Encephalitis
Comprehensive Nursing Notes
Contents
Definition
Encephalitis is an inflammation of the brain parenchyma typically caused by infection or autoimmune processes. The term derives from the Greek “enkephalos” (brain) and the suffix “-itis” (inflammation).
Clinical Pearl
While both encephalitis and meningitis involve CNS inflammation, encephalitis affects the brain parenchyma, whereas meningitis involves the meninges (the protective membranes covering the brain and spinal cord). Meningoencephalitis refers to inflammation of both the brain and the meninges.
Epidemiology
- The global incidence of encephalitis is estimated at 5-10 cases per 100,000 population annually
- Higher incidence in infants, young children, and individuals over 65 years of age
- Herpes simplex encephalitis (HSE) is the most common cause of sporadic viral encephalitis in the Western world
- Seasonal variations are observed with certain types:
- Arboviral encephalitis (like West Nile, Japanese encephalitis) more common in summer and fall
- Enteroviral encephalitis more common in summer and early autumn
- Geographic variations:
- Japanese encephalitis is endemic in parts of Asia and the Pacific
- Tick-borne encephalitis in parts of Europe and Asia
- Eastern equine encephalitis in eastern United States
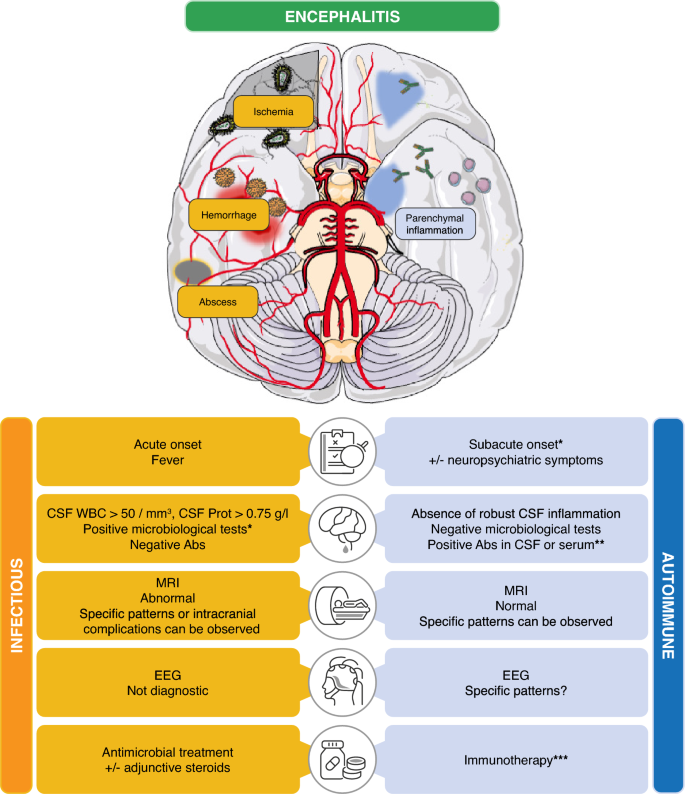
Fig 1: Global distribution of different encephalitis etiologies
