🩺 Pancreatitis: Complete Nursing Guide
Comprehensive Medical Notes for Nursing Students
🎯 Overview & Definition
Pancreatitis is an inflammatory condition of the pancreas characterized by activation of pancreatic enzymes within the pancreatic tissue, leading to autodigestion and tissue damage. This serious medical condition requires immediate nursing intervention and comprehensive patient care management.
Key Definition
Pancreatitis occurs when digestive enzymes become activated while still in the pancreas, causing the organ to essentially digest itself. This inflammatory process can range from mild swelling to severe tissue damage and systemic complications.
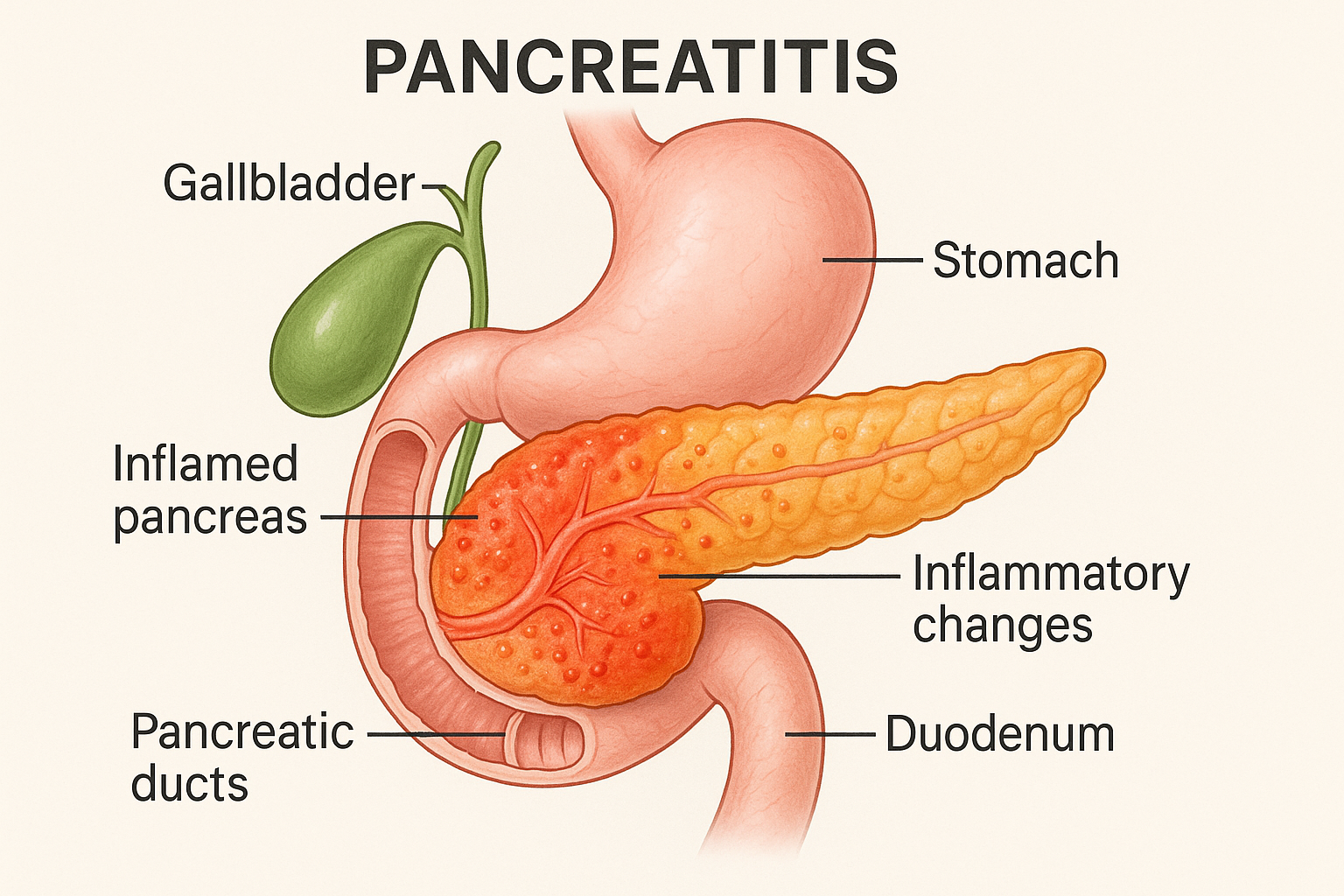
Figure 1: Anatomical illustration showing inflamed pancreas with surrounding organs and inflammatory changes
🔬 Pancreatic Anatomy & Physiology
Anatomical Structure
The pancreas is a mixed endocrine and exocrine gland located in the retroperitoneal space. Understanding its anatomy is crucial for recognizing how pancreatitis affects organ function.
