Nutrition During Labour: Evidence-Based Guidelines for Optimal Maternal Care
Comprehensive nursing notes on maternal nutrition during labor to promote positive childbirth experiences
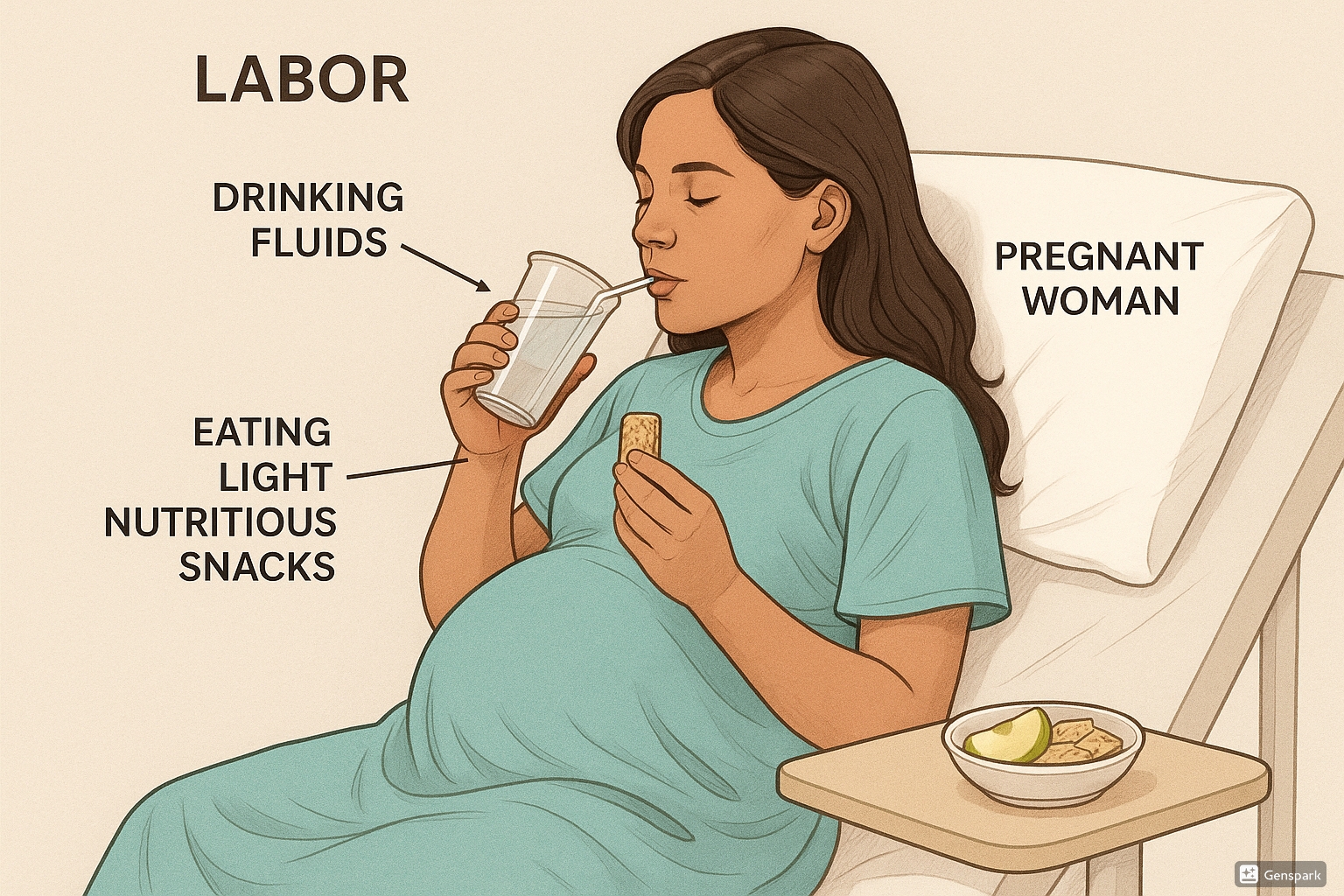
Maternal nutrition during labor plays a crucial role in promoting positive birth experiences and supporting the physiological demands of childbirth. These comprehensive notes examine evidence-based guidelines for nutritional support during labor, with practical applications for nursing care.
Table of Contents
Physiological Needs During Labor
Labor is an intense physical activity comparable to running a marathon, requiring significant energy expenditure and proper hydration. Understanding the physiological basis for nutritional support is essential for providing evidence-based care.
Key Physiological Considerations:
- Uterine muscle requires adequate energy to maintain effective contractions
- Prolonged fasting may lead to ketosis, making stomach contents more acidic
- Laboring women can burn 50-100 calories per hour during active labor
- Dehydration can contribute to maternal exhaustion and prolonged labor
- Energy needs during labor are similar to those of endurance athletes
Metabolic Changes During Labor
During labor, the body experiences increased metabolic demands. The uterus, primarily composed of muscle tissue, requires adequate glucose and oxygen for optimal functioning. Research in sports nutrition indicates that carbohydrate ingestion during prolonged physical exertion improves performance and prevents fatigue and ketosis.