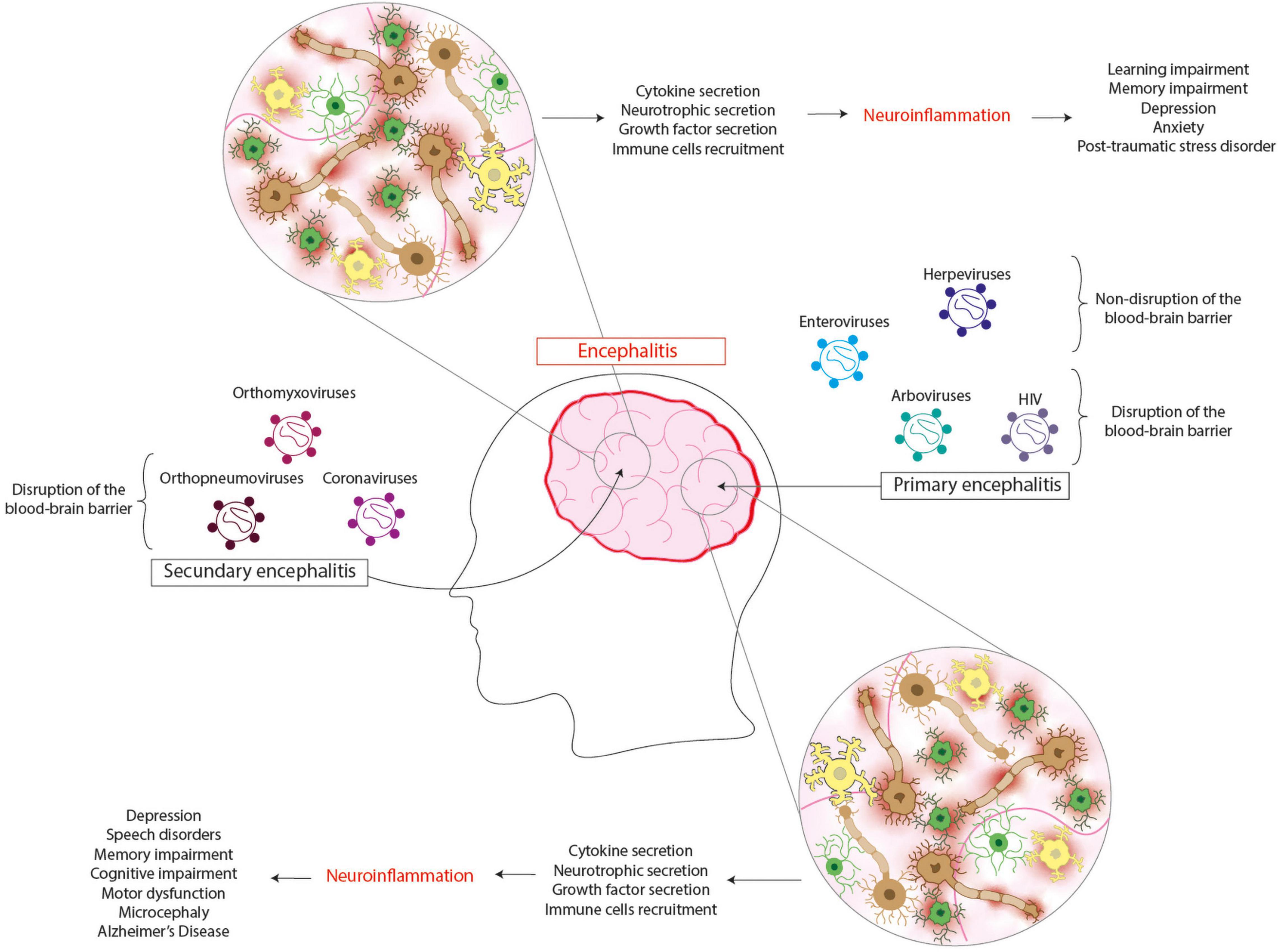
Pathophysiology
Encephalitis involves inflammation of the brain parenchyma, which can occur through several mechanisms:

Fig 2: Overview of pathophysiological mechanisms in encephalitis
Primary Mechanisms
1. Direct Invasion
- Pathogens (typically viruses) enter the central nervous system (CNS)
- Entry routes include:
- Hematogenous spread: Pathogen crosses the blood-brain barrier (BBB)
- Neural pathway: Retrograde axonal transport (e.g., HSV, rabies virus)
- Olfactory route: Via olfactory neurons (rare)
- Once inside, pathogens replicate within neurons and glial cells, causing cell injury and death
2. Immune-Mediated Processes
- Post-infectious encephalitis: Immune response against CNS components following infection elsewhere
- Autoimmune encephalitis: Antibodies target neuronal antigens (e.g., anti-NMDA receptor encephalitis)
- Release of pro-inflammatory cytokines exacerbates inflammation and BBB disruption
3. Pathological Changes
- Inflammatory infiltrates (predominantly lymphocytes)
- Microglial nodules and perivascular cuffing
- Neuronal degeneration and necrosis
- Cerebral edema (cytotoxic and vasogenic)
- Increased intracranial pressure
Clinical Pearl
Herpes simplex encephalitis typically affects the temporal lobes, insular cortex, and orbitofrontal regions, explaining its characteristic presentation with personality changes, memory impairment, and seizures.
