Postpartum Care: Nursing Management from 72 Hours to 6 Weeks
Comprehensive nursing notes on maternal care during the postpartum recovery period
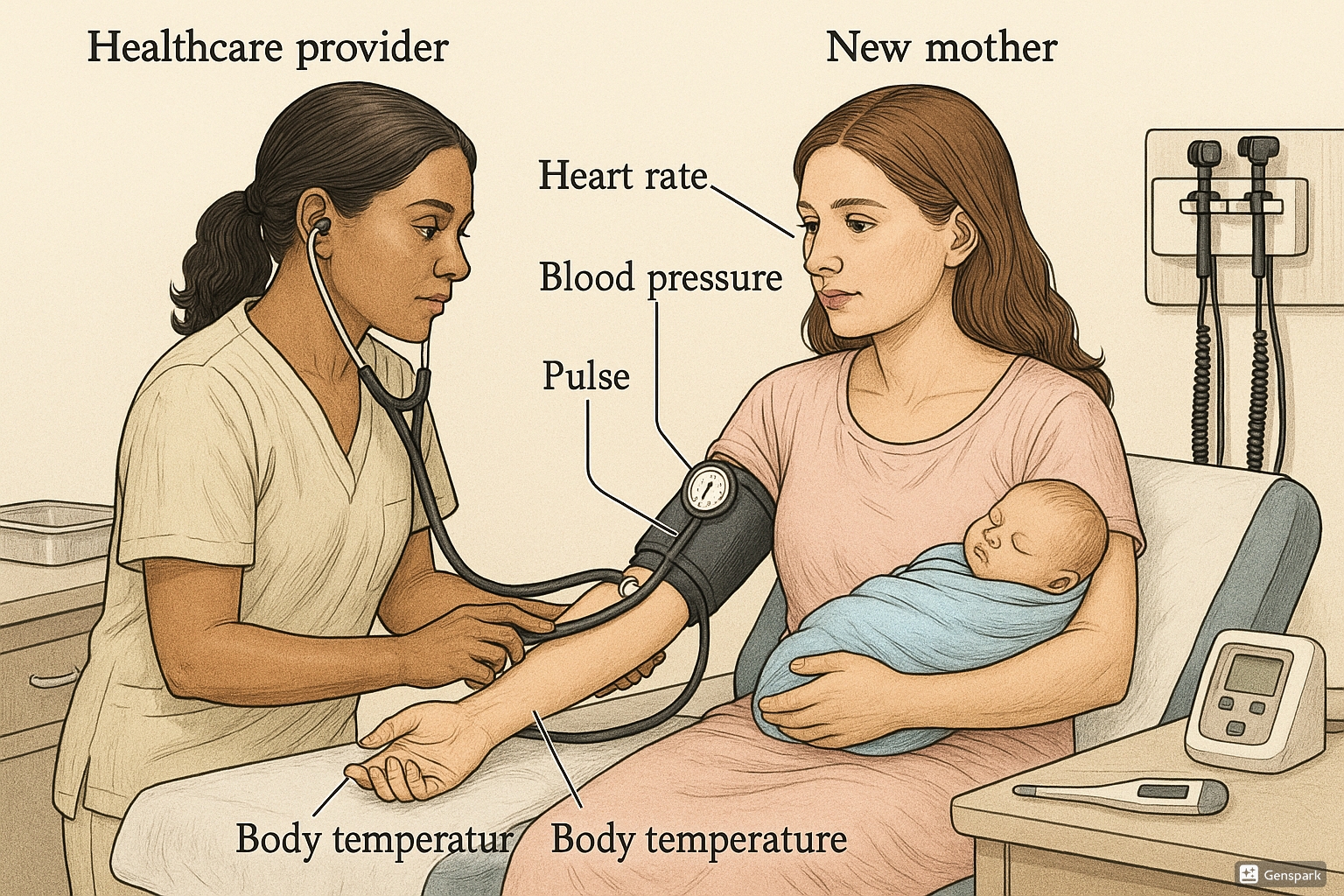
Figure 1: Healthcare provider conducting a comprehensive postpartum recovery assessment
1. Introduction to Postpartum Recovery
The postpartum period, also known as the puerperium, extends from the delivery of the placenta and membranes until six weeks after birth. While the first 72 hours (immediate postpartum period) are critical for stabilization, the extended postpartum recovery period (from 72 hours to 6 weeks) involves significant physiological and psychological adjustments as the mother’s body returns to its non-pregnant state.
