislodgment while maintaining skin integrity. |
| Verify tube placement before each feeding or medication administration according to facility protocol. | Ensures tube is in correct position before delivering formula or medications. |
| For confused or agitated patients, consider using mitts or alternate securing methods as the least restrictive option. | Prevents self-removal while maintaining patient dignity and safety. |
| Educate patient and caregivers about the importance of tube position and how to recognize displacement. | Promotes early identification of tube dislocation and prevents complications. |
| If displacement is suspected, hold feeding, verify placement per protocol, and notify provider if repositioning is needed. | Prevents complications from feeding through a displaced tube. |
Expected Outcomes:
- Feeding tube will remain in proper position between tube placement checks
- Tube marking will remain at documented position
- Patient will not experience complications related to tube displacement
- Patient/caregiver will demonstrate understanding of proper tube securement
10. Disturbed Body Image
Definition/Related Factors:
Confusion in mental picture of one’s physical self, related to presence of visible feeding tube, dependency on artificial means of nutrition, or alterations in body function.
Assessment Data:
- Assess patient’s verbal and nonverbal responses to tube placement
- Evaluate avoidance of looking at or touching the tube
- Note expressions of negative feelings about appearance or body function
- Assess for social withdrawal or avoidance of social situations
- Evaluate coping mechanisms and support systems
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Acknowledge the patient’s feelings about the feeding tube and changes in body function. | Validates emotions and shows respect for the patient’s experience. |
| Involve patient in care of the feeding tube when appropriate. | Increases sense of control and promotes adaptation to body changes. |
| Suggest strategies to minimize visibility of tube (scarves, high-necked clothing for nasogastric tubes; clothing options for gastrostomy tubes). | Provides practical solutions for social situations and improves confidence. |
| Refer to support groups or connect with others who have similar feeding tubes. | Peer support normalizes the experience and provides psychological benefits. |
| Focus on the patient’s strengths and abilities rather than limitations. | Promotes positive self-concept despite physical changes. |
| Encourage expression of feelings through conversation, journaling, or creative activities. | Provides outlet for emotions and assists in psychological adaptation. |
Expected Outcomes:
- Patient will verbalize improved acceptance of feeding tube
- Patient will participate in self-care activities related to tube feeding
- Patient will maintain social interactions and relationships
- Patient will demonstrate healthy coping strategies for body image changes
11. Risk for Electrolyte Imbalance
Definition/Related Factors:
Vulnerable to changes in serum electrolyte levels that may compromise health, related to diarrhea, vomiting, improper formula selection, refeeding syndrome, or medication interactions.
Assessment Data:
- Monitor laboratory values (sodium, potassium, magnesium, phosphorus, calcium)
- Assess for clinical manifestations of electrolyte imbalances
- Evaluate gastrointestinal losses (diarrhea, vomiting)
- Review medication profile for potential interactions with electrolytes
- Assess nutritional status prior to initiation of feeding (risk for refeeding syndrome)
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Monitor serum electrolytes as ordered and report significant changes. | Early detection allows timely intervention to prevent complications. |
| For malnourished patients, start feedings at lower rates and advance slowly. | Prevents refeeding syndrome, which can cause severe electrolyte shifts, particularly of phosphorus, potassium, and magnesium. |
| Administer electrolyte supplements as prescribed. | Corrects identified deficiencies to maintain physiologic balance. |
| Monitor for and manage diarrhea promptly. | Excessive diarrhea can lead to significant electrolyte losses, particularly potassium. |
| Consult with dietitian to select appropriate formula based on electrolyte needs. | Formula composition can be adjusted to address specific electrolyte requirements. |
| Monitor cardiac rhythm in patients at high risk for severe electrolyte disturbances. | Electrolyte imbalances, particularly potassium, can cause cardiac arrhythmias. |
Expected Outcomes:
- Patient will maintain electrolyte values within normal ranges
- Patient will not exhibit clinical signs of electrolyte imbalance
- Patient will tolerate feeding advancement without refeeding syndrome
- Patient will receive appropriate formula to meet electrolyte needs
12. Social Isolation
Definition/Related Factors:
Aloneness experienced by the individual and perceived as imposed by others and as a negative or threatening state, related to inability to participate in normal eating activities, embarrassment about feeding tube, or perceived stigma.