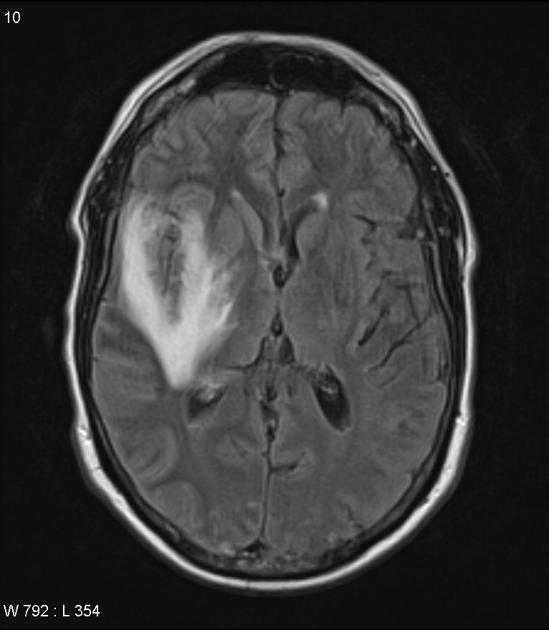
Fig 3: MRI showing typical temporal lobe involvement in Herpes Simplex Encephalitis
Etiology
Encephalitis can be classified into two main categories based on its cause:
1. Infectious Encephalitis
| Category | Examples | Clinical Features |
|---|---|---|
| Herpes Viruses |
|
HSV: Temporal lobe involvement, fever, altered mental status, focal neurological deficits VZV: Often follows chickenpox or shingles, cerebellar ataxia common |
| Arboviruses |
|
Seasonal pattern, geographical distribution varies, vector-borne (mosquitoes or ticks), often with prodromal flu-like symptoms |
| Enteroviruses |
|
Summer-fall seasonality, GI or respiratory prodrome, potentially severe in neonates and immunocompromised |
| Other Viruses |
|
Rabies: Nearly always fatal, hydrophobia, aerophobia Measles: Delayed progressive encephalitis (SSPE) |
| Bacteria |
|
Often as complication of meningitis or cerebral abscess, may present as meningoencephalitis |
| Fungi & Parasites |
|
More common in immunocompromised patients, may have indolent course |
2. Autoimmune Encephalitis
| Category | Examples | Clinical Features |
|---|---|---|
| Cell-surface/Synaptic Antibodies |
|
Anti-NMDA: Psychiatric symptoms, dyskinesias, autonomic instability, language dysfunction Anti-LGI1: Faciobrachial dystonic seizures, hyponatremia |
| Intracellular Antibodies |
|
Often paraneoplastic (associated with cancer), worse prognosis than cell-surface antibody encephalitis |
| Post-infectious |
|
Occurs 1-2 weeks after viral illness or vaccination, widespread demyelination, more common in children |
VIRAL BRAIN Mnemonic for Causes of Encephalitis
Clinical Presentation
The clinical presentation of encephalitis can vary widely, from mild symptoms to severe, life-threatening manifestations. The onset may be acute or subacute.