During this extended postpartum recovery phase, nursing care focuses on monitoring the normal involution process, detecting complications early, supporting breastfeeding, providing education on self-care, and promoting maternal-infant bonding. This period is divided into the subacute postpartum period (4-28 days after birth) and the delayed postpartum period (29-42 days after birth).
2. Physiological Changes
2.1 Uterine Involution
Uterine involution is the process where the uterus returns to its pre-pregnancy state. During postpartum recovery, the uterus undergoes rapid reduction in size through autolysis (self-digestion) of excess tissue and contraction of muscle fibers.
| Timeframe | Expected Fundal Height | Nursing Assessment |
|---|---|---|
| Day 3-4 | 2-3 cm below umbilicus | Firm, midline fundus |
| Day 5-7 | 4-5 cm below umbilicus | Check for firmness and position |
| Day 7-10 | Not palpable abdominally | Descent into pelvis |
| 2 weeks | In pelvis, not palpable | Assess via bimanual exam if indicated |
| 6 weeks | Returns to normal size | Nearly complete involution |
During postpartum recovery, nurses should teach mothers to monitor their own uterine involution by checking fundal height and firmness. Delayed involution may indicate retained placental fragments or postpartum infection.
2.2 Lochia Progression
Lochia is the vaginal discharge consisting of blood, tissue, and mucus that occurs after delivery. The character and amount of lochia changes throughout the postpartum recovery period and serves as an important assessment parameter.
| Type | Timeframe | Characteristics | Clinical Significance |
|---|---|---|---|
| Lochia Rubra | Days 1-3 | Bright red, primarily blood | Normal immediately after delivery |
| Lochia Serosa | Days 4-10 | Pinkish-brown, serous and red blood cells | Transition stage of healing |
| Lochia Alba | Days 11-21 (up to 6 weeks) | Yellowish-white, leukocytes and decidua | Final stage of endometrial healing |
- Sudden increase in bright red bleeding after it had decreased
- Saturation of a pad within one hour
- Passing large clots (larger than a quarter)
- Foul-smelling lochia
- Persistent lochia rubra beyond 2 weeks
2.3 Changes in Reproductive Organs
During postpartum recovery, all reproductive organs undergo significant changes:
- Cervix: Initially soft and dilated, gradually closes to 1-2 cm by the end of the first week. By 6 weeks, it regains its firmness but often retains some permanent change in shape.
- Vagina: Initially swollen and edematous, gradually returns to pre-pregnancy state over 6-8 weeks. The rugae reappear by weeks 3-4.
- Perineum: If episiotomy or laceration occurred, healing progresses through the inflammatory, proliferative, and remodeling phases. Complete healing takes 4-6 weeks.
- Ovarian function: Return of ovulation is variable:
- Non-breastfeeding mothers: May ovulate as early as 4-6 weeks postpartum
- Breastfeeding mothers: Typically delayed ovulation due to elevated prolactin levels
2.4 Systemic Changes
Beyond reproductive organs, the entire body undergoes readjustment during postpartum recovery:
| System | Changes | Nursing Considerations |
|---|---|---|
| Cardiovascular |
|
|
| Urinary |
|
|
| Gastrointestinal |
|
|
| Musculoskeletal |
|
|
| Endocrine |
|
|
3. Postpartum Assessment
3.1 Home Visit Assessment
For many mothers, home visits are a critical component of postpartum recovery care between hospital discharge and the 6-week follow-up. These visits allow nurses to assess recovery in the home environment and provide targeted interventions.