| Pancreatic Region | Location | Function | Clinical Significance |
|---|---|---|---|
| Head | Adjacent to duodenum | Houses common bile duct | Most common site for tumors |
| Body | Central portion | Main digestive enzyme production | Primary site of inflammatory changes |
| Tail | Near spleen | Endocrine function (islets) | Associated with splenic complications |
Physiological Functions
🔹 Exocrine Function
Produces digestive enzymes including lipase, amylase, and proteases essential for nutrient breakdown
🔹 Endocrine Function
Secretes insulin and glucagon for blood glucose regulation through pancreatic islets
🔹 Bicarbonate Production
Neutralizes acidic chyme from stomach to protect duodenal mucosa
🔍 Etiology & Risk Factors
🧠 MNEMONIC: GET SMASHED
Primary Causes
🥃 Alcohol-Related Pancreatitis
Chronic alcohol consumption is responsible for approximately 70% of chronic pancreatitis cases. Alcohol directly damages pancreatic acinar cells and increases protein concentration in pancreatic secretions.
🪨 Gallstone Pancreatitis
Accounts for 40-50% of acute pancreatitis cases. Gallstones obstruct the ampulla of Vater, causing pancreatic duct pressure elevation and enzyme activation.
| Risk Category | Specific Factors | Mechanism | Prevention Strategy |
|---|---|---|---|
| Lifestyle | Alcohol abuse, smoking | Direct toxicity | Cessation counseling |
| Metabolic | Hyperlipidemia, diabetes | Metabolic dysfunction | Dietary management |
| Genetic | CFTR mutations, hereditary | Enzyme dysfunction | Genetic counseling |
| Iatrogenic | ERCP, medications | Procedural trauma | Risk assessment |
High-Risk Medications
Several medications can trigger pancreatitis: azathioprine, mercaptopurine, pentamidine, didanosine, valproic acid, and furosemide. Always review medication history during assessment.
⚙️ Pathophysiology
The pathophysiological cascade of pancreatitis involves premature activation of pancreatic enzymes, leading to autodigestion and progressive tissue damage.
Acute Pancreatitis Progression
Stage 1: Initial Injury
Pancreatic duct obstruction or direct cellular damage triggers enzyme activation within pancreatic tissue
Stage 2: Enzyme Activation
Trypsinogen converts to trypsin, activating other digestive enzymes leading to autodigestion
Stage 3: Inflammatory Response
Release of inflammatory mediators causes increased vascular permeability and tissue edema
Stage 4: Systemic Effects
Systemic inflammatory response syndrome (SIRS) may develop with multi-organ involvement
Chronic Pancreatitis Development
Chronic pancreatitis involves progressive fibrosis and permanent structural damage. The inflammatory process leads to:
- Pancreatic Fibrosis: Replacement of normal tissue with scar tissue
- Ductal Strictures: Narrowing of pancreatic ducts impeding enzyme flow
- Calcifications: Calcium deposits within pancreatic tissue
- Functional Loss: Decreased enzyme and hormone production
Enzyme Cascade Effects
Activated pancreatic enzymes cause specific damage: lipase breaks down fat cells, elastase damages blood vessel walls, and phospholipase A destroys cell membranes, contributing to the severity of pancreatitis.