Studies have indicated that restricting oral intake during labor can lead to:
- Increased stress hormones
- Decreased insulin sensitivity
- Higher levels of free fatty acids
- Increased ketone production
- Potential maternal exhaustion
Evidence-Based Guidelines
Current evidence strongly supports that low-risk laboring women should have the right to decide whether they want to eat or drink during labor. Several professional organizations have established guidelines for maternal nutrition during labor.
| Organization | Recommendations | Year Updated |
|---|---|---|
| World Health Organization (WHO) | Recommends that low-risk pregnant women consume energy and fluids throughout labor as a means of reducing cesarean section rates | 1997, reaffirmed |
| American College of Nurse-Midwives (ACNM) | Supports oral nutrition for women in labor with uncomplicated pregnancies | 2016 |
| NICE (UK) | Recommends that drinks and light meals be offered to low-risk women in labor | 2014 |
| Society of Obstetricians and Gynecologists of Canada (SOGC) | Endorses oral intake for women with uncomplicated labor | 2016 |
| American College of Obstetricians and Gynecologists (ACOG) | Recommends allowing clear liquids for low-risk women; advises against solid foods during active labor (under review) | 2019, Reaffirmed 2021 |
| American Society of Anesthesiologists (ASA) | Supports clear liquids for low-risk laboring women; recommends avoiding solid foods during active labor | 2016 |
The historical “Nothing by Mouth” (NPO) policy during labor originated in the 1940s when general anesthesia was routinely used without modern airway protection methods. Today, the risk of aspiration during childbirth is extremely rare (approximately 1 in 1.4 million births in modern practice), calling into question restrictive feeding policies.
M – Mendelson’s syndrome described in 1946
O – Outdated practice from when general anesthesia was common
D – Danger of aspiration is now extremely rare (1 in 1.4 million)
E – Epidurals have largely replaced general anesthesia
R – Regional anesthesia is now standard for most cesarean births
N – New evidence supports eating and drinking for low-risk women
Recommended Foods and Fluids
Evidence suggests that maternal nutrition during labor should focus on easily digestible foods that provide quick energy and adequate hydration. Below are recommendations based on current research.
| Category | Recommended Options | Benefits During Labor |
|---|---|---|
| Carbohydrate-based fluids | Sports drinks, fruit juices, coconut water, clear broths | Quick energy, electrolyte replacement, hydration |
| Natural sugars | Honey sticks, date fruit, date syrup, fruit smoothies | Rapid glucose availability, sustained energy |
| Light proteins | Low-fat yogurt, light cheese | Sustained energy, muscle support |
| Simple carbohydrates | Toast with jam, crackers, cereal with milk, tortillas with honey | Energy provision, easily digestible |
| Fruits and vegetables | Bananas, applesauce, melon, roasted vegetables | Hydration, vitamins, easy digestion |
| Quick-energy foods | Chocolate, energy bars (low in fat), popsicles | Glucose boost, temperature regulation, comfort |
General Guidelines for Maternal Nutrition During Labor:
- Consume familiar foods that are unlikely to cause digestive discomfort
- Choose items that provide energy without being heavy or difficult to digest
- Prioritize hydration throughout all stages of labor
- Consider culturally appropriate foods that provide comfort
- Listen to hunger and thirst cues; most laboring women naturally limit intake as labor progresses
Special Nutritional Considerations
Women with Diabetes (Gestational or Pre-existing)
Nutritional management for laboring women with diabetes requires special attention to blood glucose control. Labor itself has a glucose-lowering effect similar to exercise.
Key Considerations for Women with Diabetes:
- Women who normally require insulin should have adjusted protocols during labor
- Blood glucose monitoring should be performed hourly during active labor
- For medical inductions, eat approximately 50% of normal caloric intake during the cervical ripening period
- Avoid high-sugar clear fluids which can cause blood glucose spikes
- Consult with the diabetes management team for individualized protocols
High-Risk Pregnancies
Certain conditions may increase the risk of complications during labor and delivery, potentially requiring more conservative approaches to maternal nutrition during labor.
Higher risk factors that may influence nutritional decisions include:
- Severe pre-eclampsia or eclampsia
- BMI of 40 or greater
- Use of intravenous opioids for pain management
- Anticipated difficult airway management
- Increased likelihood of emergency cesarean delivery
Even with these risk factors, current evidence suggests that clear fluids are generally safe in most circumstances, and individualized nutritional plans should be considered rather than blanket restrictions.
Best Practices and Recent Updates
Recent Update (2022): Evidence-based practice emphasizes that laboring women have the fundamental right to decide whether they would like to eat or drink during labor. Hospital policies restricting this choice are not legally binding on patients. Nurses should advocate for patient autonomy while providing education on evidence-based options.
Recent Update (2021): ACOG reaffirmed their recommendation that low-risk women should have access to moderate amounts of clear liquids during labor. Even women with epidurals can safely consume clear fluids. A recent study by Bouvet et al. (2022) found that epidural use actually improved gastric emptying compared to laboring without an epidural, contradicting previous assumptions.