Assessment Data:
- Assess patient’s social interactions and support network
- Evaluate expressions of loneliness or isolation
- Note avoidance of social situations, particularly those involving food
- Assess impact of tube feeding on daily routines and social activities
- Evaluate coping mechanisms and adjustment to lifestyle changes
Nursing Interventions with Rationales:
| Interventions | Rationales |
|---|---|
| Encourage patient to participate in social activities, adjusting feeding schedule if possible to accommodate important events. | Promotes continued social engagement while managing nutritional needs. |
| Suggest discreet methods for managing tube feeding in social settings (using a backpack for portable feeding pump, timing feedings before social events). | Provides practical strategies for maintaining social connections while managing feeding requirements. |
| Refer to support groups for individuals with feeding tubes. | Connects patient with others who understand the challenges and can share coping strategies. |
| Educate family and friends about tube feeding to increase understanding and support. | Reduces misconceptions and discomfort, encouraging continued social relationships. |
| Explore alternative ways for the patient to participate in food-related social activities. | Maintains connection to important cultural and social traditions despite feeding restrictions. |
| Consider referral to mental health professional if significant social withdrawal or depression develops. | Provides additional support for psychological adjustment to life changes. |
Expected Outcomes:
- Patient will maintain meaningful social connections and relationships
- Patient will participate in desired social activities
- Patient will express decreased feelings of isolation or loneliness
- Patient will demonstrate effective strategies for managing tube feeding in social contexts
Home Care Advice for Gastric Gavage
Transitioning from hospital to home with a gastric gavage feeding tube requires thorough preparation and education. The following home care advice is essential for patients and caregivers to safely manage enteral feeding at home.
Tube Care and Maintenance
- Clean the insertion site daily with mild soap and water, then pat dry
- Inspect the site for signs of infection (redness, swelling, drainage, pain)
- Secure the tube properly to prevent pulling or dislodgement
- For nasogastric tubes, clean nostrils daily and apply water-soluble lubricant if needed
- Check tube position marking daily to ensure the tube hasn’t migrated
- Flush tube with 30-60 mL water before and after feedings and medications
- Replace feeding equipment according to manufacturer recommendations
Formula Management
- Store unopened formula in a cool, dry place
- Check expiration dates before using formula
- Refrigerate opened formula and use within 24 hours
- Discard formula that has been at room temperature for more than 4 hours
- Warm formula to room temperature before administration
- Follow specific mixing instructions for powdered formulas
- Label prepared formula with date and time of preparation
- Keep a supply of formula on hand for emergencies
Recognizing Complications
- Contact healthcare provider immediately if:
- Tube becomes dislodged or falls out
- Fever develops, especially with redness or drainage at tube site
- Persistent vomiting, diarrhea, or abdominal distention occurs
- Difficulty breathing, coughing, or choking during feeding
- Formula leaks around the tube insertion site
- Unable to flush the tube due to clogging
- Signs of dehydration (dry mouth, decreased urine output, dizziness)
- Significant weight changes (gain or loss)
Daily Management Tips
- Keep a daily log of feedings, water flushes, and medications
- Weigh weekly (or as directed) at the same time of day
- Elevate the head of the bed or sit upright during and after feedings
- Follow prescribed feeding schedule and rates
- Administer medications properly, checking for interactions with formula
- Practice good oral hygiene even if not eating by mouth
- Maintain activity as tolerated and recommended
- Keep emergency contact information readily available
- Have a backup plan for power outages if using an electric feeding pump
Follow-up Care:
- Attend all scheduled follow-up appointments with healthcare providers
- Have laboratory tests done as ordered to monitor nutritional status
- Contact healthcare team with any questions or concerns about the feeding regimen
- Request regular reassessment of nutritional needs as condition changes
- Keep track of supply needs and order replacements before running out
References
- American Society for Parenteral and Enteral Nutrition (ASPEN). (2022). Enteral Nutrition Practice Recommendations.
- Bankhead, R., Boullata, J., Brantley, S., Corkins, M., Guenter, P., Krenitsky, J., Lyman, B., Metheny, N. A., Mueller, C., Robbins, S., & Wessel, J. (2009). Enteral nutrition practice recommendations. Journal of Parenteral and Enteral Nutrition, 33(2), 122-167.
- Boullata, J. I., Carrera, A. L., Harvey, L., Escuro, A. A., Hudson, L., Mays, A., McGinnis, C., Wessel, J. J., Bajpai, S., Beebe, M. L., Kinn, T. J., Klang, M. G., Lord, L., Martin, K., Pompeii‐Wolfe, C., Sullivan, J., Wood, A., Malone, A., & Guenter, P. (2017). ASPEN safe practices for enteral nutrition therapy. Journal of Parenteral and Enteral Nutrition, 41(1), 15-103.
- Herdman, T.H., & Kamitsuru, S. (Eds.). (2018). NANDA International nursing diagnoses: Definitions and classification, 2018-2020. Thieme.
- Metheny, N. A., & Meert, K. L. (2014). Monitoring feeding tube placement. Nutrition in Clinical Practice, 29(6), 737-748.
- Perry, A. G., Potter, P. A., & Ostendorf, W. R. (2018). Clinical nursing skills and techniques. Elsevier.
- RNpedia. (2023). Gastric Gavage Feeding. Retrieved from https://www.rnpedia.com/nursing-notes/fundamentals-in-nursing-notes/gastric-gavage-feeding/
- Taylor, C., Lillis, C., Lynn, P., & LeMone, P. (2019). Fundamentals of nursing: The art and science of person-centered care. Wolters Kluwer.
