Nursing Performance Audit and Patient Satisfaction
Comprehensive guide to understanding, implementing, and optimizing nursing audit processes to enhance patient satisfaction and care quality
Table of Contents
1. Introduction to Nursing Performance Audit and Patient Satisfaction
In the evolving landscape of healthcare, nursing performance audits and patient satisfaction metrics have become critical components of quality assurance and improvement. Healthcare facilities worldwide are increasingly recognizing that systematic evaluation of nursing care, combined with patient feedback, drives meaningful improvements in care delivery and outcomes.
Why This Matters:
Nursing performance audits provide objective evidence of care quality, while patient satisfaction measures offer subjective experiences of care received. Together, they create a comprehensive picture of nursing effectiveness that drives continuous quality improvement.
This comprehensive guide explores the theoretical foundations, methodologies, and practical applications of nursing performance audits, their relationship to patient satisfaction, and implementation strategies for healthcare facilities seeking to enhance care quality through systematic evaluation processes.
2. Definitions & Key Concepts
Nursing Performance Audit
A nursing performance audit is a systematic, detailed review and evaluation of selected clinical records by qualified professional personnel for evaluating the quality of nursing care. It involves collecting information from nursing reports and other documented evidence about patient care and assessing the quality against established criteria and standards.
Patient Satisfaction
Patient satisfaction refers to patients’ perception and evaluation of their healthcare experience, including the care provided by nursing staff. It measures how well the delivered care meets or exceeds patients’ expectations and is considered a key indicator of healthcare quality.
Quality Assurance
Quality assurance in nursing encompasses planned and systematic activities that provide confidence that healthcare services will consistently meet predetermined standards of quality.
Evidence-Based Practice
The integration of clinical expertise, patient values, and the best research evidence into the decision-making process for patient care.
Mnemonic: A-U-D-I-T
- Assessment of current practice
- Understanding standards & criteria
- Data collection & analysis
- Implementing improvements
- Tracking outcomes & sustaining change
3. Nursing Audit Framework
A nursing audit framework provides a structured approach to evaluate nursing practice against predetermined standards. Several types of nursing audits exist, each with specific purposes and methodologies.

Figure 1: The Clinical Audit Cycle showing the continuous improvement process
Types of Nursing Audits
| Audit Type | Description | Primary Focus |
|---|---|---|
| Structure Audit | Evaluates the settings in which patient care occurs, including physical facilities, organizational structure, and resources | Environment, staffing, policies, equipment |
| Process Audit | Assesses how care is delivered by evaluating the actions and behaviors of nursing staff | Care delivery methods, procedures, protocols adherence |
| Outcome Audit | Measures the end results or changes in patient health status resulting from nursing care | Patient outcomes, recovery rates, complication rates |
| Concurrent Audit | Performed during ongoing nursing care to identify and address issues in real-time | Real-time quality improvement |
| Retrospective Audit | Conducted after patient discharge by reviewing patient records | Historical evaluation of care quality |
Components of a Nursing Audit Framework
- Standards Development: Creation of specific, measurable criteria based on evidence-based practice guidelines
- Audit Tool Design: Development of instruments to gather relevant data systematically
- Sampling Strategy: Determination of which records or practices to evaluate
- Data Collection: Systematic gathering of information using the audit tools
- Analysis: Comparison of collected data against established standards
- Reporting: Documentation and communication of findings
- Action Planning: Development of strategies to address identified gaps
- Implementation: Execution of improvement plans
- Re-audit: Follow-up evaluation to assess improvement
Clinical Insight:
Effective audit frameworks should be designed with input from front-line nursing staff to ensure relevance and buy-in. Frameworks that emerge from collaborative processes tend to yield more meaningful improvements in practice.
4. Audit Methodology
The methodology of nursing performance audits follows a systematic approach to ensure reliability, validity, and actionable results. Understanding these methodologies is essential for designing and implementing effective audit processes.
