🫁 Pancreatic Cyst: Complete Nursing Guide
Comprehensive Medical Notes for Nursing Students
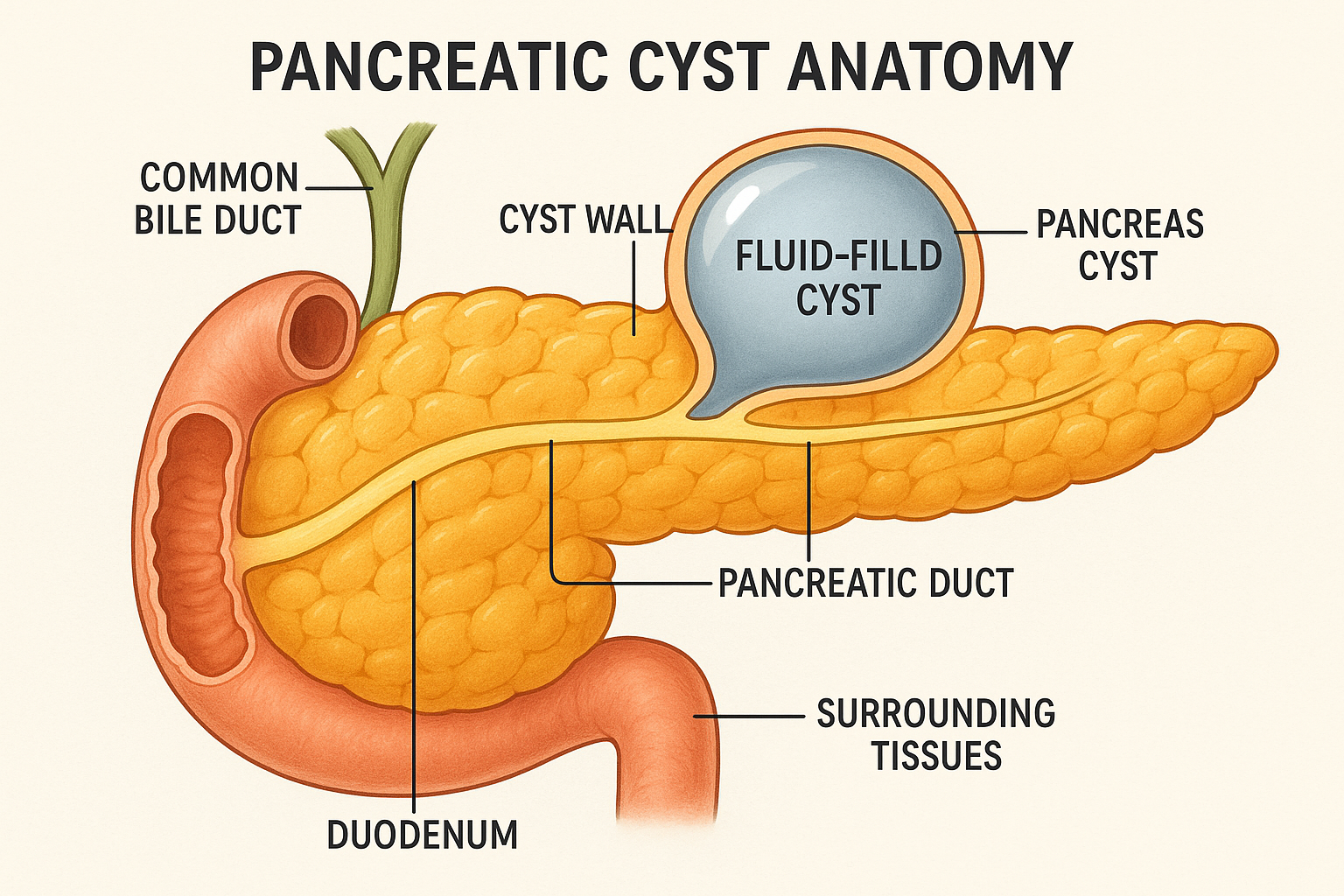
🔍 Overview and Definition
A pancreatic cyst is a fluid-filled sac that develops within or on the pancreas, an essential organ located behind the stomach in the upper abdomen. These cystic lesions represent a diverse group of pathological conditions that can range from benign pseudocysts to potentially malignant neoplastic cysts. Understanding pancreatic cysts is crucial for nursing professionals as they require careful assessment, monitoring, and patient education to ensure optimal outcomes.