📊 Classification Types
| Type | Duration | Reversibility | Key Features |
|---|---|---|---|
| Acute Pancreatitis | Days to weeks | Potentially reversible | Sudden onset, severe pain |
| Chronic Pancreatitis | Months to years | Irreversible | Progressive fibrosis |
| Acute-on-Chronic | Variable | Partially reversible | Acute flare of chronic disease |
Severity Classification (Atlanta Classification)
🟢 Mild Pancreatitis
No organ failure, no local complications, usually resolves within one week
🟡 Moderately Severe
Transient organ failure or local complications without persistent organ failure
🔴 Severe Pancreatitis
Persistent organ failure (>48 hours), high mortality risk, requires intensive care
🩺 Clinical Manifestations
Primary Signs and Symptoms
Classic Triad of Pancreatitis
- Severe epigastric pain – Often radiating to the back
- Nausea and vomiting – Persistent and projectile
- Elevated pancreatic enzymes – Serum amylase and lipase
🔥 Pain Characteristics
The hallmark symptom of pancreatitis is severe abdominal pain with specific characteristics:
| Pain Feature | Description | Clinical Significance |
|---|---|---|
| Location | Epigastric, may radiate to back | Suggests pancreatic origin |
| Quality | Knife-like, boring, constant | Distinguishes from other conditions |
| Intensity | Severe (7-10/10 pain scale) | Indicates inflammatory severity |
| Aggravating factors | Eating, lying supine | Helps confirm diagnosis |
| Relieving factors | Leaning forward, fetal position | Characteristic positioning |
Physical Assessment Findings
🔍 Cullen’s Sign
Bluish discoloration around umbilicus indicating retroperitoneal bleeding in severe pancreatitis
🔍 Grey Turner’s Sign
Bluish-gray discoloration of flanks suggesting retroperitoneal hemorrhage
🔍 Abdominal Rigidity
Board-like abdomen due to peritoneal irritation and guarding
🔍 Diminished Bowel Sounds
Paralytic ileus secondary to inflammatory process
Systemic Manifestations
Cardiovascular Signs
- Tachycardia and hypotension due to fluid loss
- Shock in severe cases from third-spacing
- Pleural effusions from inflammatory mediators
Respiratory Signs
- Tachypnea and shallow breathing
- Adult respiratory distress syndrome (ARDS) in severe cases
- Decreased oxygen saturation
Metabolic Signs
- Hyperglycemia from beta cell damage
- Hypocalcemia from fat saponification
- Hypomagnesemia and hypoalbuminemia
🧪 Diagnostic Tests
Laboratory Studies
| Test | Normal Range | Pancreatitis Finding | Clinical Significance |
|---|---|---|---|
| Serum Amylase | 30-110 U/L | >3x upper limit | Early marker, peaks in 24 hours |
| Serum Lipase | 10-140 U/L | >3x upper limit | More specific, remains elevated longer |
| C-Reactive Protein | <3 mg/L | >150 mg/L | Severity predictor at 48 hours |
| White Blood Count | 4,000-11,000/μL | 12,000-20,000/μL | Indicates inflammatory response |
| Serum Calcium | 8.5-10.5 mg/dL | <8.0 mg/dL | Poor prognostic indicator |
Lipase vs. Amylase
Lipase is more specific for pancreatitis and remains elevated longer than amylase. Lipase elevation persists for 8-14 days while amylase normalizes within 3-5 days, making lipase more useful for delayed presentations.
Imaging Studies
🔹 CT Scan
Gold standard for assessing severity, complications, and guiding intervention in pancreatitis
🔹 Ultrasound
First-line imaging for gallstone detection, may show pancreatic enlargement
🔹 MRCP
Magnetic resonance cholangiopancreatography for ductal anatomy visualization
🔹 ERCP
Endoscopic procedure for therapeutic intervention and detailed ductal imaging
Severity Assessment Scores
🧠 RANSON’S CRITERIA (At Admission)
≥3 criteria indicates severe pancreatitis with increased mortality risk
👩⚕️ Nursing Assessment
Primary Assessment Priorities
🚨 IMMEDIATE PRIORITIES
- Assess airway, breathing, circulation (ABC)
- Evaluate pain level using 0-10 scale
- Monitor vital signs and hemodynamic status
- Assess for signs of shock or organ failure
Comprehensive Assessment Framework
🔍 Pain Assessment
Pain is the most prominent symptom in pancreatitis and requires thorough evaluation:
| Assessment Component | Key Questions | Documentation Points |
|---|---|---|
| Onset | When did pain start? How quickly? | Sudden vs. gradual onset |
| Location | Where is the pain? Does it move? | Epigastric with back radiation |
| Quality | How would you describe the pain? | Boring, knife-like, constant |
| Severity | Rate pain 0-10 scale | Usually 7-10/10 intensity |
| Aggravating factors | What makes it worse? | Eating, supine position |
| Relieving factors | What helps the pain? | Leaning forward, knee-chest position |
🫀 Cardiovascular Assessment
Critical Monitoring Points
- Blood Pressure: Monitor for hypotension indicating fluid loss
- Heart Rate: Tachycardia >100 bpm suggests dehydration
- Capillary Refill: >3 seconds indicates poor perfusion
- Urine Output: <0.5 mL/kg/hr suggests renal compromise
🫁 Respiratory Assessment
Respiratory complications are common in severe pancreatitis:
- Monitor respiratory rate and depth
- Assess oxygen saturation continuously
- Auscultate for decreased breath sounds
- Watch for signs of respiratory distress
🤢 Gastrointestinal Assessment
Nausea/Vomiting
Assess frequency, volume, and characteristics of emesis
Bowel Sounds
Often diminished or absent due to ileus
Abdominal Distension
Monitor for increasing girth and rigidity
Bowel Movement Pattern
Note steatorrhea in chronic cases
Psychosocial Assessment
Assess patient and family understanding of pancreatitis, coping mechanisms, and support systems. Evaluate for alcohol use history and readiness for lifestyle changes.