Recent Update (2023): New nursing guidelines emphasize the importance of supporting culturally diverse food preferences during labor. Cultural foods should not be dismissed as “unhealthy” or “inappropriate” based on the personal biases of healthcare providers. Nurses should address their own implicit biases about food and respect the cultural significance of nutritional choices during the birth experience.
Clinical Benefits of Appropriate Maternal Nutrition During Labor
Evidence from clinical studies and meta-analyses has identified several potential benefits when laboring women are allowed to eat and drink according to their preferences:
- Shorter labor duration by approximately 16 minutes (Ciardulli et al., 2017)
- Increased maternal satisfaction with the birth experience
- Reduced perception of pain and environmental stress
- Prevention of dehydration and ketosis
- Promotion of maternal autonomy and sense of control
- Avoidance of unnecessary intravenous fluid administration
Nursing Implications
Nurses play a critical role in supporting optimal maternal nutrition during labor. Understanding both the physiological requirements and the evidence-based guidelines enables nurses to provide comprehensive care.
Assessment
- Evaluate the laboring woman’s risk factors that might impact nutritional needs
- Assess pre-existing conditions like diabetes or hypertension
- Review labor progress and projected energy needs
- Monitor for signs of dehydration or ketosis
- Evaluate the woman’s preferences for food and fluids during labor
Nursing Interventions
- Advocate for evidence-based nutritional protocols that support maternal choice
- Provide education on the benefits and risks of eating/drinking during labor
- Offer appropriate food and fluid options based on labor stage and risk assessment
- Document oral intake and tolerance
- Monitor for nausea or vomiting that might increase aspiration risk
- Support cultural preferences in food and drink choices
- Coordinate with the healthcare team regarding individual nutritional plans
Documentation
- Record type and amount of oral intake
- Document maternal response to nutrition/hydration
- Note any discussions regarding nutritional preferences or restrictions
- Record signs of dehydration, ketosis, or other nutritional concerns
- Document educational information provided to the woman and family
N – Needs assessment (individual risk factors and preferences)
O – Offer evidence-based options for nutrition
U – Understand cultural preferences and respect maternal choice
R – Recognize signs of dehydration or ketosis
I – Inform about benefits and potential risks
S – Support autonomy in decision-making
H – Hydration monitoring throughout labor
Memory Aids for Nursing Students
W – World Health Organization
A – American College of Nurse-Midwives
N – NICE (UK)
S – Society of Obstetricians and Gynecologists of Canada
S – Sports drinks (electrolytes)
I – Isotonic beverages
M – Minimal fat content foods
P – Protein in small amounts
L – Light carbohydrates
E – Easy to digest options
A – Anesthesia type (regional vs. general)
S – Specific risk factors (BMI, preeclampsia)
P – Pain medication (IV opioids increase risk)
I – Induction or spontaneous labor
R – Risk category (low vs. high)
E – Expected mode of delivery
References
- American College of Obstetricians and Gynecologists. (2019, Reaffirmed 2021). Approaches to limit intervention during labor and birth. ACOG Committee Opinion No. 766. https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2019/02/approaches-to-limit-intervention-during-labor-and-birth
- American Society of Anesthesiologists. (2016). Practice guidelines for obstetric anesthesia. https://www.asahq.org/standards-and-practice-parameters/statement-on-oral-intake-during-labor
- Bouvet, L., Chassard, D., Benhamou, D., & Boselli, E. (2022). Effect of epidural analgesia on gastric emptying of a light meal in term pregnant women: A prospective ultrasound study. Anesthesiology, 136(4), 542-550.
- Ciardulli, A., Saccone, G., Anastasio, H., & Berghella, V. (2017). Less-restrictive food intake during labor in low-risk singleton pregnancies: A systematic review and meta-analysis. Obstetrics & Gynecology, 129(3), 473-480.
- Evidence Based Birth. (2022). Evidence on: Eating and drinking during labor. https://evidencebasedbirth.com/evidence-eating-drinking-labor/
- Liang, J., Mu, Y., Li, X., Tang, W., Wang, Y., Liu, Z., … & Liang, J. (2021). The nutritional and fluid intake preferences during labor: A survey. Birth, 48(4), 578-587.
- McDermott, H., Mullen, A., & Byrne, M. (2022). Eating and drinking during labour: A survey of women’s preferences and experiences. Midwifery, 107, 103276.
- Singata, M., Tranmer, J., & Gyte, G. M. (2013). Restricting oral fluid and food intake during labour. Cochrane Database of Systematic Reviews, (8).
- World Health Organization. (1997). Care in normal birth: A practical guide. Report of a technical working group. https://www.who.int/maternal_child_adolescent/documents/who_frh_msm_9624/en/
© 2025 Nutrition During Labour: Evidence-Based Guidelines for Optimal Maternal Care. These nursing notes are designed for educational purposes only. Clinical practice should always follow institutional policies and the most current evidence-based guidelines.