🎯 Key Definition
A pancreatic cyst is defined as any fluid-containing space within the pancreatic parenchyma or peripancreatic area, which may be lined by epithelium (true cyst) or lack epithelial lining (pseudocyst). These lesions can vary significantly in size, location, and clinical significance.
💎 Clinical Pearl
Not all pancreatic cysts are created equal! While many are benign, some have malignant potential. The key is understanding the different types and their clinical significance to provide appropriate nursing care and patient education.
🫀 Anatomy and Pathophysiology
Pancreatic Anatomy Review
The pancreas is a vital organ measuring approximately 12-15 cm in length, weighing 70-100 grams in adults. It consists of four main anatomical regions:
| Anatomical Region | Location | Key Features | Clinical Significance |
|---|---|---|---|
| Head | Right side, surrounded by duodenum | Contains uncinate process | Most common site for pancreatic cyst formation |
| Neck | Anterior to superior mesenteric vessels | Narrowed portion | Can be compressed by cystic lesions |
| Body | Central portion, crosses midline | Contains main pancreatic duct | Second most common cyst location |
| Tail | Extends to splenic hilum | Contains islets of Langerhans | Cysts here may affect splenic vessels |
Ductal System
The pancreatic ductal system plays a crucial role in pancreatic cyst development:
- Main Pancreatic Duct (Wirsung): Runs through the entire pancreas, collecting secretions
- Accessory Duct (Santorini): Drains the upper head region
- Secondary Ducts: Branch from main duct, can become dilated in cystic conditions
🧠 Mnemonic: DUCT
Dilation occurs with obstruction
Uncinate process commonly affected
Cysts can compress adjacent structures
Tail region affects splenic vessels
📊 Classification and Types
Pancreatic cysts are broadly classified into two main categories based on their pathological characteristics and clinical behavior. Understanding this classification is essential for nursing professionals to provide appropriate care and education.
Non-neoplastic Cysts
| Type | Characteristics | Etiology | Malignant Potential |
|---|---|---|---|
| Pseudocysts | No epithelial lining, inflammatory origin | Pancreatitis, trauma | None |
| Retention Cysts | Ductal obstruction | Strictures, stones | None |
| Congenital Cysts | Developmental anomalies | Genetic factors | Very low |
Neoplastic Cysts
| Type | Characteristics | Malignant Potential | Key Features |
|---|---|---|---|
| Serous Cystadenomas | Benign, multiple small cysts | Very low (<1%) | Honeycomb appearance on imaging |
| Mucinous Cystadenomas | Mucin-producing, larger cysts | Moderate (10-15%) | Thick mucin content |
| IPMN | Intraductal papillary mucinous neoplasm | Variable (5-60%) | Communicates with pancreatic duct |
| Solid Pseudopapillary | Mixed solid-cystic, young women | Low but exists | Encapsulated, hemorrhagic |
🔑 Key Classification Points
- Pseudocysts account for 85-90% of all pancreatic cysts
- Neoplastic cysts require closer monitoring due to malignant potential
- Size, location, and imaging characteristics help differentiate types
- Patient age and gender can provide diagnostic clues
⚡ Etiology and Risk Factors
Understanding the various causes and risk factors for pancreatic cyst development is crucial for prevention, early detection, and appropriate nursing interventions.
Primary Etiological Factors
🔥 Inflammatory Causes
- Acute Pancreatitis: Most common cause of pseudocysts (85% of cases)
- Chronic Pancreatitis: Long-term inflammation leading to ductal changes
- Autoimmune Pancreatitis: IgG4-related disease
⚠️ Traumatic Causes
- Blunt Abdominal Trauma: Motor vehicle accidents, falls
- Penetrating Trauma: Stab wounds, gunshot wounds
- Iatrogenic Injury: Post-surgical complications, endoscopic procedures
Risk Factor Analysis
| Risk Category | Specific Factors | Relative Risk | Nursing Implications |
|---|---|---|---|
| Lifestyle | Alcohol abuse, smoking | High | Counseling, cessation programs |
| Genetic | CFTR mutations, hereditary pancreatitis | Very High | Family screening, genetic counseling |
| Medical | Gallstones, medications, infections | Moderate | Medication review, infection prevention |
| Demographic | Age >40, male gender | Low-Moderate | Increased surveillance, education |
🧠 Mnemonic: PANCREAS
Pancreatitis (most common)
Alcohol abuse
Neoplastic transformation
Congenital anomalies
Retention from obstruction
Endocrine disorders
Autoimmune conditions
Surgical complications
🔬 Pathogenesis
The development of a pancreatic cyst involves complex pathophysiological mechanisms that vary depending on the underlying etiology. Understanding these processes helps nurses anticipate complications and provide appropriate interventions.