⚕️ Nursing Interventions
Priority Nursing Diagnoses
🔥 PRIORITY #1: Acute Pain
Related to: Pancreatic inflammation and enzyme autodigestion
Evidence: Patient reports severe epigastric pain 8/10, guarding, restlessness
Interventions:
- Administer prescribed analgesics (avoid morphine – may cause sphincter of Oddi spasm)
- Position patient in knee-chest or leaning forward position
- Apply heat/cold as ordered and tolerated
- Teach relaxation and breathing techniques
- Monitor pain level every 2-4 hours using standard pain scale
💧 PRIORITY #2: Deficient Fluid Volume
Related to: Third-spacing, vomiting, and decreased oral intake
Evidence: Hypotension, tachycardia, decreased urine output, poor skin turgor
Interventions:
- Monitor vital signs every 2-4 hours
- Maintain accurate intake and output records
- Administer IV fluids as prescribed (often 250-500 mL/hr initially)
- Monitor electrolyte levels and replace as needed
- Weigh patient daily at same time
Comprehensive Care Interventions
🍽️ Nutritional Management
NPO (Nothing by Mouth) Protocol
- Maintain NPO status during acute phase to rest pancreas
- Insert nasogastric tube if persistent vomiting
- Provide mouth care every 2-4 hours
- Monitor for return of bowel sounds
Nutritional Reintroduction
When resuming feeding in pancreatitis patients:
- Start with clear liquids when pain subsides
- Progress to low-fat, small frequent meals
- Avoid alcohol, caffeine, and spicy foods
- Monitor for pain recurrence with feeding
- Collaborate with dietitian for meal planning
🩺 Monitoring and Prevention
| System | Monitoring Parameters | Frequency | Action Thresholds |
|---|---|---|---|
| Cardiovascular | BP, HR, CVP, urine output | Every 2-4 hours | SBP <90, HR >120, UO <0.5 mL/kg/hr |
| Respiratory | RR, O2 sat, breath sounds | Every 4 hours | RR >24, O2 sat <92% |
| Neurological | LOC, orientation | Every 8 hours | Decreased consciousness |
| Laboratory | Enzymes, electrolytes, CBC | Daily or PRN | Ca <8.0, glucose >250 |
🛡️ Complication Prevention
Infection Prevention
- Monitor temperature every 4 hours
- Maintain aseptic technique for all procedures
- Assess for signs of systemic infection
- Administer antibiotics as prescribed
Skin Integrity
- Reposition every 2 hours if on bed rest
- Use pressure-relieving devices
- Keep skin clean and dry
- Monitor pressure points
💊 Pharmacological Management
Pain Management
🔹 Meperidine (Pethidine)
Dose: 25-100 mg IM/IV every 3-4 hours
Rationale: Preferred over morphine as it causes less sphincter of Oddi spasm
Nursing Considerations: Monitor for respiratory depression, assess pain relief, avoid in renal impairment
🔹 Fentanyl
Dose: 25-100 mcg IV every 1-2 hours PRN
Rationale: Potent opioid with minimal effect on pancreatic sphincter
Nursing Considerations: Short duration, monitor respiratory status, titrate carefully
⚠️ Avoid Morphine
Morphine can cause spasm of the sphincter of Oddi, potentially worsening pancreatitis by increasing pancreatic duct pressure. Use alternative opioids when possible.