A comprehensive postpartum recovery assessment should include:
- Vital signs: Temperature, pulse, respiration, blood pressure
- Physical assessment: Fundal height, lochia, perineum, breasts, incision sites
- Systems review: Cardiovascular, respiratory, gastrointestinal, urinary
- Emotional status: Mood, sleep patterns, anxiety, bonding with infant
- Knowledge assessment: Understanding of self-care, infant care, warning signs
- Support system: Partner involvement, family support, resources
3.2 BUBBLE-HE Assessment Framework
The BUBBLE-HE mnemonic is a practical framework for postpartum recovery assessment that covers all essential aspects of maternal care:
BUBBLE-HE Mnemonic for Postpartum Recovery Assessment:
- B – Breasts: Engorgement, mastitis, nipple condition, lactation status
- U – Uterus: Fundal height, firmness, midline position, tenderness
- B – Bladder: Urinary output, retention, incontinence, infection symptoms
- B – Bowels: Constipation, hemorrhoids, return of normal function
- L – Lochia: Color, amount, odor, presence of clots
- E – Episiotomy/laceration: Healing progress, signs of infection, pain level
- H – Homan’s sign: Check for deep vein thrombosis
- E – Emotional status: Mood, anxiety, bonding, social support
This systematic approach ensures comprehensive assessment during postpartum recovery home visits and follow-up appointments, enabling early detection of complications and appropriate intervention.
4. Postpartum Complications
While many women experience uncomplicated postpartum recovery, nurses must remain vigilant for potential complications that can occur between 72 hours and 6 weeks after delivery.
4.1 Late Postpartum Hemorrhage
Late or secondary postpartum hemorrhage occurs after the first 24 hours up to 12 weeks postpartum, with most cases occurring between 1-2 weeks during postpartum recovery.
| Causes | Assessment Findings | Nursing Interventions |
|---|---|---|
|
|
|
4.2 Postpartum Infection
Infections account for approximately 15% of maternal deaths worldwide. During postpartum recovery, infections may develop in various sites:
| Infection Type | Common Presentation | Nursing Interventions |
|---|---|---|
| Endometritis |
|
|
| Urinary Tract Infection |
|
|
| Mastitis |
|
|
| Wound Infection |
|
|
REEDA Scale for Wound Assessment During Postpartum Recovery:
- R – Redness
- E – Edema
- E – Ecchymosis (bruising)
- D – Drainage
- A – Approximation (closure of wound edges)
Each component is scored 0-3, with higher scores indicating potential infection or impaired healing.
4.3 Thromboembolic Disorders
Pregnant and postpartum women have a 4-5 times higher risk of thromboembolic events compared to non-pregnant women. This risk extends throughout the postpartum recovery period.
| Condition | Risk Factors | Assessment Findings | Nursing Interventions |
|---|---|---|---|
| Deep Vein Thrombosis (DVT) |
|
|
|
| Pulmonary Embolism (PE) |
|
|
|
4.4 Postpartum Mood Disorders
Psychological complications are common during postpartum recovery and range from mild “baby blues” to severe psychiatric emergencies.
| Condition | Onset & Duration | Clinical Features | Nursing Interventions |
|---|---|---|---|
| Postpartum Blues | Days 3-5, resolves within 2 weeks |
|
|
| Postpartum Depression | Within first 4 weeks to 1 year, most common at 6-12 weeks postpartum |
|
|
| Postpartum Psychosis | Usually within first 2 weeks, peak at 3-4 days |
|
|
SAFE MOM Screening for Postpartum Depression Risk Factors:
- S – Sleep disturbances
- A – Anxiety or panic attacks
- F – Family history of mood disorders
- E – Emotional liability and excessive worry
- M – Major life stressors
- O – Obsessive thoughts about infant
- M – Mother’s history of depression
5. Nursing Interventions
5.1 Supporting Physical Recovery
Nursing interventions during the extended postpartum recovery period focus on promoting healing, preventing complications, and educating the mother about self-care.
Perineal Care
- Teach proper perineal hygiene (front-to-back cleansing)
- Demonstrate sitz bath technique: 15-20 minutes, 2-3 times daily
- Instruct on proper pad changing and hand hygiene
- Teach proper application of topical medications if prescribed
- Advise on Kegel exercises to strengthen pelvic floor muscles
Cesarean Incision Care
- Assess incision for signs of infection or dehiscence
- Teach proper cleaning technique with mild soap and water
- Instruct to pat dry thoroughly after showering
- Advise on supporting abdomen when coughing or sneezing
- Demonstrate proper application of prescribed topical medications
Pain Management
- Assess pain using standardized scale
- Administer analgesics as prescribed, educate on timing and dosage
- Teach non-pharmacological methods:
- Ice packs for perineal discomfort (first 24-48 hours)
- Warm compresses after 48 hours
- Positioning for comfort
- Relaxation techniques
- Monitor effectiveness of pain management strategies
5.2 Emotional Support
The emotional challenges of postpartum recovery can be significant. Nurses play a crucial role in supporting the mother’s psychological adjustment.