Pseudocyst Formation Mechanism
💎 Pathophysiological Sequence
- Initial Injury: Pancreatic ductal disruption or parenchymal necrosis
- Enzyme Release: Pancreatic enzymes leak into surrounding tissues
- Inflammatory Response: Tissue necrosis and inflammatory cell infiltration
- Fluid Collection: Pancreatic juice accumulates in damaged area
- Wall Formation: Fibrous capsule develops over 4-6 weeks
- Maturation: Cyst wall matures and may communicate with pancreatic duct
Neoplastic Cyst Development
Neoplastic cysts follow a different pathogenesis involving cellular transformation and growth:
- Genetic Mutations: Oncogene activation and tumor suppressor gene inactivation
- Cellular Proliferation: Abnormal cell growth and division
- Mucin Production: Excessive mucin secretion in mucinous lesions
- Cystic Degeneration: Central necrosis and fluid accumulation
Molecular Pathways
| Pathway | Key Molecules | Function | Clinical Relevance |
|---|---|---|---|
| Inflammatory | TNF-α, IL-1β, IL-6 | Tissue damage and repair | Pseudocyst formation |
| Growth Factor | VEGF, PDGF, TGF-β | Angiogenesis and fibrosis | Cyst wall development |
| Oncogenic | KRAS, p53, SMAD4 | Cell cycle regulation | Neoplastic transformation |
🔑 Pathogenesis Key Points
- Pseudocyst maturation requires 4-6 weeks for fibrous wall formation
- Communication with pancreatic duct affects healing and complications
- Neoplastic cysts may undergo malignant transformation over time
- Location within pancreas influences drainage and symptom development
🩺 Clinical Manifestations
The clinical presentation of pancreatic cyst varies significantly based on size, location, type, and associated complications. Many patients remain asymptomatic, while others present with severe symptoms requiring immediate intervention.
Symptom Categories
🔴 Primary Symptoms
- Abdominal Pain: Most common symptom (60-90% of patients)
- Epigastric Discomfort: Dull, aching pain radiating to back
- Early Satiety: Due to gastric compression
- Nausea and Vomiting: Especially with larger cysts
Specific Clinical Signs
| Clinical Sign | Description | Frequency | Clinical Significance |
|---|---|---|---|
| Palpable Mass | Upper abdominal fullness or mass | 20-50% | Suggests larger cyst (>5 cm) |
| Jaundice | Yellow discoloration of skin/sclera | 5-15% | Indicates biliary obstruction |
| Weight Loss | Unintentional weight reduction | 10-30% | May suggest malignancy |
| Steatorrhea | Fatty, foul-smelling stools | 5-20% | Pancreatic enzyme insufficiency |
| Diabetes | New-onset glucose intolerance | 5-15% | Pancreatic endocrine dysfunction |
Location-Specific Manifestations
💎 Head of Pancreas Cysts
- Biliary obstruction and jaundice
- Duodenal compression
- Portal vein compression
- Common bile duct dilation
💎 Body/Tail Cysts
- Gastric outlet obstruction
- Splenic vein thrombosis
- Left-sided portal hypertension
- Splenic artery pseudoaneurysm
Complication-Related Signs
⚠️ Emergency Presentations
- Acute Abdomen: Cyst rupture or perforation
- Hematemesis: Bleeding into GI tract
- Shock: Massive bleeding or sepsis
- Fever with Chills: Infected cyst
🧠 Mnemonic: CYST PAIN
Compression symptoms
Yellow skin (jaundice)
Steatorrhea
Tender epigastrium
Palpable mass
Abdominal distension
Indigestion
Nausea and vomiting
🔍 Nursing Assessment
Comprehensive nursing assessment of patients with suspected or confirmed pancreatic cyst requires systematic evaluation of multiple body systems and careful monitoring for complications. The assessment should be thorough yet efficient, focusing on key indicators that may signal deterioration or improvement.
