Nutrient Classification
Complete Guide for Nursing Students
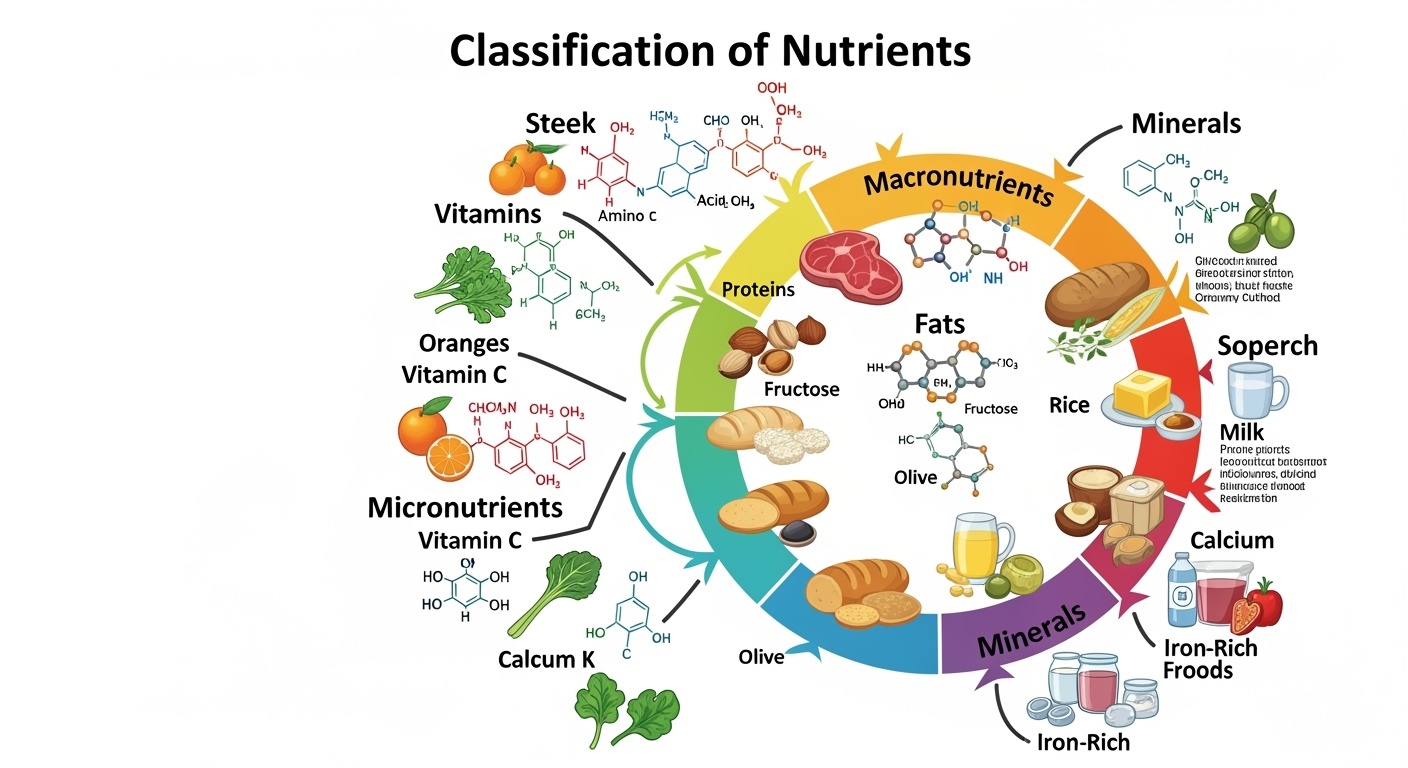
Visual representation of nutrient classification systems
Learning Objectives
By the end of this module, you will be able to:
- Classify nutrients into major categories
- Differentiate between macronutrients and micronutrients
- Distinguish organic from inorganic nutrients
- Identify energy-yielding vs non-energy yielding nutrients
Clinical Applications:
- Assess nutritional status in patients
- Plan therapeutic diets
- Recognize deficiency symptoms
- Provide patient education
Introduction to Nutrition
Nutrition is the cornerstone of health and healing, making it essential knowledge for every nursing professional. As a nurse, you’ll encounter patients across the spectrum of nutritional status—from those with severe malnutrition to individuals with obesity-related complications. Understanding nutrient classification provides the foundation for comprehensive patient care, therapeutic interventions, and health promotion strategies.