Common Symptoms
General Symptoms
- Fever (often high-grade)
- Headache (typically severe)
- Nausea and vomiting
- Fatigue/malaise
- Photophobia and phonophobia
Neurological Symptoms
- Altered mental status/consciousness
- Confusion or disorientation
- Seizures (focal or generalized)
- Personality changes
- Memory impairment
- Speech/language disturbances
Focal Neurological Signs
- Motor weakness or paralysis
- Abnormal reflexes
- Cranial nerve deficits
- Ataxia or coordination problems
- Visual field defects
- Sensory impairment
Warning Signs Requiring Immediate Intervention
- Decreased level of consciousness (Glasgow Coma Scale < 8)
- Status epilepticus
- Signs of increased intracranial pressure (bradycardia, hypertension, irregular breathing)
- Respiratory compromise
- Bulging fontanelles in infants
Presentation by Specific Etiology
| Type | Characteristic Features | Special Considerations |
|---|---|---|
| HSV Encephalitis |
|
Rapid progression; untreated mortality >70% |
| Japanese Encephalitis |
|
Most common epidemic encephalitis globally |
| West Nile Encephalitis |
|
More severe in elderly and immunocompromised |
| Anti-NMDA Receptor Encephalitis |
|
Often young women; check for ovarian teratoma |
| Rabies Encephalitis |
|
Nearly 100% fatal once symptoms begin |
| Acute Disseminated Encephalomyelitis (ADEM) |
|
More common in children; typically monophasic |
Clinical Pearl
The triad of fever, headache, and altered mental status should always prompt consideration of encephalitis, especially when accompanied by focal neurological signs. In elderly patients, altered mental status may be the predominant or only symptom.
Diagnosis
Diagnosing encephalitis requires a systematic approach, as early identification and treatment significantly improve outcomes. The diagnostic workup includes clinical assessment, laboratory tests, imaging studies, and sometimes brain biopsy.
Diagnostic Approach
Initial Clinical Assessment
- Thorough history, including:
- Recent travel history
- Animal exposures
- Insect bites
- Recent infections
- Vaccination status
- Immune status
- Occupational exposures
- Comprehensive neurological examination
- Assessment of vital signs and level of consciousness
Laboratory Tests
| Test | Findings | Significance |
|---|---|---|
| Blood Tests |
|
Leukocytosis suggests infection Electrolyte abnormalities may indicate SIADH (common in encephalitis) Rule out other conditions |
| Cerebrospinal Fluid (CSF) Analysis |
|
Typical findings: Lymphocytic pleocytosis (10-1000 cells/mm³) Mildly elevated protein (50-200 mg/dL) Normal glucose HSV PCR has 98% sensitivity and specificity |
| Serology |
|
IgM indicates recent infection Paired acute and convalescent samples may show rising titers |
Imaging Studies
| Modality | Findings | Utility |
|---|---|---|
| Magnetic Resonance Imaging (MRI) |
|
Preferred imaging modality High sensitivity for early changes Can suggest specific etiologies |
| Computed Tomography (CT) |
|
Less sensitive than MRI Useful for initial screening To rule out contraindications for lumbar puncture |
Other Diagnostic Tests
- Electroencephalography (EEG):
- Generalized slowing (common)
- Periodic lateralized epileptiform discharges (PLEDs) in HSV encephalitis
- Subclinical seizures may be detected
- Extreme delta brush pattern in anti-NMDA receptor encephalitis
- Brain Biopsy:
- Reserved for cases where diagnosis remains unclear
- Can identify inflammatory changes and specific pathogens
- Considered when empiric therapy fails

Fig 4: MRI (T2-weighted) showing hyperintensity in the right temporal lobe characteristic of HSV encephalitis
ENCEPHALITIS Mnemonic for Diagnostic Approach
Clinical Pearl
When encephalitis is suspected, do not delay empiric antiviral therapy while waiting for diagnostic confirmation. In HSV encephalitis, treatment delay beyond 24 hours significantly increases morbidity and mortality.
Treatment
Treatment of encephalitis focuses on addressing the underlying cause, managing symptoms, and preventing complications. Early intervention is crucial for improved outcomes.