Primary Assessment Framework
🎯 ABCDE Assessment Priority
- Airway: Usually not compromised unless severe vomiting
- Breathing: Assess for splinting due to abdominal pain
- Circulation: Monitor for signs of bleeding or shock
- Disability: Neurological status, pain assessment
- Exposure: Complete abdominal examination
Systematic Physical Assessment
| Assessment Area | Key Findings | Normal vs. Abnormal | Nursing Actions |
|---|---|---|---|
| Inspection | Abdominal distension, asymmetry | Flat vs. distended, symmetric vs. asymmetric | Document changes, measure girth |
| Auscultation | Bowel sounds, bruits | Normal vs. absent/hyperactive | Listen for 2 minutes, note quality |
| Percussion | Tympany, dullness | Tympanic vs. dull percussion | Map areas of dullness |
| Palpation | Masses, tenderness, guarding | Soft vs. rigid, non-tender vs. tender | Light then deep palpation |
Pain Assessment
💎 Comprehensive Pain Evaluation
- Location: Epigastric, left upper quadrant, radiating to back
- Quality: Dull, aching, burning, cramping
- Intensity: Use 0-10 numerical rating scale
- Duration: Acute, chronic, intermittent, constant
- Aggravating factors: Food intake, positioning, movement
- Relieving factors: Medications, positioning, rest
Vital Signs Monitoring
| Parameter | Normal Range | Concerning Changes | Potential Causes |
|---|---|---|---|
| Blood Pressure | 120/80 mmHg | Hypotension <90/60 | Bleeding, sepsis, dehydration |
| Heart Rate | 60-100 bpm | Tachycardia >100 | Pain, anxiety, hypovolemia |
| Temperature | 98.6°F (37°C) | Fever >101°F | Infection, inflammation |
| Respirations | 12-20 per minute | Tachypnea >24 | Pain, anxiety, splinting |
Nutritional Assessment
🔑 Nutritional Status Indicators
- Weight Changes: Document baseline and trends
- Albumin Levels: Indicator of protein status
- Dietary Intake: Assess appetite and tolerance
- Stool Characteristics: Note color, consistency, frequency
- Fat-Soluble Vitamins: A, D, E, K deficiency signs
🧠 Mnemonic: ASSESS
Abdominal examination
Symptom severity
Signs of complications
Extraabdominal manifestations
Systemic symptoms
Support system evaluation
🔬 Diagnostic Studies
Accurate diagnosis of pancreatic cyst requires a combination of clinical assessment, laboratory studies, and advanced imaging techniques. Understanding these diagnostic modalities helps nurses prepare patients, interpret results, and monitor for complications.
Laboratory Studies
| Laboratory Test | Normal Values | Expected Changes | Clinical Significance |
|---|---|---|---|
| Amylase | 30-110 U/L | May be elevated | Pancreatic inflammation or ductal obstruction |
| Lipase | 10-140 U/L | Often elevated | More specific for pancreatic pathology |
| Bilirubin | 0.2-1.0 mg/dL | Elevated if obstructed | Biliary obstruction from head cysts |
| CA 19-9 | <37 U/mL | Variable elevation | Tumor marker, not specific |
| CEA | <2.5 ng/mL | May be elevated | Mucinous cyst marker |
Imaging Studies
🎯 Primary Imaging Modalities
- CT Scan: First-line imaging, excellent anatomical detail
- MRI/MRCP: Superior soft tissue contrast, ductal evaluation
- Ultrasound: Initial screening, real-time assessment
- Endoscopic Ultrasound (EUS): High-resolution pancreatic imaging
Advanced Diagnostic Procedures
| Procedure | Indication | Information Obtained | Nursing Considerations |
|---|---|---|---|
| EUS-FNA | Tissue sampling | Cytology, tumor markers | NPO, consent, post-procedure monitoring |
| ERCP | Ductal evaluation | Pancreatic duct anatomy | Pancreatitis risk, NPO, sedation |
| Cyst Fluid Analysis | Cyst characterization | Amylase, CEA, cytology | Sterile technique, specimen handling |
Imaging Characteristics by Cyst Type
💎 Imaging Pearls
- Pseudocysts: Well-defined, no solid components, low CEA
- Serous Cystadenomas: Honeycomb appearance, central scar
- Mucinous Lesions: Thick walls, high CEA, septations
- IPMN: Ductal communication, “string of beads” sign
Nursing Responsibilities
🔑 Pre-Procedure Nursing Care
- Patient Preparation: NPO status, allergies, medications
- Education: Explain procedure, expectations, risks
- Consent: Ensure informed consent obtained
- Baseline Assessment: Vital signs, pain level, anxiety
⚠️ Post-Procedure Monitoring
- Vital Signs: Monitor for bleeding, perforation
- Pain Assessment: Distinguish normal from concerning pain
- Complications: Watch for pancreatitis, infection
- Diet Advancement: Clear liquids to regular diet as tolerated
⚕️ Medical Management
The management of pancreatic cyst varies significantly based on cyst type, size, symptoms, and malignant potential. Treatment options range from conservative observation to surgical intervention, requiring individualized care plans and multidisciplinary collaboration.