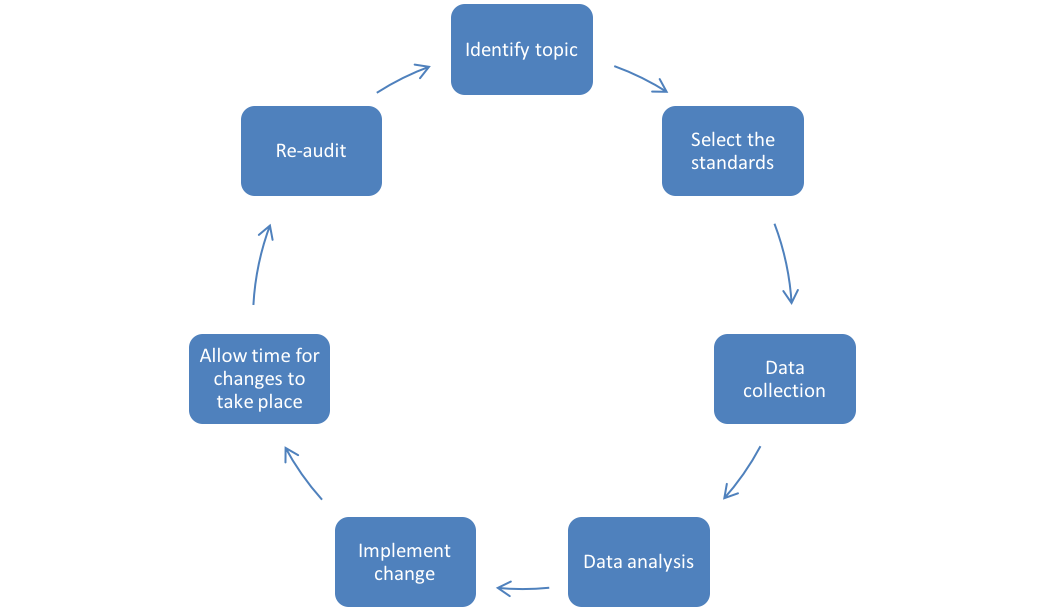
Figure 2: Detailed Clinical Audit Cycle showing key methodology components
The Six Stages of Nursing Audit Process
1 Preparing for the Audit
- Establish audit committee or team
- Define audit scope and objectives
- Conduct literature review for best practices
- Develop project plan with timelines
- Identify resources needed
- Communicate with stakeholders
2 Selecting Audit Criteria
- Identify evidence-based standards of care
- Develop specific, measurable criteria
- Ensure criteria reflect current best practice
- Consider patient-centered outcomes
- Validate criteria with subject matter experts
3 Measuring Performance
- Develop data collection tools
- Determine sampling methodology
- Train auditors for consistency
- Collect data through document review, observation, or interviews
- Ensure inter-rater reliability
4 Making Improvements
- Analyze data to identify gaps
- Prioritize areas for improvement
- Develop action plans with specific interventions
- Assign responsibilities for implementation
- Set timelines for completion
5 Sustaining Improvements
- Implement action plans
- Monitor progress regularly
- Provide support and resources
- Address barriers to implementation
- Celebrate successes
6 Re-auditing
- Schedule follow-up audit
- Use same criteria for comparison
- Analyze improvements and ongoing gaps
- Refine action plans as needed
- Establish continuous audit cycle
Mnemonic: P-E-R-F-O-R-M
- Prepare thoroughly
- Establish clear criteria
- Reliably collect data
- Formulate action plans
- Optimize implementation
- Review outcomes
- Monitor continuously
5. Patient Satisfaction: Measurement & Significance
Patient satisfaction is a multidimensional concept that encompasses various aspects of the healthcare experience. As a key quality indicator, it provides valuable insights into how patients perceive the care they receive.
