Oral Care in Nursing: Essential Practices for Patient Hygiene, Comfort & Health
Comprehensive Guide for Nursing Students and Healthcare Professionals
Table of Contents
of hospitalized patients develop oral complications
reduction in pneumonia risk with proper oral care
daily oral care frequency recommended
patient comfort improvement with regular oral care
1. Introduction to Oral Care in Nursing
Foundation of Patient-Centered Care
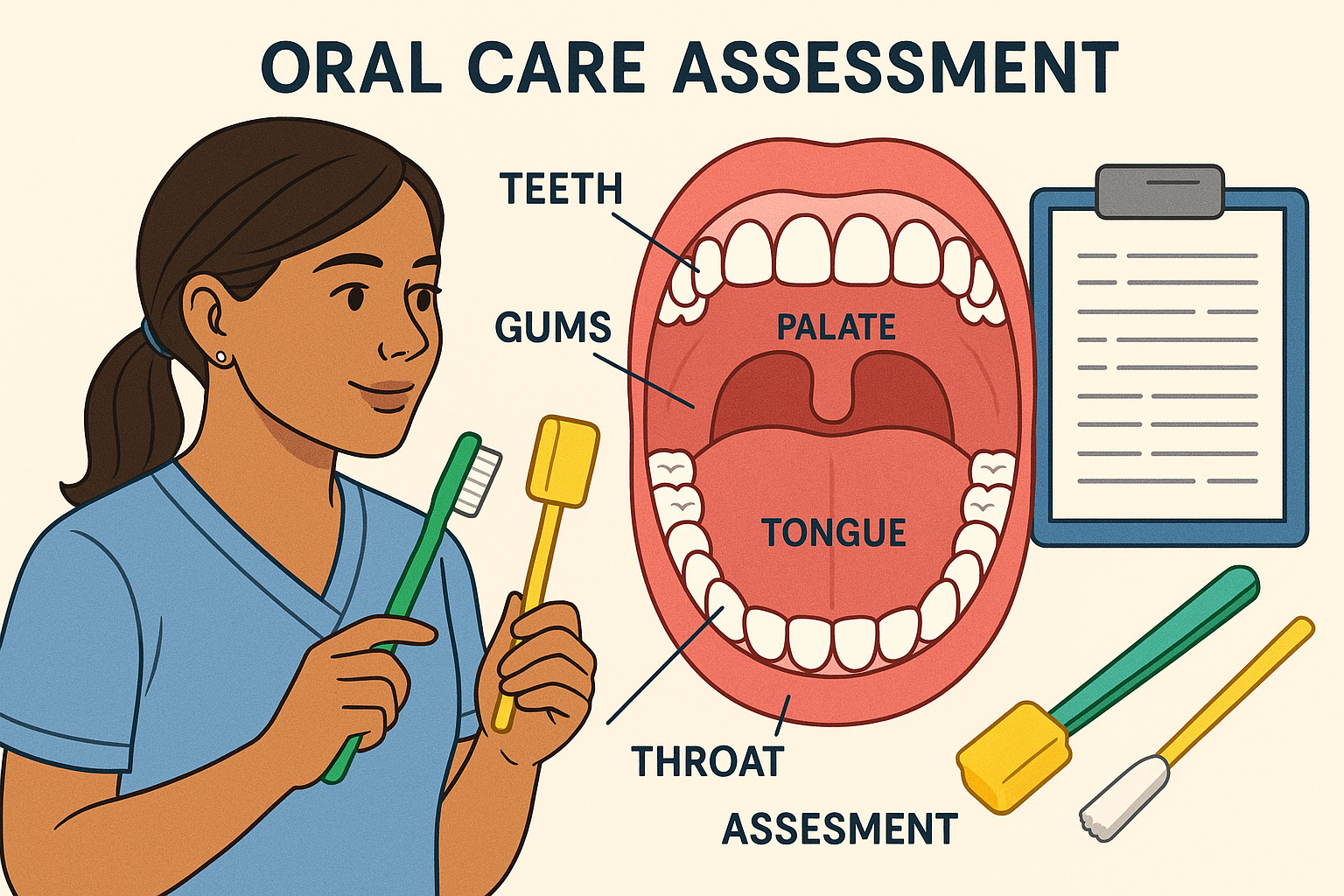
Professional nursing illustration showing oral care assessment with labeled anatomical parts and nursing tools
Oral care represents one of the most fundamental yet critical aspects of nursing practice. It encompasses the systematic assessment, maintenance, and restoration of oral health to promote patient comfort, prevent complications, and enhance overall quality of life. As healthcare professionals, nurses play a pivotal role in ensuring that patients receive comprehensive oral care that addresses both immediate needs and long-term health outcomes.
