Pelvic Inflammatory Disease: Complete Nursing Study Guide
Evidence-Based Care for Women’s Health
Table of Contents
Introduction to Pelvic Inflammatory Disease
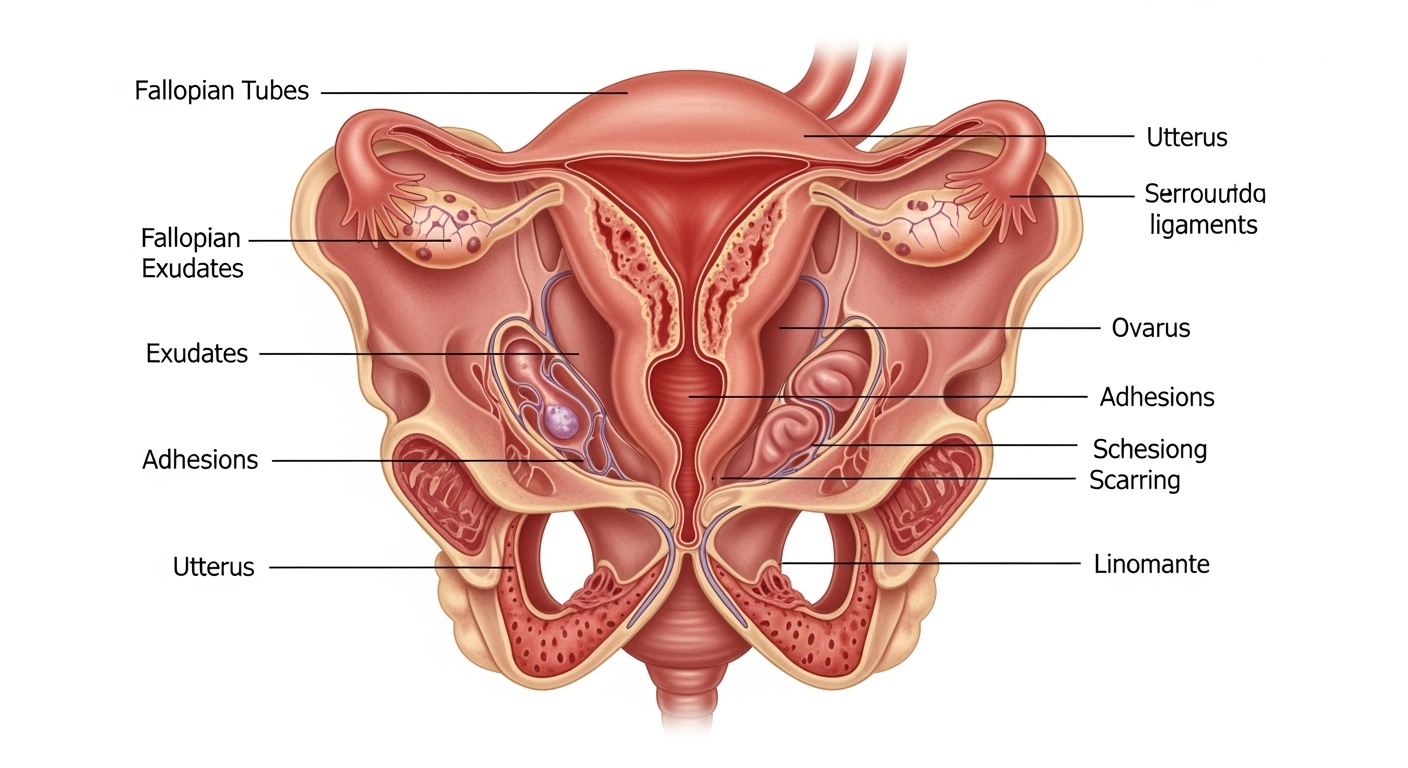
Figure 1: Anatomical representation of pelvic inflammatory disease affecting female reproductive organs
Pelvic inflammatory disease represents one of the most significant health challenges affecting women of reproductive age worldwide. This comprehensive nursing study guide provides evidence-based information essential for delivering quality patient care to women experiencing this complex condition. Understanding pelvic inflammatory disease is crucial for nursing professionals working in gynecological settings, emergency departments, and primary care environments.
Key Definition
Pelvic inflammatory disease is an infectious and inflammatory disorder of the upper female genital tract, including any combination of endometritis, salpingitis, tubo-ovarian abscess, and pelvic peritonitis. This condition primarily affects sexually active women and can result in serious reproductive health consequences if not promptly diagnosed and treated.
The significance of pelvic inflammatory disease extends beyond immediate clinical presentation, as it represents a leading cause of acquired infertility, ectopic pregnancy, and chronic pelvic pain in women. Nursing professionals play a vital role in early recognition, comprehensive assessment, patient education, and coordination of care for women affected by this condition. The multifaceted nature of pelvic inflammatory disease requires a thorough understanding of its pathophysiology, clinical manifestations, and evidence-based treatment approaches.
Contemporary research indicates that pelvic inflammatory disease affects approximately one million women annually in the United States, with healthcare costs exceeding billions of dollars. The condition disproportionately affects young women, particularly those under 25 years of age, making education and prevention strategies essential components of comprehensive nursing care.
Pathophysiology and Etiology
The pathophysiology of pelvic inflammatory disease involves ascending infection from the lower to upper genital tract. Understanding this process is fundamental for nursing professionals to provide comprehensive care and education to affected patients. The condition typically begins with cervical infection that ascends through the uterus to involve the fallopian tubes, ovaries, and surrounding pelvic structures.