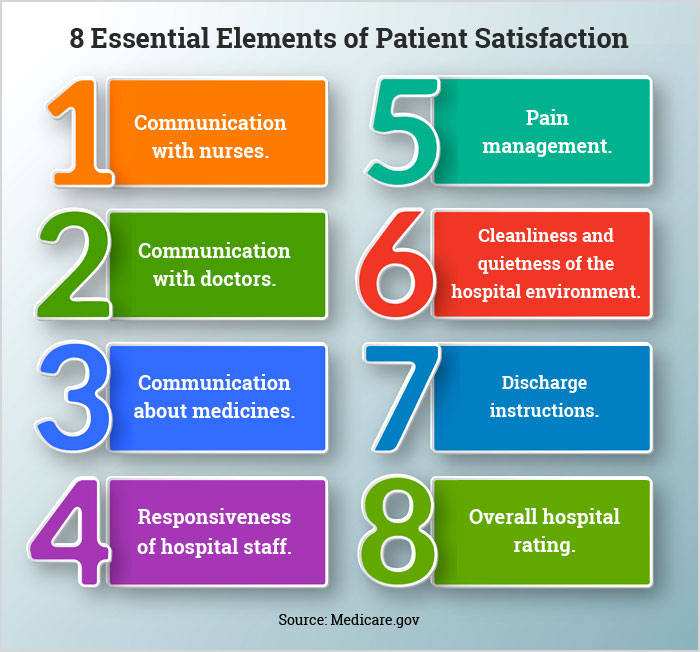
Figure 3: Components of Patient Satisfaction in Healthcare Settings
Dimensions of Patient Satisfaction
| Dimension | Description | Nursing Impact |
|---|---|---|
| Technical Competence | Perceived skill and professionalism in delivering care | Clinical skills, knowledge demonstration, confidence |
| Interpersonal Care | Quality of personal interactions with staff | Communication, empathy, respect, attentiveness |
| Accessibility | Ease of obtaining care when needed | Responsiveness to call bells, timeliness of care |
| Information & Education | Quality of communication about care, treatments, and health | Patient education, explanation of procedures |
| Physical Environment | Cleanliness, comfort, noise level, aesthetics | Unit cleanliness, noise management, comfort measures |
| Emotional Support | Addressing psychological aspects of illness | Compassion, reassurance, emotional presence |
| Involvement in Care | Inclusion in decision-making | Patient-centered care, shared decision-making |
| Continuity & Coordination | Seamless transition between care providers | Handoff communication, interdisciplinary collaboration |
Patient Satisfaction Assessment Tools
HCAHPS Survey
The Hospital Consumer Assessment of Healthcare Providers and Systems survey measures patients’ perspectives on hospital care. Used for national comparisons and linked to reimbursement.
Press Ganey
Comprehensive survey tool used by many hospitals to measure patient experience across multiple dimensions. Provides benchmarking capabilities.
PSNCQQ
Patient Satisfaction with Nursing Care Quality Questionnaire – 19-item tool specifically focused on nursing care quality.
NPS (Net Promoter Score)
Simple metric measuring likelihood to recommend, increasingly used in healthcare settings to gauge loyalty and satisfaction.
Clinical Insight:
While patient satisfaction metrics are valuable indicators of care quality, they should be interpreted alongside clinical outcome measures. Some evidence suggests that highly satisfied patients don’t always experience the best clinical outcomes.
6. Relationship Between Nursing Performance Audits and Patient Satisfaction
Nursing performance audits and patient satisfaction are intricately connected, with each influencing and informing the other. Understanding this relationship is crucial for developing comprehensive quality improvement strategies.