Key Learning Objectives
- Understand the physiological and psychological importance of oral care in healthcare settings
- Master comprehensive oral assessment techniques and documentation methods
- Develop proficiency in evidence-based oral care interventions for diverse patient populations
- Implement infection control measures and safety protocols during oral care procedures
2. Importance of Oral Care
Beyond Basic Hygiene
Physical Health Benefits
-
Infection Prevention: Regular oral care significantly reduces bacterial colonization, decreasing the risk of ventilator-associated pneumonia and other respiratory infections.
-
Cardiovascular Health: Oral bacteria can enter the bloodstream, potentially causing endocarditis and other cardiovascular complications.
-
Nutritional Support: Healthy oral tissues enable proper mastication and swallowing, supporting adequate nutrition.
Psychological Well-being
-
Self-Esteem: Clean, healthy oral tissues contribute to positive self-image and confidence.
-
Communication: Proper oral health enables clear speech and social interaction.
-
Comfort: Relief from oral discomfort improves sleep quality and overall patient experience.
Memory Aid: SMILE
3. Oral Anatomy and Physiology
Understanding the Foundation
Teeth Structure
- Enamel: Hardest substance in body
- Dentin: Calcified tissue beneath enamel
- Pulp: Contains nerves and blood vessels
- Cementum: Covers tooth root
Gingiva (Gums)
- Free gingiva: Surrounds tooth crown
- Attached gingiva: Firmly bound to bone
- Alveolar mucosa: Movable tissue
- Interdental papilla: Between teeth
Tongue
- Dorsal surface: Upper surface with papillae
- Ventral surface: Underneath, highly vascular
- Lateral borders: Sides of tongue
- Tip: Most mobile portion
Oral Cavity
- Hard palate: Roof of mouth
- Soft palate: Posterior roof
- Uvula: Hangs from soft palate
- Buccal mucosa: Cheek lining
Clinical Significance
Understanding normal oral anatomy is crucial for accurate assessment. Deviations from normal appearance, texture, or function may indicate underlying pathology requiring immediate attention and appropriate nursing interventions.
4. Oral Assessment Techniques
Systematic Evaluation Approach
Assessment Framework
Comprehensive oral care assessment should follow a systematic approach to ensure nothing is missed. The assessment should be conducted in adequate lighting with proper equipment and infection control measures.
| Assessment Area | Normal Findings | Abnormal Findings | Nursing Actions |
|---|---|---|---|
| Lips | Pink, moist, intact | Dry, cracked, swollen, lesions | Apply lip balm, hydrate, report lesions |
| Teeth | Clean, intact, properly aligned | Decay, loose, missing, plaque buildup | Gentle brushing, dental referral |
| Gums | Pink, firm, no bleeding | Red, swollen, bleeding, recession | Soft brush, antiseptic rinse, document |
| Tongue | Pink, moist, papillae present | Coated, smooth, ulcers, discoloration | Gentle cleaning, positioning, hydration |
| Mucosa | Pink, moist, smooth | Dry, ulcers, white patches, bleeding | Moisturize, protective measures, report |
| Saliva | Adequate flow, clear | Decreased, thick, discolored | Hydration, saliva substitutes, stimulation |
Assessment Mnemonic: LIPS
Assessment Frequency
5. Equipment and Supplies
Essential Tools for Effective Care
Basic Equipment
Specialized Supplies
Safety Equipment
Gloves
Disposable, non-latex preferred
Face Protection
Masks and eye protection
Barrier Protection
Gowns when indicated
Equipment Considerations
Always ensure equipment is appropriate for individual patient needs. Oral care supplies should be patient-specific to prevent cross-contamination. Replace toothbrushes regularly and after illness resolution.
6. Oral Care Procedures
Step-by-Step Implementation
Standard Oral Care Procedure
Preparation and Safety
Gather all necessary supplies and ensure proper hand hygiene. Don appropriate personal protective equipment including gloves and face protection.
Patient Positioning
Position patient in semi-Fowler’s position (45-60 degrees) or turn head to side if supine. This prevents aspiration and facilitates drainage.
- • Ensure patient comfort and accessibility
- • Protect clothing with towels
- • Have suction available if needed
Initial Assessment
Conduct thorough visual inspection of oral cavity before beginning care. Document any abnormalities or concerns.