Conservative Management
🎯 Observation Criteria
- Small Size: Less than 3 cm diameter
- Asymptomatic: No pain or complications
- Benign Characteristics: Imaging suggests low malignant potential
- Stable Appearance: No growth over time
Pharmacological Management
| Medication Category | Examples | Indication | Nursing Considerations |
|---|---|---|---|
| Analgesics | Morphine, Fentanyl | Pain control | Monitor respiratory status, addiction risk |
| Proton Pump Inhibitors | Omeprazole, Pantoprazole | Gastric protection | Monitor for drug interactions |
| Antibiotics | Ciprofloxacin, Metronidazole | Infected cysts | Culture sensitivity, allergies |
| Pancreatic Enzymes | Pancrelipase | Exocrine insufficiency | Take with meals, monitor stool |
| Insulin | Various types | Diabetes management | Blood glucose monitoring |
Interventional Procedures
💎 Minimally Invasive Options
- Percutaneous Drainage: Large symptomatic pseudocysts
- Endoscopic Drainage: Cystogastrostomy or cystoduodenostomy
- EUS-Guided Drainage: Precise needle placement
- Cyst Aspiration: Diagnostic and sometimes therapeutic
Surgical Management
| Surgical Procedure | Indication | Approach | Recovery Considerations |
|---|---|---|---|
| Distal Pancreatectomy | Body/tail cysts, malignant potential | Open or laparoscopic | Diabetes risk, splenic preservation |
| Pancreaticoduodenectomy | Head cysts, malignancy suspected | Open surgery (Whipple) | Complex recovery, multiple anastomoses |
| Central Pancreatectomy | Neck/body lesions | Parenchyma-sparing | Pancreatic fistula risk |
| Enucleation | Small benign cysts | Minimally invasive | Lower morbidity |
Treatment Algorithm
🧠 Treatment Decision Mnemonic: SIZE
Symptoms present = intervention
Imaging characteristics = risk stratification
Zone location = surgical approach
Evaluation over time = surveillance
Multidisciplinary Team Approach
🔑 Team Members and Roles
- Gastroenterologist: Endoscopic procedures, medical management
- Surgeon: Operative interventions, complex cases
- Radiologist: Imaging interpretation, interventional procedures
- Oncologist: Malignant cases, chemotherapy
- Nurse: Coordination, education, symptom management
- Dietitian: Nutritional support, enzyme therapy
👩⚕️ Nursing Care and Interventions
Comprehensive nursing care for patients with pancreatic cyst requires expertise in symptom management, patient education, and prevention of complications. Nurses play a crucial role in coordinating care, monitoring patient status, and providing emotional support throughout the treatment journey.