Figure 4: Factors influencing patient satisfaction, many of which are assessed in nursing audits
How Audit Findings Impact Patient Satisfaction
| Audit Area | Potential Impact on Patient Satisfaction |
|---|---|
| Documentation Quality | Better documentation leads to improved continuity of care, reducing errors and enhancing patient trust and satisfaction |
| Medication Administration | Proper medication protocols reduce adverse events, improve pain management, and increase patient comfort and satisfaction |
| Care Plan Implementation | Adherence to care plans ensures comprehensive, individualized care that meets patient needs and expectations |
| Communication Protocols | Standardized communication improves information sharing with patients, addressing a primary driver of satisfaction |
| Pain Assessment & Management | Regular, appropriate pain assessment leads to better pain control, significantly impacting satisfaction |
| Discharge Planning | Comprehensive discharge planning reduces readmissions and improves patients’ perception of care continuity |
Key Research Finding:
Research shows a positive correlation between nursing care quality (as measured by audits) and patient satisfaction. A study of over 29,000 patients across 107 hospitals found that the nurse-patient relationship was a significant predictor of overall nursing care satisfaction, with factors like trust, professional ethics, and caring being the strongest predictors.
Using Patient Satisfaction Data to Inform Audits
- Identifying Audit Priorities: Areas with low satisfaction scores can be targeted for focused audits
- Developing Audit Criteria: Patient feedback can inform the standards and criteria used in audits
- Validating Audit Findings: Satisfaction data can confirm whether audit-identified improvements translate to better patient experiences
- Measuring Impact: Pre and post-implementation satisfaction scores can measure the effectiveness of audit-driven improvements
- Closing the Feedback Loop: Sharing with patients how their feedback influenced care practices enhances engagement
Mnemonic: S-A-T-I-S-F-Y
- Systematically audit care processes
- Analyze findings alongside satisfaction data
- Target improvement opportunities
- Implement evidence-based changes
- Survey patients post-implementation
- Feedback results to staff
- Yield continuous improvement
7. Implementation Strategies for Effective Nursing Audits
Implementing an effective nursing audit system requires careful planning, stakeholder engagement, and strategic execution. The following strategies can help healthcare organizations establish successful audit programs that drive meaningful improvements in care quality.

Figure 5: Schematic diagram of an audit implementation cycle
Organizational Readiness Assessment
Before implementing a nursing audit program, assess your organization’s readiness by evaluating:
- Current quality improvement infrastructure
- Staff attitudes toward audit and feedback
- Available resources (time, personnel, technology)
- Leadership support and commitment
- Existing data collection systems
- Potential barriers to implementation
Key Implementation Steps
1 Secure Leadership Support
- Engage nursing leadership early in the process
- Present business case highlighting benefits
- Connect audit goals to organizational priorities
- Secure necessary resources and protected time
2 Establish Audit Infrastructure
- Form a multidisciplinary audit committee
- Define roles and responsibilities
- Develop policies and procedures
- Create communication channels
- Select appropriate audit tools
3 Build Staff Capacity
- Provide education on audit purpose and process
- Train audit team members
- Develop champions on each unit
- Address concerns and resistance
- Create a supportive, non-punitive environment
4 Pilot and Refine
- Start with a small-scale pilot
- Test audit tools and processes
- Gather feedback from participants
- Refine methodology based on pilot findings
- Document lessons learned
5 Scale Implementation
- Develop roll-out plan for organization-wide implementation
- Provide ongoing education and support
- Monitor implementation progress
- Address emerging barriers
- Celebrate early successes
6 Sustain and Integrate
- Incorporate audit into routine operations
- Link with existing quality improvement initiatives
- Regularly evaluate audit system effectiveness
- Refine as needed based on outcomes
- Develop succession planning for audit leadership
Implementation Insight:
Research shows that successful audit implementations are characterized by strong leadership support, adequate resources, meaningful staff engagement, and integration with existing quality improvement systems. Organizations that approach audits as learning opportunities rather than punitive measures achieve greater long-term success.
8. Best Practices in Nursing Performance Audits
Drawing from evidence and experience, the following best practices can enhance the effectiveness of nursing performance audits and maximize their impact on patient care and satisfaction.