Treatment Approaches
1. Antimicrobial Therapy
| Agent | Indication | Dosage and Administration | Nursing Considerations |
|---|---|---|---|
| Acyclovir | HSV and VZV encephalitis (also given empirically) | 10-15 mg/kg IV every 8 hours for 14-21 days |
|
| Ganciclovir | CMV encephalitis | 5 mg/kg IV every 12 hours for 14-21 days |
|
| Antibiotics | Bacterial encephalitis/meningoencephalitis | Based on suspected pathogen, typically broad-spectrum initially |
|
| Amphotericin B | Fungal encephalitis | 0.7-1.0 mg/kg/day IV |
|
2. Immunomodulatory Therapy
| Agent | Indication | Administration | Nursing Considerations |
|---|---|---|---|
| Corticosteroids |
|
Methylprednisolone 1g IV daily for 3-5 days |
|
| Intravenous Immunoglobulin (IVIG) | Autoimmune encephalitis | 2g/kg divided over 2-5 days |
|
| Plasma Exchange | Severe autoimmune encephalitis | 5-7 exchanges over 10-14 days |
|
| Rituximab | Refractory autoimmune encephalitis | 375 mg/m² weekly for 4 weeks |
|
3. Supportive Care
- Airway management: Intubation may be necessary for decreased consciousness
- Seizure management:
- Benzodiazepines for acute seizures
- Antiepileptic drugs (levetiracetam, phenytoin) for seizure prophylaxis
- EEG monitoring for subclinical seizures
- Managing increased intracranial pressure (ICP):
- Head elevation (30°)
- Osmotic diuretics (mannitol, hypertonic saline)
- Avoiding hypercapnia
- ICP monitoring in severe cases
- Fluid and electrolyte management:
- Monitor for SIADH (Syndrome of Inappropriate Antidiuretic Hormone)
- Fluid restriction if hyponatremia present
- Regular electrolyte monitoring
- Nutrition support: Early enteral nutrition if prolonged altered consciousness
- DVT prophylaxis for immobilized patients
- Fever management with antipyretics
Treatment Algorithm
- Initial stabilization: Secure airway, breathing, and circulation
- Empiric therapy: Start acyclovir immediately if encephalitis is suspected
- Diagnostic tests: Perform LP, blood tests, and imaging while starting treatment
- Etiology-specific treatment: Adjust therapy based on identified cause
- Supportive care: Manage complications (seizures, increased ICP, etc.)
- Rehabilitation: Early initiation of physical, occupational, and speech therapy
Clinical Pearl
For suspected HSV encephalitis, initiate acyclovir before confirmatory test results are available. If HSV PCR is negative after 24-72 hours and an alternative diagnosis becomes apparent, acyclovir can be discontinued.
Nursing Care
Nursing care for patients with encephalitis is multifaceted and requires a comprehensive approach. Key nursing interventions focus on neurological assessment, supportive care, and prevention of complications.
Nursing Care Plan for Encephalitis
Nursing Diagnosis 1: Risk for Ineffective Cerebral Tissue Perfusion related to cerebral edema and inflammation
Assessment:
- Monitor vital signs, especially blood pressure and heart rate
- Perform neurological assessments q2-4h or as indicated
- Monitor Glasgow Coma Scale (GCS)
- Assess pupillary responses, motor function, and sensory function
- Monitor for signs of increased intracranial pressure
- Monitor oxygen saturation and respiratory status
Interventions:
- Position patient with head of bed elevated 30° (unless contraindicated)
- Maintain head and neck in neutral alignment
- Administer prescribed medications (osmotic diuretics, corticosteroids) as ordered
- Monitor fluid balance and avoid fluid overload
- Maintain normothermia; implement cooling measures for hyperthermia
- Avoid activities that increase ICP (Valsalva maneuver, excessive stimulation)
- Maintain adequate oxygenation
Expected Outcomes:
- Patient will maintain cerebral perfusion as evidenced by stable or improved neurological status
- ICP will remain within normal limits
- Patient will not demonstrate signs of neurological deterioration
Nursing Diagnosis 2: Risk for Injury related to seizure activity
Assessment:
- Monitor for clinical seizure activity
- Review EEG reports for subclinical seizures
- Monitor effectiveness of anticonvulsant therapy
- Monitor drug levels of anticonvulsants
Interventions:
- Maintain seizure precautions (padded side rails, oral airway at bedside)
- Administer anticonvulsant medications as prescribed
- During seizure: ensure patient safety, protect airway, position in lateral position if possible