Nutrients are chemical substances found in food that are essential for growth, maintenance, and repair of body tissues. The human body requires approximately 50 different nutrients to function optimally, each playing specific roles in physiological processes. These nutrients can be classified in multiple ways, each classification system serving different clinical and educational purposes.
Clinical Relevance
Understanding nutrient classification enables nurses to identify patients at risk for specific deficiencies, plan appropriate interventions, and collaborate effectively with dietitians and physicians in developing comprehensive care plans.
Nutrient Classification Systems
Major Classification Systems
Quantity Needed
Macronutrients vs Micronutrients
Chemical Structure
Organic vs Inorganic
Energy Provision
Energy-yielding vs Non-energy yielding
Memory Aid – “QCE Classification”
Quantity (Macro/Micro) → Chemistry (Organic/Inorganic) → Energy (Yielding/Non-yielding)
Macronutrients: The Body’s Primary Building Blocks
Macronutrients are nutrients required by the body in large amounts (grams) and serve as the primary sources of energy and structural components. The three macronutrients—carbohydrates, proteins, and fats—each provide distinct functions and energy contributions to human physiology.
Carbohydrates
4 kcal/g
45-65% of total calories
Proteins
4 kcal/g
10-35% of total calories
Fats
9 kcal/g
20-35% of total calories
Carbohydrates
Classification:
- Simple Carbohydrates: Monosaccharides (glucose, fructose) and disaccharides (sucrose, lactose)
- Complex Carbohydrates: Polysaccharides (starch, glycogen, cellulose)
Primary Functions:
- • Primary energy source for brain and muscles
- • Protein-sparing action
- • Prevention of ketosis
- • Structural components (connective tissues)
Clinical Significance:
Monitor blood glucose levels, assess fiber intake for digestive health, evaluate carbohydrate counting in diabetes management.
Proteins
Classification:
- Complete Proteins: Contain all essential amino acids (animal sources)
- Incomplete Proteins: Missing one or more essential amino acids (plant sources)
Primary Functions:
- • Tissue building and repair
- • Enzyme and hormone synthesis
- • Immune system support
- • Fluid and pH balance maintenance
- • Energy source when carbohydrates are limited
Clinical Significance:
Assess wound healing, monitor albumin and prealbumin levels, evaluate nitrogen balance in critically ill patients.
Fats (Lipids)
Classification:
- Saturated Fats: No double bonds, solid at room temperature
- Unsaturated Fats: Contains double bonds, liquid at room temperature
- Trans Fats: Artificially hydrogenated, pro-inflammatory
Primary Functions:
- • Concentrated energy storage
- • Fat-soluble vitamin absorption
- • Cell membrane structure
- • Hormone production
- • Insulation and organ protection
Clinical Significance:
Monitor lipid profiles, assess essential fatty acid status, evaluate fat malabsorption syndromes.
Micronutrients: Essential in Small Amounts
Micronutrients are nutrients required in smaller quantities (milligrams or micrograms) but are essential for proper physiological function. They include vitamins and minerals, each playing crucial roles in metabolism, immune function, and cellular processes. Despite their small required amounts, deficiencies can have severe health consequences.
Vitamins (13 Essential)
- • Fat-soluble: A, D, E, K
- • Water-soluble: B-complex, C
- • Function as coenzymes and antioxidants
Minerals (15+ Essential)
- • Macrominerals: Ca, P, Mg, Na, K, Cl, S
- • Trace elements: Fe, Zn, Cu, I, Se, etc.