Priority Nursing Diagnoses
| Nursing Diagnosis | Related Factors | Expected Outcomes | Key Interventions |
|---|---|---|---|
| Acute Pain | Cyst pressure, inflammation | Pain score <4/10 | Analgesic administration, positioning |
| Imbalanced Nutrition | Malabsorption, decreased intake | Stable weight, adequate intake | Enzyme replacement, dietary counseling |
| Risk for Infection | Invasive procedures, immunocompromise | No signs of infection | Sterile technique, monitoring |
| Anxiety | Fear of cancer, uncertain prognosis | Reduced anxiety levels | Education, support, referrals |
Pain Management Strategies
💎 Multimodal Pain Approach
- Pharmacological: Opioids, NSAIDs, adjuvant medications
- Non-pharmacological: Heat therapy, positioning, relaxation
- Interventional: Nerve blocks, drainage procedures
- Complementary: Acupuncture, massage, meditation
Nutritional Support
🎯 Nutritional Interventions
- Enzyme Replacement: Pancrelipase with meals and snacks
- Diet Modification: Small frequent meals, fat-soluble vitamins
- Caloric Density: High-calorie, high-protein foods
- Monitoring: Weight trends, laboratory values
Pre-Operative Nursing Care
| Assessment Area | Key Elements | Interventions | Documentation |
|---|---|---|---|
| Physical Status | Vital signs, pain, nutrition | Optimize medical conditions | Baseline assessments |
| Psychological | Anxiety, coping, support | Education, counseling | Mental health screening |
| Educational | Procedure understanding | Teaching, reinforcement | Learning outcomes |
| Preparation | NPO, bowel prep, consent | Protocol adherence | Checklist completion |
Post-Operative Nursing Care
⚠️ Critical Monitoring Parameters
- Vital Signs: Hourly initially, then per protocol
- Pain Assessment: Regular scoring, intervention effectiveness
- Drainage: Output characteristics, patency
- Laboratory Values: Glucose, electrolytes, enzymes
- Complications: Bleeding, infection, pancreatic fistula
Complication Prevention
🔑 Prevention Strategies
- Infection Prevention: Hand hygiene, sterile technique, antibiotic prophylaxis
- Thromboembolism: Early mobilization, compression devices, anticoagulation
- Respiratory: Incentive spirometry, deep breathing, positioning
- Skin Integrity: Pressure relief, moisture management, nutrition
Discharge Planning
💎 Discharge Readiness Criteria
- Stable Vital Signs: No fever, stable blood pressure
- Pain Control: Manageable with oral medications
- Oral Intake: Tolerating regular diet
- Mobility: Independent or with assistance
- Understanding: Demonstrates self-care knowledge
🧠 Nursing Care Mnemonic: PANCREAS
Pain management
Assessment comprehensive
Nutrition support
Complications prevention
Respiratory care
Education provision
Anxiety reduction
Support systems
⚠️ Complications
Patients with pancreatic cyst may develop various complications ranging from minor to life-threatening. Understanding these potential complications is essential for early recognition, prompt intervention, and improved patient outcomes.
Acute Complications
| Complication | Incidence | Clinical Signs | Emergency Management |
|---|---|---|---|
| Cyst Rupture | 5-10% | Severe abdominal pain, peritonitis | Immediate surgery, fluid resuscitation |
| Hemorrhage | 10-15% | Hematemesis, melena, shock | Blood products, endoscopic control |
| Infection | 15-20% | Fever, leukocytosis, sepsis | Antibiotics, drainage, supportive care |
| Obstruction | 20-30% | Biliary or gastric outlet symptoms | Decompression, stenting, surgery |
Chronic Complications
🎯 Long-term Sequelae
- Diabetes Mellitus: Endocrine pancreatic insufficiency
- Malabsorption: Exocrine pancreatic insufficiency
- Chronic Pain: Nerve involvement, inflammation
- Malignant Transformation: Neoplastic cysts risk
Procedure-Related Complications
| Procedure | Specific Complications | Prevention Strategies | Management |
|---|---|---|---|
| Endoscopic Drainage | Perforation, bleeding, infection | Careful technique, antibiotic prophylaxis | Conservative vs. surgical repair |
| Surgical Resection | Pancreatic fistula, delayed gastric emptying | Gentle tissue handling, drainage | Conservative management, nutrition |
| Percutaneous Drainage | Catheter displacement, infection | Secure fixation, sterile technique | Catheter adjustment, antibiotics |
Recognition and Assessment
⚠️ Red Flag Symptoms
- Sudden Severe Pain: May indicate rupture or bleeding
- Hemodynamic Instability: Shock, hypotension, tachycardia
- High Fever: Temperature >101.5°F with chills
- Jaundice: Progressive biliary obstruction
- Peritoneal Signs: Guarding, rebound tenderness
Nursing Interventions for Complications
💎 Early Detection Strategies
- Frequent Assessment: Vital signs, pain, abdominal exam
- Laboratory Monitoring: CBC, chemistry panel, coagulation
- Imaging Surveillance: Serial CT or ultrasound
- Patient Education: Warning signs, when to seek help
Multisystem Impact
🔑 System-Specific Effects
- Cardiovascular: Shock, arrhythmias from electrolyte imbalance
- Respiratory: Pleural effusion, respiratory compromise
- Renal: Acute kidney injury from hypoperfusion
- Hematologic: Coagulopathy, thrombocytopenia
- Neurologic: Altered mental status from sepsis
🧠 Complication Mnemonic: BLEEDS
Bleeding into cyst or GI tract
Leakage and peritonitis
Erosion into adjacent organs
Endocrine dysfunction
Duodenal obstruction
Sepsis and infection
📚 Patient Education
Effective patient education is fundamental to successful management of pancreatic cyst. Nurses must provide comprehensive, culturally sensitive education that empowers patients to participate actively in their care and make informed decisions about treatment options.