Supportive Medications
| Medication Class | Example | Purpose | Nursing Implications |
|---|---|---|---|
| Antiemetics | Ondansetron 4-8 mg IV | Control nausea/vomiting | Monitor for constipation |
| Proton Pump Inhibitors | Pantoprazole 40 mg IV | Reduce gastric acid | Give before meals if feeding |
| Enzyme Supplements | Pancrelipase with meals | Replace deficient enzymes | Give with first bite of food |
| Insulin | Regular insulin sliding scale | Control hyperglycemia | Monitor blood glucose closely |
Chronic Pancreatitis Management
🔹 Pancreatic Enzyme Replacement Therapy (PERT)
Examples: Creon, Zenpep, Pancreaze
Dosing: 25,000-50,000 units lipase with meals
Administration: Take with first bite of food, do not crush enteric-coated capsules
Patient Education: Essential for preventing malabsorption in chronic pancreatitis
Medication Safety Considerations
Drug Interactions and Contraindications
- Alcohol: Strictly contraindicated – can worsen pancreatitis
- Tetracycline: Avoid with pancreatic enzymes – reduces effectiveness
- Antacids: May inactivate pancreatic enzymes if taken simultaneously
- Warfarin: Monitor INR closely as pancreatic enzymes may affect absorption
⚠️ Complications
Local Complications
🔴 Pancreatic Necrosis
Tissue death requiring surgical debridement, high mortality risk
🔴 Pancreatic Abscess
Infected necrotic tissue, requires drainage and antibiotics
🟡 Pseudocyst Formation
Fluid collection that may compress surrounding structures
🟡 Biliary Obstruction
Compression of common bile duct causing jaundice
Systemic Complications
🫁 Respiratory Complications
Adult Respiratory Distress Syndrome (ARDS)
Severe pancreatitis can trigger ARDS through inflammatory mediator release:
- Pathophysiology: Increased pulmonary capillary permeability
- Signs: Severe hypoxemia, bilateral infiltrates on chest X-ray
- Management: Mechanical ventilation, PEEP, prone positioning
- Nursing Care: Frequent respiratory assessments, positioning, sedation management
🫀 Cardiovascular Complications
- Hypovolemic Shock: From third-spacing and fluid loss
- Distributive Shock: From systemic inflammatory response
- Cardiac Arrhythmias: Secondary to electrolyte imbalances
- Pericardial Effusion: Rare but serious complication
🧠 Metabolic Complications
| Complication | Mechanism | Clinical Signs | Management |
|---|---|---|---|
| Diabetes Mellitus | Beta cell destruction | Hyperglycemia, polyuria | Insulin therapy, glucose monitoring |
| Hypocalcemia | Fat saponification | Tetany, positive Chvostek’s sign | Calcium replacement |
| Hypomagnesemia | Malabsorption | Muscle weakness, seizures | Magnesium supplementation |
| Disseminated Intravascular Coagulation | Systemic inflammation | Bleeding, thrombosis | Supportive care, hematology consult |
🚨 Red Flag Complications
Immediate physician notification required for: persistent hypotension, respiratory distress, altered mental status, signs of bleeding, temperature >101.5°F, or worsening abdominal pain in pancreatitis patients.