Strategies for Emotional Support
- Regular screening for postpartum mood disorders
- Normalizing common emotional responses to motherhood
- Encouraging verbalization of feelings and concerns
- Facilitating communication between partners about role transitions
- Providing information about community support groups
- Teaching stress-reduction techniques:
- Deep breathing exercises
- Progressive muscle relaxation
- Mindfulness practice
- Promoting adequate sleep and rest periods
5.3 Breastfeeding Support
Extended breastfeeding support is vital during the postpartum recovery period as many women encounter challenges after leaving the hospital.
Common Breastfeeding Issues During Postpartum Recovery
| Issue | Nursing Interventions |
|---|---|
| Engorgement |
|
| Sore/Cracked Nipples |
|
| Plugged Ducts |
|
| Perception of Insufficient Milk |
|
Monitoring Adequate Intake
Teach mothers to monitor these signs of adequate intake during postpartum recovery:
- 6+ wet diapers per day after day 4
- 3-4 yellow, seedy stools per day (may decrease after 4-6 weeks)
- Audible swallowing during feeding
- Infant appears satisfied after feeding
- Return to birth weight by 10-14 days
5.4 Family Planning Counseling
Comprehensive postpartum recovery care includes discussion of contraception options before the woman resumes sexual activity.
Key Points for Contraceptive Counseling
- Ovulation can occur as early as 25 days postpartum in non-breastfeeding mothers
- Breastfeeding alone (LAM – Lactational Amenorrhea Method) is effective only when:
- Baby is less than 6 months old
- Mother is exclusively breastfeeding
- No menstruation has returned
- Progestin-only methods (mini-pill, implant, injection) are safe during breastfeeding
- Combined hormonal methods may affect milk supply and are typically started after 6 weeks in breastfeeding mothers
- IUDs can be inserted at the postpartum visit (some immediately after delivery)
- Barrier methods can be used when sexual activity resumes
- Immediate postpartum (within 10 minutes of placental delivery): Copper IUD
- Before hospital discharge: Progestin-only methods, hormonal IUD
- At 3-week visit: Barrier methods if sexual activity resumed
- At 6-week visit: Combined hormonal methods if not breastfeeding
6. Postpartum Nutrition
Proper nutrition during postpartum recovery supports healing, energy levels, and lactation if breastfeeding. Nurses should provide evidence-based nutritional counseling.
Nutritional Needs During Postpartum Recovery
| Nutrient | Importance | Food Sources | Special Considerations |
|---|---|---|---|
| Protein | Tissue repair, immune function | Lean meats, poultry, fish, eggs, legumes, dairy | Need increases by 25g daily if breastfeeding |
| Iron | Blood volume restoration, fatigue prevention | Red meat, spinach, beans, fortified cereals | Supplement often continued, especially after hemorrhage |
| Calcium | Bone health, breast milk production | Dairy products, fortified non-dairy milks, leafy greens | 500 mg transferred to breast milk daily |
| Vitamin D | Calcium absorption, immune function | Fatty fish, fortified milk, egg yolks, sunlight | Supplement recommended, especially in winter months |
| Vitamin C | Wound healing, immune support | Citrus fruits, berries, tomatoes, bell peppers | Enhances iron absorption when consumed together |
| B Vitamins | Energy metabolism, nervous system function | Whole grains, meat, eggs, legumes | B12 supplement for vegetarian/vegan mothers |
| Omega-3 Fatty Acids | Brain development for breastfed infant, reducing inflammation | Fatty fish, flaxseeds, walnuts | DHA supplements often recommended |
| Fluids | Hydration, milk production | Water, milk, non-caffeinated beverages | Minimum 2-3 liters daily, more if breastfeeding |
| Fiber | Preventing constipation | Fruits, vegetables, whole grains, legumes | Gradual increase with adequate fluids |
Nutritional Guidelines for Postpartum Recovery
- Consume 1800-2200 calories daily for non-breastfeeding mothers
- Increase to 2300-2700 calories for breastfeeding mothers
- Eat smaller, frequent meals if experiencing fatigue
- Limit caffeine intake to 300 mg or less daily if breastfeeding
- Minimize highly processed foods high in sodium and sugar
- Consider continuing prenatal vitamins throughout breastfeeding
7. Postpartum Exercise
Appropriate exercise during postpartum recovery offers physical and psychological benefits but should be resumed gradually with consideration for the type of delivery and individual recovery progress.