Audit Design Best Practices
Focus on High-Impact Areas
Target aspects of care that have the greatest influence on patient outcomes and satisfaction (e.g., medication safety, pain management, care transitions).
Use Valid, Reliable Measures
Develop audit criteria based on evidence-based practice guidelines and test tools for reliability before full implementation.
Balance Quantity and Quality
Include both quantitative measures (e.g., completion rates) and qualitative assessments (e.g., appropriateness of interventions).
Incorporate Patient Perspective
Include patient-reported outcomes and experiences as part of the audit criteria when possible.
Audit Implementation Best Practices
Train Auditors Thoroughly
Ensure all auditors receive comprehensive training on audit tools, methodology, and inter-rater reliability.
Use Electronic Solutions
When possible, utilize electronic audit tools to streamline data collection, analysis, and reporting.
Balance Frequency and Depth
Conduct frequent, focused mini-audits for ongoing monitoring and comprehensive audits less frequently.
Sample Appropriately
Use statistically valid sampling methods to ensure results are representative of overall practice.
Feedback and Improvement Best Practices
Provide Timely Feedback
Share audit results promptly with staff to maintain engagement and facilitate rapid improvement.
Make Feedback Actionable
Present findings with specific, actionable recommendations for improvement.
Celebrate Success
Recognize and celebrate improvements and achievements to motivate continued engagement.
Close the Feedback Loop
Communicate how audit findings led to specific changes and improvements in care delivery.
Mnemonic: B-E-S-T
- Base audits on evidence and standards
- Engage staff at all levels of the process
- Share results transparently and promptly
- Track improvements and celebrate progress
9. HCAHPS Survey: A Critical Tool for Patient Satisfaction Assessment
The Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey is a standardized, publicly reported survey of patients’ perspectives on hospital care. As a key measure of patient satisfaction, it has significant implications for nursing performance audits and quality improvement.

Figure 6: Overview of HCAHPS survey structure and domains
HCAHPS Survey Structure
The HCAHPS survey consists of 29 questions organized into key domains:
| Domain | Sample Questions | Nursing Relevance |
|---|---|---|
| Nurse Communication | “During this hospital stay, how often did nurses treat you with courtesy and respect?” “How often did nurses listen carefully to you?” | Directly measures nursing interpersonal skills and communication effectiveness |
| Doctor Communication | “During this hospital stay, how often did doctors explain things in a way you could understand?” | Reflects interdisciplinary collaboration and care coordination |
| Hospital Environment | “During this hospital stay, how often was your room and bathroom kept clean?” “How often was the area around your room quiet at night?” | Nurses influence environment through unit management and noise control |
| Responsiveness | “How often did you get help in getting to the bathroom or in using a bedpan as soon as you wanted?” | Directly measures timely nursing response to basic needs |
| Pain Management | “How often was your pain well controlled?” “How often did hospital staff do everything they could to help with your pain?” | Reflects nursing assessment and intervention for pain |
| Communication about Medicines | “Before giving you any new medicine, how often did hospital staff tell you what the medicine was for?” | Measures nursing patient education regarding medications |
| Discharge Information | “During this hospital stay, did you get information in writing about symptoms or health problems to look out for after leaving the hospital?” | Evaluates nursing discharge education effectiveness |
| Overall Rating and Recommendation | “Using any number from 0 to 10, where 0 is the worst hospital possible and 10 is the best hospital possible, what number would you use to rate this hospital during your stay?” | Nursing care is a major contributor to overall satisfaction |
Key Insight:
Multiple studies show that nursing care domains (especially nurse communication and responsiveness) are among the strongest predictors of patients’ overall satisfaction and likelihood to recommend the hospital.