Brushing Technique
Use gentle, circular motions with soft-bristled toothbrush. Apply minimal pressure to avoid tissue damage while ensuring effective plaque removal.
- • 45-degree angle to gum line
- • Small circular motions
- • 2-3 minutes duration
- • Tongue surface
- • Gum line carefully
- • Inner cheek surfaces
Rinsing and Moisturizing
Provide opportunity for rinsing with water or appropriate mouthwash. Apply lip balm to prevent dryness and cracking.
Documentation and Follow-up
Complete accurate documentation of oral care provided, patient response, and any abnormal findings requiring further attention.
Procedure Mnemonic: BRUSH
7. Special Populations
Tailored Approaches for Unique Needs
Unconscious Patients
Unconscious patients require modified oral care approaches to prevent aspiration while maintaining oral hygiene. Special attention must be paid to positioning and technique.
Modified Techniques
- • Use oral swabs instead of toothbrush
- • Position patient on side
- • Avoid excessive moisture
- • Use suction for secretion removal
- • Check for gag reflex presence
Safety Considerations
- • Continuous monitoring during procedure
- • Suction equipment readily available
- • Avoid forceful manipulation
- • Document neurological status
- • Collaborate with respiratory therapy
Mechanically Ventilated Patients
Patients on mechanical ventilation require specialized oral care protocols to prevent ventilator-associated pneumonia and maintain comfort.
| Intervention | Frequency | Special Considerations |
|---|---|---|
| Oral assessment | Every 4 hours | Check around ET tube, secretions |
| Tooth brushing | Every 12 hours | Gentle technique, avoid tube displacement |
| Antiseptic rinse | Every 6 hours | Chlorhexidine 0.12% solution |
| Lip care | Every 2 hours | Prevent dryness around tube |
| Suction | As needed | Remove secretions, maintain airway |
Patients with Dentures
Denture care requires specific techniques and considerations to maintain both prosthetic integrity and oral health.
Daily Care
- • Remove and clean separately
- • Use denture cleanser
- • Handle carefully to avoid damage
- • Store in water when not worn
Tissue Care
- • Clean gums and tongue
- • Massage gum tissues
- • Check for sore spots
- • Allow tissue rest periods
Assessment Points
- • Fit and comfort
- • Tissue irritation
- • Prosthetic integrity
- • Patient adaptation
8. Common Complications
Prevention and Management
Ventilator-Associated Pneumonia (VAP)
Risk Factors
- • Poor oral hygiene
- • Bacterial colonization
- • Compromised immunity
- • Prolonged intubation
- • Aspiration of secretions
Prevention Strategies
- • Regular oral care every 6 hours
- • Chlorhexidine antiseptic rinse
- • Proper positioning (HOB elevation)
- • Suction secretions appropriately
- • Monitor for signs of infection
Xerostomia (Dry Mouth)
Common Causes
- • Medications (anticholinergics)
- • Dehydration
- • Radiation therapy
- • Systemic diseases
- • Mouth breathing
Clinical Signs
- • Sticky, thick saliva
- • Difficulty swallowing
- • Altered taste
- • Increased thirst
- • Oral discomfort
Management
- • Frequent hydration
- • Saliva substitutes
- • Sugar-free gum/candy
- • Humidification
- • Medication review
Oral Candidiasis (Thrush)
Fungal infection commonly seen in immunocompromised patients
Mucositis
Inflammation of mucous membranes, common in chemotherapy
9. Nursing Interventions
Evidence-Based Practice Guidelines
Intervention Hierarchy
Nursing interventions for oral care should follow evidence-based guidelines and be individualized based on patient assessment and risk factors.
Preventive Care
- • Regular assessment
- • Routine hygiene maintenance
- • Risk factor identification
- • Patient education
- • Environmental modifications
Therapeutic Care
- • Targeted interventions
- • Medication administration
- • Specialized products
- • Comfort measures
- • Symptom management
Emergency Care
- • Immediate assessment
- • Rapid intervention
- • Complication management
- • Collaborative care
- • Continuous monitoring
Intervention Protocols
| Risk Level | Patient Population | Intervention Frequency | Specific Actions |
|---|---|---|---|
| Low | Conscious, cooperative patients | Twice daily | Standard oral hygiene, education |
| Moderate | Post-operative, elderly | Three times daily | Assisted care, soft brush, monitoring |
| High | ICU, immunocompromised | Every 6 hours | Specialized products, frequent assessment |
| Critical | Ventilated, unconscious | Every 4 hours | Intensive protocol, antiseptic rinse |
Quality Indicators
- • Completion of scheduled oral care
- • Appropriate technique utilization
- • Timely documentation
- • Patient comfort during procedure
- • Reduced infection rates
- • Improved patient satisfaction
- • Decreased complications
- • Enhanced quality of life
10. Documentation
Accurate Recording and Communication
Documentation Requirements
Comprehensive documentation of oral care is essential for continuity of care, legal protection, and quality improvement initiatives. All interventions must be accurately recorded.