- • Structural and regulatory functions
Vitamin Classification and Functions
Fat-Soluble Vitamins (A, D, E, K)
Vitamin A (Retinol)
Vision, immune function, cell differentiation
Deficiency: Night blindness, xerophthalmia
Vitamin D (Calciferol)
Calcium absorption, bone health
Deficiency: Rickets, osteomalacia
Vitamin E (Tocopherol)
Antioxidant, membrane protection
Deficiency: Hemolytic anemia (rare)
Vitamin K (Phylloquinone)
Blood clotting, bone metabolism
Deficiency: Bleeding disorders
Water-Soluble Vitamins (B-Complex, C)
B1 (Thiamine)
Carbohydrate metabolism, nerve function
Deficiency: Beriberi, Wernicke-Korsakoff
B12 (Cobalamin)
DNA synthesis, nerve function
Deficiency: Pernicious anemia
Folate (B9)
DNA synthesis, cell division
Deficiency: Neural tube defects
Vitamin C (Ascorbic Acid)
Collagen synthesis, antioxidant
Deficiency: Scurvy
Mnemonic for Fat-Soluble Vitamins
“All Dogs Eat Kibble” = A, D, E, K
Remember: These vitamins are stored in fat and can accumulate to toxic levels
Essential Minerals and Their Functions
Macrominerals (>100mg/day needed)
Calcium (Ca)
Bone health, muscle contraction, nerve transmission
Deficiency: Osteoporosis, tetany
Iron (Fe)
Oxygen transport, energy metabolism
Deficiency: Iron-deficiency anemia
Sodium (Na)
Fluid balance, nerve transmission
Excess: Hypertension, fluid retention
Trace Elements (<15mg/day needed)
Zinc (Zn)
Immune function, wound healing, taste
Deficiency: Impaired healing, taste loss
Iodine (I)
Thyroid hormone synthesis
Deficiency: Goiter, hypothyroidism
Selenium (Se)
Antioxidant enzyme component
Deficiency: Cardiomyopathy (Keshan disease)
Organic vs Inorganic Nutrient Classification
Organic Nutrients
Contain carbon atoms in their molecular structure. These are primarily derived from living organisms and are more complex molecules.
Components:
- Carbohydrates
- Proteins
- Fats (Lipids)
- Vitamins
Characteristics:
- • Complex molecular structures
- • Can be broken down by heat
- • Susceptible to oxidation
- • Provide energy (except vitamins)
Inorganic Nutrients
Do not contain carbon atoms. These are simpler molecules that come from non-living sources like soil and water.
Components:
- Minerals
- Water
- Oxygen
Characteristics:
- • Simple molecular structures
- • Heat stable
- • Not easily destroyed
- • Do not provide energy
- • Essential for metabolic processes
Memory Aid: “COPY vs SIMPLE”
COPY = Organic nutrients:
Carbohydrates, Oils (fats), Proteins, Vitamins
SIMPLE = Inorganic nutrients:
Simple molecules like minerals and water
Energy-Yielding vs Non-Energy Yielding Nutrients
Energy-Yielding Nutrients
Provide calories (energy) when metabolized by the body. These nutrients can be oxidized to produce ATP, the body’s energy currency.
Carbohydrates 4 kcal/g
Primary and preferred energy source
Proteins 4 kcal/g
Secondary energy source, primarily structural
Fats 9 kcal/g
Most concentrated energy source
Alcohol 7 kcal/g
Not a nutrient but provides energy
Non-Energy Yielding Nutrients
Do not provide calories but are essential for metabolic processes, structural functions, and regulation of body systems.
Vitamins
Coenzymes and antioxidants for metabolic reactions
Minerals
Structural components and enzyme cofactors
Water
Medium for reactions, temperature regulation
Fiber
Digestive health, though some provides minimal energy
Clinical Alert: Energy Balance
Understanding energy-yielding nutrients is crucial for calculating caloric needs, managing weight, and preventing malnutrition in hospitalized patients. Total energy expenditure must match energy intake for weight maintenance.
Nursing Implementation and Clinical Applications
Assessment Strategies
-
Nutritional Screening: Use validated tools like MNA-SF or SGA to identify at-risk patients
-
Anthropometric Measurements: Monitor BMI, weight changes, and body composition
-
Laboratory Values: Track albumin, prealbumin, transferrin, and specific nutrient levels
-
Dietary History: Assess intake patterns, preferences, and cultural considerations
Intervention Planning
-
Meal Planning: Collaborate with dietitians to develop individualized nutrition plans
-
Supplementation: Identify needs for vitamin, mineral, or protein supplements
-
Patient Education: Provide culturally appropriate nutrition education
-
Monitoring: Track progress and adjust interventions based on outcomes
Special Populations and Considerations
Pediatric Patients
- • Higher protein needs per kg body weight
- • Critical periods for brain development
- • Growth velocity considerations
- • Age-appropriate food textures
Geriatric Patients
- • Decreased appetite and absorption
- • Polypharmacy interactions
- • Risk for sarcopenia
- • Hydration challenges
Critical Care
- • Hypermetabolic states
- • Enteral vs parenteral nutrition
- • Immune-enhancing nutrients
- • Glycemic control
Clinical Case Studies
Case 1: Iron Deficiency Anemia
Patient: 28-year-old female presenting with fatigue, pale conjunctiva, and Hgb 8.2 g/dL.