- Document seizure characteristics (duration, type, associated behaviors)
- Maintain a quiet, non-stimulating environment
- Educate family about seizure management
Expected Outcomes:
- Patient will remain free from injury during seizure activity
- Seizures will be controlled with appropriate medication
- Patient/family will demonstrate understanding of seizure precautions
Nursing Diagnosis 3: Hyperthermia related to inflammatory process
Assessment:
- Monitor body temperature q2-4h or continuously if indicated
- Assess for signs of dehydration
- Monitor for shivering during cooling measures
Interventions:
- Administer antipyretics as prescribed
- Implement cooling measures (cooling blanket, tepid sponge bath)
- Ensure adequate hydration
- Provide light clothing and bedding
- Monitor effectiveness of interventions
Expected Outcomes:
- Patient will maintain normothermia (T ≤ 37.5°C)
- Patient will not experience complications related to hyperthermia
Nursing Diagnosis 4: Impaired Verbal Communication related to cerebral inflammation
Assessment:
- Assess speech pattern, comprehension, and ability to express needs
- Evaluate effectiveness of current communication methods
- Determine best method of communication for the patient
Interventions:
- Establish alternative communication methods (picture boards, writing, gestures)
- Speak slowly and clearly, using simple language
- Allow adequate time for patient response
- Minimize environmental distractions during communication
- Involve speech therapy early in care
- Educate family on effective communication techniques
Expected Outcomes:
- Patient will demonstrate ability to communicate basic needs
- Patient will show decreased frustration with communication
- Effective communication method will be established
Nursing Diagnosis 5: Risk for Impaired Skin Integrity related to decreased mobility and altered mental status
Assessment:
- Perform regular skin assessments
- Identify risk factors (immobility, incontinence, nutritional status)
- Use validated pressure ulcer risk assessment tool (e.g., Braden Scale)
Interventions:
- Implement turning schedule (q2h) if patient is immobile
- Use pressure-relieving devices (specialized mattress, heel protectors)
- Keep skin clean and dry
- Provide meticulous perineal care for incontinent patients
- Ensure adequate nutrition and hydration
- Initiate early mobilization when appropriate
- Perform passive range of motion exercises
Expected Outcomes:
- Patient will maintain skin integrity
- No evidence of pressure injuries will develop
- Any existing skin issues will show improvement
Additional Nursing Considerations
Observation and Monitoring
- Implement neurological checks q1-2h initially, then as indicated
- Monitor for signs of increasing ICP: decreased LOC, pupillary changes, Cushing’s triad
- Assess for adverse medication effects
- Monitor I/O and daily weights
- Observe for signs of immunosuppression if on corticosteroids
- Monitor electrolytes, especially sodium (risk of SIADH)
Patient and Family Support
- Provide emotional support and reassurance
- Educate about the disease process, treatments, and expected course
- Prepare family for potential personality/behavioral changes
- Involve social services early in care planning
- Provide resources for long-term support
- Assess coping mechanisms and provide appropriate resources
Infection Control
- Implement isolation precautions as indicated
- Follow standard precautions for all patients
- Practice proper hand hygiene
- Ensure proper administration of antimicrobial therapy
- Monitor for healthcare-associated infections
- Educate visitors about infection control measures
Rehabilitation Considerations
- Initiate early rehabilitation consultation
- Coordinate care with physical, occupational, and speech therapy
- Implement therapy recommendations in daily care
- Promote independence in ADLs as appropriate
- Assess need for assistive devices
- Prepare for potential transition to rehabilitation facility
NURSE CARE Mnemonic for Encephalitis Management
Complications
Encephalitis can lead to various short-term and long-term complications, which can significantly impact quality of life. The severity of complications often correlates with the causative agent, extent of brain involvement, timing of treatment, and patient’s age and comorbidities.