Integrating HCAHPS with Nursing Audits
- Align Audit Criteria: Design audit tools that evaluate the same care processes measured by HCAHPS
- Correlate Results: Analyze relationships between audit findings and HCAHPS scores
- Targeted Improvements: Focus improvement efforts on areas with both low audit compliance and low HCAHPS scores
- Measure Impact: Use HCAHPS as one indicator of the effectiveness of audit-driven improvements
- Staff Education: Help nurses understand the connection between their documented practice and patient perceptions
Implementation Note:
Many successful hospitals create crosswalks between their nursing audit criteria and HCAHPS domains, allowing them to predict the potential impact of practice changes on survey results. This approach enables more strategic quality improvement efforts.
10. Challenges in Nursing Audits & Patient Satisfaction Assessment
While nursing performance audits and patient satisfaction assessment are valuable quality improvement tools, they present several challenges that must be addressed for successful implementation and meaningful outcomes.
Common Challenges and Solutions
| Challenge | Impact | Solutions |
|---|---|---|
| Time Constraints | Staff lack time to conduct thorough audits amid clinical responsibilities |
|
| Staff Resistance | Nursing staff may view audits as punitive or bureaucratic |
|
| Complex EHR Systems | Electronic documentation can be fragmented across multiple screens/modules |
|
| Inconsistent Methods | Variations in audit approach reduce reliability and comparability |
|
| Low Survey Response Rates | Limited patient participation skews satisfaction data |
|
| Data Overload | Excessive data without analysis leads to inaction |
|
| Limited Follow-through | Implementation of improvements identified from audit findings often falls short |
|
Ethical Considerations
Confidentiality & Privacy
Ensure patient and staff confidentiality during audit processes and when sharing results. De-identify data whenever possible and follow institutional privacy policies.
Fairness & Bias
Develop audit processes that minimize bias and ensure fair evaluation of all staff and units. Consider factors that may affect performance (acuity, staffing) when interpreting results.
Transparency
Maintain transparency about audit purpose, methodology, and how results will be used. Avoid using audit data for punitive purposes unless serious safety issues are identified.
Implementation Insight:
Organizations that successfully overcome these challenges typically adopt a collaborative approach that engages frontline staff in all aspects of the audit cycle, from design to implementation of improvements. They also create a culture where audits are viewed as learning opportunities rather than punitive measures.
11. Case Studies: Successful Implementation of Nursing Audits
Examining real-world examples of successful nursing audit implementations provides valuable insights into effective strategies and potential outcomes.
Case Study 1: Abu Dhabi Hospital Documentation Audit
Background:
A hospital in Abu Dhabi implemented a systematic nursing documentation audit process to improve the quality of electronic health record documentation and ensure compliance with accreditation standards.
Approach:
- Established a dedicated documentation task force
- Developed comprehensive audit criteria based on hospital guidelines and accreditation requirements
- Created a standardized audit tool with clear instructions
- Conducted pilot testing and inter-rater reliability assessment
- Implemented regular audit cycle with feedback to staff
Challenges:
- No existing audit models in the region to follow
- Complexity of electronic documentation across multiple modules
- Time constraints for auditors
- Changing documentation requirements from authorities
Outcomes:
- Steady improvements in documentation compliance
- Enhanced standardization of documentation practices
- Better preparation for accreditation surveys
- Increased staff awareness of documentation requirements
Case Study 2: Comprehensive Nursing Performance Audit in University Hospital
Background:
A 500-bed university hospital implemented a comprehensive nursing performance audit program to improve care quality and patient satisfaction after noting declining HCAHPS scores over three consecutive quarters.
Approach:
- Conducted HCAHPS domain analysis to identify key areas for improvement
- Developed audit tools aligned with HCAHPS domains (nurse communication, responsiveness, pain management)
- Trained unit-based champions to conduct monthly mini-audits
- Implemented quarterly comprehensive audits by quality department
- Created visual management boards on units displaying audit results and improvement plans
- Developed targeted educational interventions based on audit findings
Challenges:
- Initial resistance from nursing staff
- Limited resources for conducting audits
- Difficulty connecting process measures to patient outcomes
- Competing quality initiatives
Outcomes:
- HCAHPS scores improved by 15% in nurse communication domain
- Staff responsiveness scores increased by 22%
- Pain management scores improved by 18%
- Overall hospital rating increased by 12%
- Reduced variability in practice across units
- Enhanced staff engagement in quality improvement
Case Study 3: Targeted Audit for Fall Prevention
Background:
A community hospital with higher-than-benchmark fall rates implemented a targeted nursing audit program focused specifically on fall prevention practices.