Nursing Assessment:
- • Dietary history reveals limited red meat intake
- • Heavy menstrual periods reported
- • Serum ferritin: 8 ng/mL (low)
- • TIBC elevated, transferrin saturation low
Interventions:
- • Educate on iron-rich foods (heme vs non-heme)
- • Vitamin C enhances iron absorption
- • Avoid tea/coffee with iron-rich meals
- • Monitor compliance with iron supplements
Case 2: Protein-Energy Malnutrition
Patient: 75-year-old male, post-surgical, with 15% weight loss over 3 months.
Assessment Findings:
- • Albumin: 2.8 g/dL (low)
- • Prealbumin: 12 mg/dL (low)
- • Poor wound healing observed
- • Decreased muscle mass
Nursing Actions:
- • Calculate protein needs (1.2-1.5 g/kg)
- • Collaborate for nutrition consult
- • Consider oral supplements
- • Monitor intake and output
Case 3: Diabetes Management
Patient: 52-year-old male with Type 2 diabetes, HbA1c 9.2%.
Nutritional Challenges:
- • High carbohydrate intake
- • Irregular meal timing
- • Limited understanding of glycemic index
- • Portion size misconceptions
Education Focus:
- • Carbohydrate counting methods
- • Plate method for portion control
- • Complex vs simple carbohydrates
- • Timing of meals with medications
Nutritional Assessment Tools for Nurses
Screening Tools
Mini Nutritional Assessment (MNA)
Validated tool for elderly patients, assesses:
- • Anthropometric measurements
- • General assessment
- • Dietary assessment
- • Subjective assessment
MUST (Malnutrition Universal Screening Tool)
Five-step screening process:
- • BMI calculation
- • Weight loss percentage
- • Acute disease effect
- • Overall risk calculation
- • Management guidelines
Laboratory Markers
Protein Status Indicators
Micronutrient Markers
Essential Memory Aids and Mnemonics
Classification Mnemonics
Fat-Soluble Vitamins
“All Dogs Eat Kibble”
A, D, E, K – stored in fat
Energy Values
“4-4-9-7”
CHO-Protein-Fat-Alcohol kcal/g
Organic Nutrients
“COPY”
Carbs, Oils, Proteins, Vitamins
Clinical Memory Aids
Iron Deficiency Signs
“TIRED”
Tired, Ice cravings, Restless legs, Excessive menstrual bleeding, Decreased concentration
B12 Deficiency
“BEAM”
Balance problems, Elevated MCV, Anemia, Memory loss
Protein Assessment
“APT”
Albumin, Prealbumin, Transferrin
Key Takeaways for Nursing Practice
Assessment Excellence
- • Use validated screening tools consistently
- • Monitor anthropometric and laboratory markers
- • Assess cultural and socioeconomic factors
- • Document findings comprehensively
- • Identify high-risk populations early
Intervention Strategies
- • Collaborate with interdisciplinary team
- • Individualize nutrition plans
- • Provide evidence-based education
- • Monitor patient response to interventions
- • Adjust plans based on outcomes
Patient Advocacy
- • Recognize nutritional needs across lifespan
- • Address barriers to adequate nutrition
- • Promote health literacy and empowerment
- • Ensure access to appropriate resources
- • Support patient autonomy in food choices
Clinical Pearl
Remember: Nutrition is not just about food—it’s about healing, recovery, and quality of life. Every patient interaction is an opportunity to assess, educate, and intervene. Your knowledge of nutrient classification directly impacts patient outcomes and your ability to provide holistic, evidence-based care.
References and Evidence Base
Professional Guidelines
- • Academy of Nutrition and Dietetics Evidence Analysis Library
- • American Society for Parenteral and Enteral Nutrition (ASPEN)
- • Institute of Medicine Dietary Reference Intakes
- • WHO Global Strategy on Diet, Physical Activity and Health
- • Joint Commission Standards on Nutrition Care
Key Learning Resources
- • Nutrition Care Process and Model (NCPM)
- • Malnutrition Clinical Characteristics Consensus
- • Critical Care Nutrition Practice Guidelines
- • Pediatric and Geriatric Nutrition Considerations
- • Cultural Competency in Nutrition Care
Note: This educational material is based on current evidence-based practice and professional standards. Always consult current clinical guidelines and collaborate with registered dietitians for complex nutritional assessments and interventions.