Core Educational Components
🎯 Essential Knowledge Areas
- Disease Understanding: What is a pancreatic cyst
- Treatment Options: Conservative vs. interventional approaches
- Symptom Management: Pain control, dietary modifications
- Monitoring Requirements: Follow-up schedules, warning signs
Teaching Strategies
| Learning Style | Teaching Methods | Resources | Evaluation Methods |
|---|---|---|---|
| Visual | Diagrams, videos, written materials | Anatomical models, imaging studies | Return demonstration, written quiz |
| Auditory | Verbal explanations, discussions | Audio recordings, group sessions | Verbal feedback, teach-back method |
| Kinesthetic | Hands-on practice, demonstrations | Practice kits, simulation | Skill demonstration, competency |
Dietary Education
💎 Nutritional Guidelines
- Enzyme Therapy: Take with first bite of meals and snacks
- Fat-Soluble Vitamins: A, D, E, K supplementation
- Small Frequent Meals: 6 small meals better than 3 large
- Alcohol Avoidance: Complete cessation recommended
- High-Calorie Foods: Compensate for malabsorption
Medication Management
| Medication Category | Key Teaching Points | Side Effects | Monitoring |
|---|---|---|---|
| Pain Medications | Take as prescribed, don’t skip doses | Drowsiness, constipation, addiction | Pain scores, bowel function |
| Pancreatic Enzymes | Must take with all meals and snacks | Nausea, abdominal cramping | Stool consistency, weight |
| Insulin | Proper injection technique, storage | Hypoglycemia, weight gain | Blood glucose levels |
Warning Signs Education
⚠️ When to Seek Immediate Medical Attention
- Severe Abdominal Pain: Sudden onset, unrelieved by medications
- Vomiting Blood: Fresh red blood or coffee-ground appearance
- High Fever: Temperature >101.5°F with chills
- Yellowing Skin: Progressive jaundice
- Severe Weakness: Unable to perform daily activities
Lifestyle Modifications
🔑 Lifestyle Recommendations
- Smoking Cessation: Reduces pancreatic cancer risk
- Alcohol Avoidance: Prevents further pancreatic damage
- Regular Exercise: As tolerated, improves overall health
- Stress Management: May help with pain control
- Regular Follow-up: Adherence to surveillance schedule
Support Resources
💎 Patient Support Systems
- Support Groups: Pancreatic disease organizations
- Online Resources: Reputable medical websites
- Counseling Services: Psychological support
- Financial Resources: Insurance navigation, assistance programs
- Family Education: Include caregivers in teaching
🧠 Education Mnemonic: TEACH
Tune in to patient needs
Edit information for understanding
Act on teaching opportunities
Clarify and confirm understanding
Honor cultural preferences
📈 Prognosis and Outcomes
The prognosis for patients with pancreatic cyst varies significantly depending on the type of cyst, size, location, patient factors, and treatment approach. Understanding prognostic factors helps nurses provide appropriate education and support to patients and families.