Potential Complications
Acute Complications
- Cerebral edema and increased ICP:
- Brain herniation
- Compression of vital structures
- Seizures:
- Status epilepticus
- Refractory seizures
- Respiratory complications:
- Respiratory failure
- Aspiration pneumonia
- Systemic complications:
- SIADH (hyponatremia)
- Autonomic instability
- Cardiac arrhythmias
- Thromboembolism:
- Deep vein thrombosis
- Pulmonary embolism
Long-term Complications
- Cognitive impairment:
- Memory deficits
- Attention and concentration problems
- Executive function impairment
- Motor deficits:
- Weakness or paralysis
- Movement disorders
- Ataxia
- Neuropsychiatric changes:
- Personality changes
- Mood disorders (depression, anxiety)
- Behavioral disturbances
- Speech and language disorders:
- Dysarthria
- Aphasia
- Epilepsy:
- 10-20% develop chronic seizures
- Other neurological sequelae:
- Visual disturbances
- Hearing impairment
- Sleep disorders
- Chronic headaches
High Mortality Risk Factors
- Delayed treatment initiation (>24 hours)
- Age extremes (very young or elderly)
- Immunocompromised status
- Low Glasgow Coma Scale (GCS < 8) at presentation
- Certain etiologies (HSV, rabies)
- Status epilepticus
- Need for mechanical ventilation
Clinical Pearl
Recovery from encephalitis often follows a biphasic pattern: initial recovery of consciousness and vital functions, followed by a more prolonged phase of cognitive and neurological improvement. Full recovery can take months to years, and some deficits may be permanent. Early intervention with comprehensive rehabilitation services is key to maximizing functional outcomes.
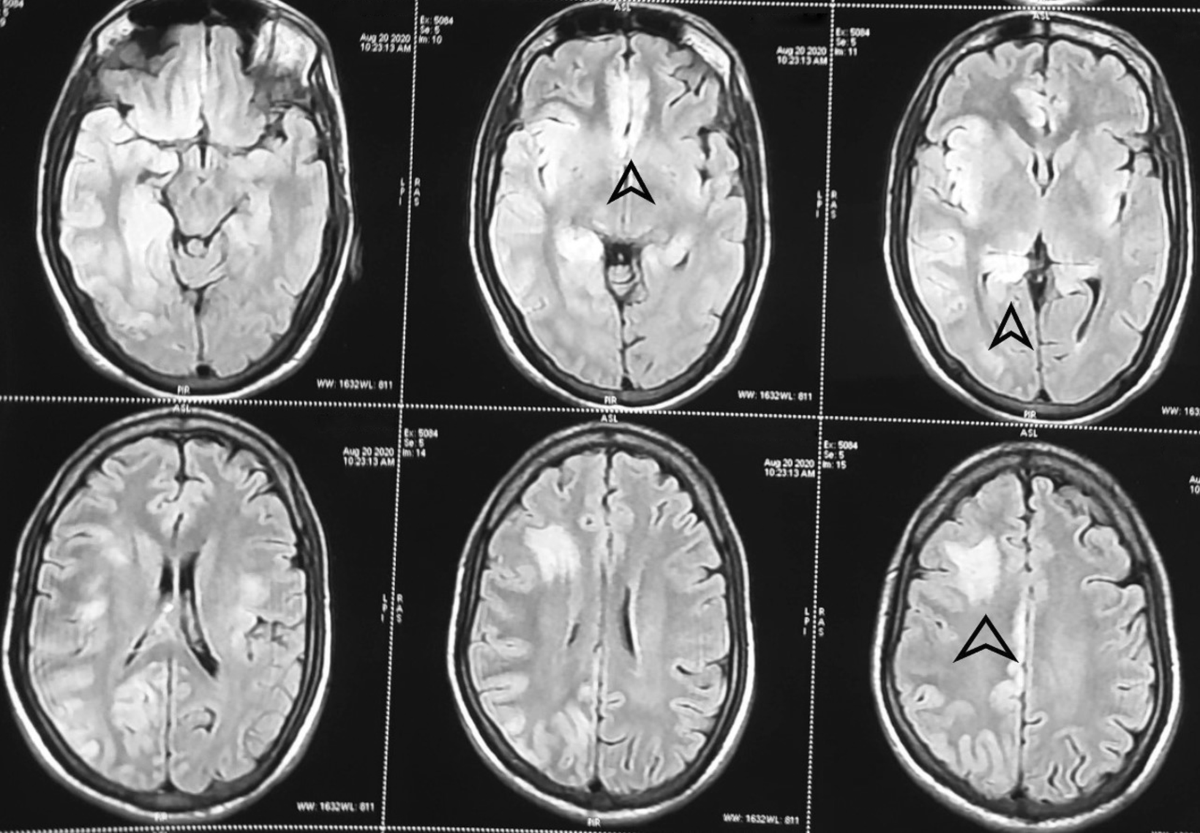
Fig 5: MRI showing long-term changes after encephalitis, with persistent signal abnormalities and atrophy in the affected regions
Prevention
Prevention strategies for encephalitis focus on reducing exposure to potential infectious agents, vaccination, and early recognition and treatment of infections that may lead to encephalitis.