Required Elements
- Date and time of care provided
- Assessment findings and oral condition
- Interventions performed and products used
- Patient response and tolerance
- Any complications or adverse events
- Follow-up actions or referrals needed
Documentation Best Practices
- • Use objective, descriptive language
- • Document immediately after care
- • Include patient’s own words when relevant
- • Note any teaching provided
- • Record interdisciplinary communications
- • Follow facility-specific guidelines
Sample Documentation Examples
Normal Findings
“0800: Oral care completed. Oral cavity assessed – lips pink and moist, teeth clean with no visible decay, gums pink without bleeding, tongue pink with normal papillae, adequate saliva production. Patient tolerated procedure well, no discomfort reported. Used soft-bristled toothbrush with fluoride toothpaste, followed by water rinse. Patient educated on importance of regular oral hygiene.”
Abnormal Findings
“1400: Oral assessment reveals dry, cracked lips and thick, sticky saliva. Patient reports mouth feeling ‘very dry’ and difficulty swallowing. Oral care provided with gentle foam swabs and mouth moisturizer. Lip balm applied. Increased fluid intake encouraged. MD notified of xerostomia symptoms. Will monitor closely and reassess in 4 hours.”
Documentation Mnemonic: SOAP
11. Global Best Practices
International Standards and Innovations
International Guidelines
Healthcare systems worldwide have developed comprehensive oral care protocols based on evidence-based research and clinical outcomes. These practices demonstrate significant improvements in patient outcomes and quality of care.
Netherlands Healthcare System
Dutch healthcare facilities have implemented comprehensive oral care protocols that include specialized oral hygienist roles in hospital settings. Their approach emphasizes prevention and early intervention.
Key Features:
- • Dedicated oral hygienists in ICUs
- • Standardized assessment tools
- • Technology integration for monitoring
- • Interdisciplinary team approach
Outcomes:
- • 45% reduction in VAP rates
- • Improved patient satisfaction scores
- • Decreased length of stay
- • Lower healthcare costs
Japanese Healthcare Excellence
Japan’s healthcare system emphasizes meticulous oral care protocols with focus on precision, consistency, and patient comfort. Their approach integrates traditional care principles with modern technology.
Innovation Highlights:
Bacterial Monitoring: Real-time oral bacteria assessment
Automated Systems: Precision oral care devices
Quality Metrics: Continuous improvement tracking
Scandinavian Approach
Nordic countries have developed patient-centered oral care models that emphasize dignity, comfort, and individualized care plans. Their holistic approach considers physical, emotional, and social aspects of oral health.
Patient-Centered Features:
- • Individualized care plans
- • Patient preference consideration
- • Family involvement in care
- • Cultural sensitivity training
- • Comfort-first protocols
Implementation Success:
- • 95% patient satisfaction rates
- • Reduced oral complications
- • Enhanced staff competency
- • Improved quality indicators
- • Cost-effective outcomes
Emerging Technologies
Mobile Health Apps
Digital tools for assessment documentation and patient education
AI-Powered Assessment
Artificial intelligence for early detection of oral complications
Advanced Materials
Innovative oral care products with enhanced effectiveness
12. Conclusion
Commitment to Excellence in Patient Care
Oral care in nursing practice represents far more than routine hygiene maintenance. It embodies a fundamental commitment to patient dignity, comfort, and health promotion. Through systematic assessment, evidence-based interventions, and compassionate care delivery, nurses can significantly impact patient outcomes and quality of life.
Key Takeaways
- Comprehensive assessment is the foundation of effective oral care
- Evidence-based protocols improve patient outcomes significantly
- Individual patient needs require tailored interventions
- Infection prevention is a primary benefit of proper oral care
- Documentation ensures continuity and quality improvement
Future Directions
- Integration of advanced technologies in oral care
- Expansion of specialized oral hygienist roles
- Development of personalized care protocols
- Enhanced interdisciplinary collaboration
- Continuous education and competency development
Final Reflection: CARE
“Excellence in oral care is not just about maintaining oral health—it’s about preserving dignity, promoting comfort, and demonstrating the highest standards of nursing practice.”