Benefits of Postpartum Exercise
- Strengthens abdominal and pelvic floor muscles
- Promotes cardiovascular fitness
- Improves mood and reduces risk of postpartum depression
- Helps with gradual weight loss
- Increases energy levels
- Promotes better sleep quality
Exercise Progression During Postpartum Recovery
| Timeframe | Vaginal Delivery | Cesarean Delivery |
|---|---|---|
| First Week |
|
|
| 2-4 Weeks |
|
|
| 4-6 Weeks |
|
|
| After 6-Week Check |
|
|
Diastasis Recti Assessment and Exercises
Many women experience separation of the abdominal muscles (diastasis recti) during pregnancy. Nurses should teach proper assessment and exercises:
- Lie on back with knees bent, feet flat
- Place fingers at umbilicus, perpendicular to midline
- Lift head slightly off floor while feeling for separation
- Measure width and depth of separation
- Separation of more than 2 finger-widths indicates diastasis recti
For women with diastasis recti, recommend:
- Avoid traditional sit-ups, crunches, planks
- Focus on transverse abdominal exercises
- Consider referral to physical therapist specializing in women’s health
- Practice diaphragmatic breathing with core engagement
8. Follow-up Care
Scheduled follow-up care is an essential component of comprehensive postpartum recovery management.
Standard Postpartum Follow-up Schedule
| Timepoint | Assessment Focus | Interventions |
|---|---|---|
| 1-3 Week Visit (if indicated) |
|
|
| 6-Week Comprehensive Visit |
|
|
| 12-Week Visit (if indicated) |
|
|
Preparing Mothers for the 6-Week Visit
Nurses should educate mothers about what to expect and how to prepare for the standard 6-week postpartum recovery visit:
- Keep track of any physical concerns or symptoms
- Note questions about physical recovery, emotional well-being, infant care
- Be prepared to discuss sexual activity and contraception
- Consider bringing partner to discuss family adjustment
- Prepare to discuss return to work plans if applicable
- Bring list of current medications
- Understand that pelvic examination will likely be performed
9. Cultural Considerations in Postpartum Recovery
Cultural beliefs and practices significantly influence postpartum recovery behaviors. Culturally competent nursing care acknowledges and respects these diverse traditions while ensuring safety.
Examples of Cultural Postpartum Recovery Practices
| Cultural Practice | Description | Nursing Considerations |
|---|---|---|
| “La Cuarentena” (Latin American) | 40-day period of rest with mother-infant seclusion, assistance from female relatives, dietary restrictions, and traditional remedies |
|
| “Zuo Yuezi” (Chinese) | Month-long confinement with dietary practices (hot foods), activity restrictions, avoiding cold water, specific bathing restrictions |
|
| “Sawa Mahina” (South Asian) | 40-day confinement, warm foods, massage with oils, ceremonial bathing, avoidance of household work |
|
| Native American Practices | Varies by tribe; may include specific foods, ceremonies, use of traditional medicine, belly binding |
|
Principles for Culturally Competent Postpartum Recovery Care
- Conduct cultural assessment to understand specific beliefs and practices
- Avoid assumptions based on apparent cultural background
- Integrate safe cultural practices into care plan
- Use professional interpreters when language barriers exist
- Provide education that acknowledges and respects cultural beliefs
- Identify practices that might compromise safety and negotiate modifications
- Support beneficial cultural practices that promote rest and family bonding
10. Conclusion
The extended postpartum recovery period from 72 hours to 6 weeks represents a critical time of physiological and psychological adjustment. Comprehensive nursing care during this period focuses on monitoring physical recovery, detecting complications early, supporting breastfeeding, promoting emotional well-being, and providing education for self-care and newborn care.
Key nursing responsibilities during this time include:
- Systematic assessment using frameworks like BUBBLE-HE
- Early identification of common complications
- Culturally sensitive support of the transition to parenthood
- Practical education on self-care and infant care
- Coordination of appropriate referrals as needed
- Documentation of findings and interventions
Through comprehensive, evidence-based care during the extended postpartum recovery period, nurses can significantly contribute to maternal well-being, facilitate family adjustment, and promote positive long-term outcomes for mothers and infants.