Prevention Strategies
1. Vaccination
| Vaccine | Target Disease | Recommendations |
|---|---|---|
| MMR (Measles, Mumps, Rubella) | Measles encephalitis, Mumps encephalitis | Routine childhood vaccination, 2 doses |
| Japanese Encephalitis (JE) Vaccine | Japanese encephalitis | Recommended for travelers to endemic areas in Asia |
| Tick-borne Encephalitis Vaccine | Tick-borne encephalitis | Recommended for travelers to endemic areas in Europe and Asia |
| Rabies Vaccine | Rabies encephalitis | Pre-exposure for high-risk individuals; post-exposure prophylaxis after animal bites |
| Varicella Vaccine | Varicella-zoster encephalitis | Routine childhood vaccination, 2 doses |
2. Vector Control Measures
Mosquito Control
- Use insect repellents containing DEET, picaridin, or oil of lemon eucalyptus
- Wear long-sleeved shirts and long pants when outdoors
- Use permethrin-treated clothing and gear
- Stay in places with air conditioning or window and door screens
- Eliminate standing water where mosquitoes breed
- Limit outdoor activities during peak mosquito hours (dusk and dawn)
Tick Control
- Avoid wooded and brushy areas with high grass
- Walk in the center of trails
- Use repellents containing DEET or permethrin
- Conduct full-body tick checks after being outdoors
- Shower within two hours of coming indoors
- Examine gear and pets for ticks
- Remove attached ticks promptly with fine-tipped tweezers
3. Prevention of Exposure to Other Infectious Agents
- Hand hygiene: Frequent handwashing with soap and water
- Avoid close contact with people who are sick
- Food and water safety: Properly cook foods and drink safe water
- Animal contact precautions:
- Avoid direct contact with wild animals
- Vaccinate pets against rabies
- Do not handle sick or dead animals
- Safe sexual practices to prevent sexually transmitted infections that can lead to encephalitis
4. Early Recognition and Treatment
- Prompt medical attention for symptoms of infection that could progress to encephalitis
- Completion of full course of antibiotics for bacterial infections
- Antiviral treatment for herpes simplex infections
- Post-exposure prophylaxis for rabies
- Early identification and treatment of autoimmune conditions
Prevention of Encephalitis: A Comprehensive Approach
Clinical Pearl
Patient education about encephalitis prevention should be tailored to specific risk factors. For example, travelers to endemic regions should receive appropriate vaccinations and information about vector control, while immunocompromised patients should be educated about avoiding potential sources of infection and recognizing early symptoms.
Key Nursing Role in Prevention
- Educate patients and communities about vaccination schedules
- Provide information about vector-borne disease prevention
- Teach proper hand hygiene techniques
- Identify high-risk populations who may need additional preventive measures
- Advocate for vaccination and public health measures
- Participate in community surveillance for encephalitis outbreaks