Prognostic Factors
| Factor | Favorable Prognosis | Unfavorable Prognosis | Clinical Impact |
|---|---|---|---|
| Cyst Type | Pseudocyst, serous cystadenoma | Mucinous lesions, IPMN | Malignant potential varies |
| Size | Small (<3 cm) | Large (>5 cm) | Complications increase with size |
| Symptoms | Asymptomatic | Symptomatic, complications | Quality of life impact |
| Age | Younger patients | Elderly patients | Surgical risk, comorbidities |
Outcomes by Cyst Type
🎯 Type-Specific Prognosis
- Pseudocysts: 40-60% resolve spontaneously within 6 weeks
- Serous Cystadenomas: Excellent prognosis, <1% malignancy risk
- Mucinous Lesions: 10-30% malignancy risk, requires monitoring
- IPMN: Variable risk based on features and location
Surgical Outcomes
| Procedure | Mortality Rate | Morbidity Rate | Long-term Outcomes |
|---|---|---|---|
| Distal Pancreatectomy | 1-3% | 20-30% | Good quality of life |
| Pancreaticoduodenectomy | 2-5% | 40-50% | Functional impairment possible |
| Endoscopic Drainage | <1% | 10-20% | Symptom relief in 80-90% |
Long-term Complications
💎 Chronic Sequelae
- Diabetes: 10-30% develop new-onset diabetes
- Malabsorption: 15-25% require enzyme replacement
- Chronic Pain: 20-40% experience ongoing pain
- Recurrence: 5-15% recurrence rate after treatment
Quality of Life Factors
🔑 Factors Affecting Quality of Life
- Pain Control: Adequate analgesia improves function
- Nutritional Status: Maintaining weight and strength
- Psychological Health: Anxiety and depression management
- Social Support: Family and community resources
- Functional Independence: Ability to perform daily activities
Surveillance and Monitoring
| Risk Category | Surveillance Interval | Imaging Modality | Duration |
|---|---|---|---|
| Low Risk | Annual | MRI or CT | 5 years |
| Moderate Risk | 6-12 months | MRI with MRCP | Indefinite |
| High Risk | 3-6 months | EUS or MRI | Until intervention |
⚠️ Poor Prognostic Indicators
- Rapid Growth: >2 mm/year increase in size
- Solid Components: Development of mural nodules
- New Symptoms: Pain, weight loss, jaundice
- CA 19-9 Elevation: Rising tumor marker levels
🧠 Prognosis Mnemonic: HOPE
Histology determines risk
Outcomes vary by type
Patient factors matter
Early detection improves prognosis
🌍 Global Best Practices
Healthcare systems worldwide have developed innovative approaches to managing pancreatic cyst care. These international best practices offer valuable insights for improving patient outcomes and healthcare delivery.
European Approach – Netherlands
🎯 Dutch Pancreatic Cyst Surveillance Program
The Netherlands has implemented a nationwide surveillance program for pancreatic cystic lesions that emphasizes:
- Centralized Care: Specialized pancreatic centers for complex cases
- Risk Stratification: Evidence-based surveillance protocols
- Patient Registries: National database for outcomes tracking
- Multidisciplinary Teams: Standardized tumor board approach
Asian Innovation – Japan
💎 Japanese IPMN Management Guidelines
Japan, with high IPMN prevalence, has developed sophisticated management strategies:
- AI-Enhanced Imaging: Machine learning for cyst characterization
- Genetic Testing: Routine screening for high-risk families
- Minimally Invasive Surgery: Laparoscopic techniques advancement
- Patient Education Programs: Community-based health promotion
North American Excellence – Mayo Clinic Model
🔑 Integrated Care Model
- Team-Based Care: Nurse practitioners in specialty roles
- Telehealth Integration: Remote monitoring and consultations
- Patient Portal Systems: Electronic communication and education
- Quality Metrics: Continuous improvement programs
Developing World Solutions – India
| Challenge | Innovation | Implementation | Outcomes |
|---|---|---|---|
| Resource Limitations | Point-of-care ultrasound | Training rural healthcare workers | Earlier detection, reduced costs |
| Geographic Barriers | Mobile health units | Scheduled community visits | Improved access to care |
| Cost Constraints | Tiered treatment protocols | Risk-based resource allocation | Cost-effective care delivery |
Research and Innovation Centers
💎 Leading Research Initiatives
- Johns Hopkins: Genetic markers for cyst progression
- Memorial Sloan Kettering: Liquid biopsy development
- University of Pittsburgh: Artificial pancreas research
- Heidelberg University: Regenerative medicine approaches
Technology Integration
🎯 Digital Health Solutions
- Australia: National e-health records for continuity
- South Korea: AI-powered diagnostic assistance
- Germany: Wearable devices for symptom monitoring
- Canada: Virtual reality for patient education
Quality Improvement Initiatives
⚠️ Key Performance Indicators
- Diagnostic Accuracy: >95% correct cyst characterization
- Surveillance Compliance: >80% adherence to follow-up
- Patient Satisfaction: >90% satisfaction scores
- Complication Rates: <5% major complications
Future Directions
🔑 Emerging Trends
- Precision Medicine: Personalized treatment based on genetics
- Biomarker Development: Blood tests for cyst monitoring
- Robotic Surgery: Enhanced precision and recovery
- Immunotherapy: Novel treatments for malignant cysts
- Prevention Strategies: Lifestyle interventions and screening
Pancreatic cyst
management continues to evolve through international collaboration, technological advancement, and patient-centered care approaches. These global best practices demonstrate the importance of standardized protocols, multidisciplinary care, and continuous quality improvement in achieving optimal patient outcomes.