📚 Patient Education
Acute Phase Education
🏥 During Hospitalization
- Explain the nature of pancreatitis and treatment plan
- Discuss the importance of NPO status and IV fluid therapy
- Teach pain management techniques and positioning
- Provide realistic expectations about recovery timeline
- Address family concerns and questions
Discharge Education
🍽️ Dietary Modifications
Key Dietary Guidelines for Pancreatitis Recovery
- Low-fat diet: <30 grams of fat per day initially
- Small frequent meals: 5-6 small meals instead of 3 large ones
- Avoid alcohol completely: Even small amounts can trigger recurrence
- Stay hydrated: 8-10 glasses of water daily
- Avoid fried foods: Opt for baked, grilled, or steamed preparations
🚫 Alcohol Cessation
Alcohol cessation is crucial for preventing recurrent pancreatitis:
- Provide resources for alcohol cessation programs
- Discuss the direct relationship between alcohol and pancreatic damage
- Refer to addiction counselors or support groups as needed
- Emphasize that even moderate drinking can cause recurrence
Chronic Pancreatitis Education
💊 Enzyme Replacement Therapy Education
Timing: Take with the first bite of each meal or snack
Dosage: Adjust based on meal size and fat content
Storage: Keep in cool, dry place, do not refrigerate
Signs of inadequacy: Steatorrhea, weight loss, abdominal cramping
🩺 Monitoring and Follow-up
| Monitoring Area | Frequency | What to Watch For | When to Call Provider |
|---|---|---|---|
| Pain Level | Daily | Increasing severity | Pain >6/10 or uncontrolled |
| Blood Sugar | As directed | Hyperglycemia symptoms | Blood glucose >250 mg/dL |
| Weight | Weekly | Unintentional weight loss | Loss >5 pounds in 1 week |
| Stool Changes | Daily | Oily, floating stools | Persistent steatorrhea |
🧠 PATIENT EDUCATION MNEMONIC: PANCREAS
🌍 Global Best Practices
International Guidelines and Standards
🇺🇸 American College of Gastroenterology (ACG) Guidelines
The ACG emphasizes early aggressive fluid resuscitation within the first 12-24 hours for acute pancreatitis management, recommending lactated Ringer’s solution over normal saline to reduce systemic inflammatory response.
🇪🇺 European Society of Gastrointestinal Endoscopy (ESGE)
European protocols focus on minimally invasive approaches, including endoscopic necrosectomy for infected pancreatic necrosis, showing improved outcomes compared to traditional surgical approaches.
🇯🇵 Japanese Society of Gastroenterology Approach
Innovative Japanese Protocols
- Early enteral nutrition: Starting within 48-72 hours when possible
- Probiotic therapy: Use of specific probiotic strains to prevent complications
- Continuous regional arterial infusion: For severe necrotizing pancreatitis
- Multidisciplinary team approach: Integration of gastroenterology, surgery, and critical care
Evidence-Based Innovations
🔬 Netherlands Protocol: Step-Up Approach
Dutch medical centers pioneered the step-up approach for necrotizing pancreatitis:
- Conservative management with antibiotics
- Percutaneous catheter drainage if needed
- Minimally invasive necrosectomy as final step
This approach has reduced mortality rates by 30% compared to immediate surgical intervention.
🇨🇦 Canadian Critical Care Protocols
Enhanced Recovery After Surgery (ERAS) for Pancreatitis
- Multimodal pain management reducing opioid dependence
- Early mobilization protocols within 24-48 hours
- Goal-directed fluid therapy based on dynamic parameters
- Nutritional optimization with immunonutrition supplements
Technology Integration
📱 Digital Health Monitoring
Several countries have implemented digital solutions for pancreatitis management:
- Sweden: Mobile apps for enzyme replacement therapy adherence tracking
- South Korea: AI-powered CT scan analysis for severity assessment
- Australia: Telemedicine follow-up programs for rural patients
- Germany: Electronic health records integration for coordinated care
🧬 Precision Medicine Approaches
Genetic Testing and Personalized Treatment
Leading medical centers in the United States and Europe now utilize genetic testing for hereditary pancreatitis to provide personalized treatment plans and family counseling, improving outcomes through early intervention strategies.
Quality Improvement Initiatives
🏥 Hospital Protocol Standardization
Top-performing hospitals worldwide have implemented standardized protocols resulting in:
| Quality Metric | Global Benchmark | Best Practice Strategy | Outcome Improvement |
|---|---|---|---|
| Length of Stay | 4-6 days mild cases | Early mobilization, standardized nutrition | 25% reduction |
| Readmission Rate | <10% within 30 days | Comprehensive discharge planning | 40% reduction |
| Mortality Rate | <5% mild-moderate cases | Early recognition, aggressive resuscitation | 50% reduction |
| Patient Satisfaction | >90% satisfaction scores | Patient education, pain management | 20% improvement |
🌟 Key Takeaways for Nursing Practice
Implementing these global best practices in pancreatitis care includes early aggressive fluid resuscitation, multidisciplinary team collaboration, patient-centered education, and continuous quality improvement monitoring to achieve optimal patient outcomes.