Approach:
- Developed audit tool addressing key fall prevention elements (risk assessment, interventions, rounding practices)
- Conducted weekly audits through direct observation and chart review
- Provided immediate feedback to staff during audits
- Implemented “huddle boards” for sharing audit results
- Used peer-to-peer education model for addressing gaps
- Linked audit findings to patient stories and outcomes
Challenges:
- Inconsistent risk assessment practices
- Difficulty sustaining improvement focus
- Time constraints for hourly rounding
- Environmental factors contributing to falls
Outcomes:
- Fall rate decreased by 40% over six months
- Falls with injury reduced by 65%
- Compliance with fall prevention protocols increased from 68% to 94%
- Patient satisfaction with safety measures improved
- Cost savings from prevented falls estimated at $380,000 annually
Key Lessons from Case Studies:
- Successful audit programs align with organizational priorities and patient needs
- Staff engagement at all levels is critical for implementation success
- Regular, timely feedback loops drive continuous improvement
- Connecting audit findings to patient outcomes increases motivation
- Targeted, focused audits often yield more meaningful improvements than broad, general audits
12. Conclusion: The Future of Nursing Performance Audits
Nursing performance audits and patient satisfaction assessment continue to evolve as essential components of healthcare quality management. As healthcare systems face increasing pressure to deliver high-quality, patient-centered care while managing resources effectively, the strategic implementation of nursing audits becomes ever more critical.
Key Takeaways
Integrated Approach
Effective nursing performance audits should be integrated with patient satisfaction assessment for a comprehensive view of care quality.
Systematic Process
Following a structured audit methodology with clear criteria, reliable measurement, and consistent feedback drives meaningful improvements.
Staff Engagement
Involving nursing staff at all levels of the audit process enhances buy-in, relevance, and implementation of improvements.
Patient-Centered Focus
Keeping patient outcomes and experiences at the center of audit processes ensures meaningful quality improvement.
Emerging Trends
- Digital Transformation: Increasing use of digital tools, AI, and automation to streamline audit processes and analyze patterns
- Real-Time Feedback: Movement toward continuous, real-time monitoring and feedback rather than periodic audits
- Patient Partnership: Greater involvement of patients and families in defining audit criteria and quality standards
- Integration with Big Data: Combining audit findings with other data sources for predictive analytics and proactive quality improvement
- Focus on Value: Evolution from process-focused to outcome and value-focused audit measures
Mnemonic: I-M-P-A-C-T
Key principles for effective nursing performance audits:
- Integrate with existing quality processes
- Measure what matters to patients and providers
- Promote a culture of continuous improvement
- Act on findings with specific improvement strategies
- Celebrate successes and progress
- Track outcomes over time to sustain gains
Final Thoughts
Nursing performance audits, when thoughtfully designed and implemented, provide a powerful mechanism for improving care quality and enhancing patient satisfaction. By systematically evaluating nursing practice against evidence-based standards, identifying opportunities for improvement, and implementing targeted changes, healthcare organizations can drive meaningful advancements in patient outcomes and experiences.
As healthcare continues to evolve, so too will audit methodologies and tools. However, the fundamental principles of systematic assessment, meaningful feedback, and continuous improvement will remain essential elements of high-quality nursing care. Organizations that embrace these principles and develop robust, patient-centered audit processes will be well-positioned to meet the challenges of tomorrow’s healthcare landscape while delivering exceptional care to the patients they serve.