Primary Causative Organisms
- Chlamydia trachomatis: Most common cause, often asymptomatic
- Neisseria gonorrhoeae: Second most common, frequently co-occurs with chlamydia
- Mycoplasma genitalium: Emerging pathogen with increasing recognition
- Bacterial vaginosis organisms: Including Gardnerella vaginalis and anaerobes
- Enteric gram-negative rods: Particularly in postpartum or post-procedural cases
The ascending infection theory explains how organisms travel from the vagina and cervix upward through the reproductive tract. Factors that facilitate this ascension include sexual activity, which can propel bacteria upward, menstruation, which provides an optimal environment for bacterial growth, and procedures that disrupt the cervical barrier. The inflammatory response triggered by these pathogens results in tissue damage, scarring, and the potential for serious long-term complications.
Infection Pathway
- 1. Initial cervical infection
- 2. Endometrial invasion
- 3. Tubal involvement (salpingitis)
- 4. Ovarian complications
- 5. Pelvic peritoneal spread
Natural Defense Mechanisms
- • Cervical mucus barrier
- • Vaginal pH maintenance
- • Normal bacterial flora
- • Immune system response
- • Tubal ciliary action
The inflammatory cascade initiated by pelvic inflammatory disease involves complex interactions between pathogenic organisms and host immune responses. Cytokine release, neutrophil infiltration, and tissue destruction characterize the acute phase, while chronic inflammation can lead to fibrosis, adhesion formation, and structural damage that may persist long after the initial infection resolves.
Clinical Manifestations
Clinical presentation of pelvic inflammatory disease varies significantly among patients, ranging from subtle symptoms to acute, severe manifestations. Nursing professionals must maintain high clinical suspicion, as many women with pelvic inflammatory disease may present with nonspecific symptoms or remain asymptomatic until complications develop. Early recognition and assessment are critical for preventing long-term reproductive consequences.
| Symptom Category | Common Manifestations | Frequency | Nursing Considerations |
|---|---|---|---|
| Pelvic Pain | Lower abdominal pain, bilateral adnexal tenderness, dyspareunia, pain with movement | 95-100% | Assess pain intensity, character, timing, and aggravating factors |
| Vaginal Discharge | Abnormal color, odor, consistency; mucopurulent cervical discharge | 75-85% | Document characteristics, obtain specimens for culture |
| Systemic Symptoms | Fever, chills, malaise, nausea, vomiting | 30-40% | Monitor vital signs, assess for sepsis indicators |
| Urinary Symptoms | Dysuria, frequency, urgency | 20-30% | Differentiate from urinary tract infection |
| Menstrual Irregularities | Intermenstrual bleeding, heavy menstrual flow, prolonged periods | 40-60% | Obtain detailed menstrual history |
Silent Pelvic Inflammatory Disease
Up to 70% of women with pelvic inflammatory disease may have minimal or no symptoms, particularly those with chlamydial infections. This “silent” presentation poses significant challenges for healthcare providers and underscores the importance of routine screening in high-risk populations.
Nursing professionals should maintain awareness that absence of dramatic symptoms does not exclude pelvic inflammatory disease diagnosis, especially in sexually active women with risk factors.
Physical examination findings in pelvic inflammatory disease include cervical motion tenderness, uterine tenderness, and adnexal tenderness during bimanual examination. These findings, known as the “chandelier sign” when severe, represent classic indicators of upper genital tract infection. However, the sensitivity and specificity of physical examination findings vary, requiring careful integration with clinical history and laboratory results.
Severe presentations of pelvic inflammatory disease may include Fitz-Hugh-Curtis syndrome, characterized by right upper quadrant pain due to perihepatitis from pelvic infection ascension. This condition demonstrates the potential for widespread inflammatory involvement beyond the reproductive tract and requires comprehensive nursing assessment and monitoring.
Risk Factors Assessment
Comprehensive risk factor assessment is essential for nursing professionals caring for women at risk for pelvic inflammatory disease. Understanding these factors enables targeted prevention strategies, appropriate screening protocols, and early intervention approaches. Risk factors for pelvic inflammatory disease encompass behavioral, demographic, medical, and procedural elements that increase susceptibility to upper genital tract infection.
Behavioral Risk Factors
- • Multiple sexual partners
- • New sexual partner within 60 days
- • Inconsistent condom use
- • Early sexual activity initiation
- • History of sexually transmitted infections
Demographic Factors
- • Age under 25 years
- • Unmarried status
- • Lower socioeconomic status
- • Urban residence
- • African American ethnicity
Medical/Procedural
- • Previous pelvic inflammatory disease
- • Recent intrauterine device insertion
- • Endometrial biopsy
- • Douching practices
- • Recent abortion or delivery
Age represents one of the most significant risk factors for pelvic inflammatory disease, with women under 25 years accounting for approximately 75% of cases. This increased susceptibility among younger women relates to biological factors including larger cervical ectopy, behavioral patterns, and immune system immaturity. Nursing professionals should prioritize education and screening efforts for this high-risk population.
Protective Factors
Contraceptive Methods
- • Consistent condom use
- • Hormonal contraceptives
- • Barrier methods with spermicide
Lifestyle Factors
- • Monogamous relationships
- • Regular STI screening
- • Prompt treatment of infections
Sexual behavior assessment requires sensitive, nonjudgmental communication from nursing professionals. Creating an environment of trust and confidentiality encourages honest disclosure of risk factors, enabling appropriate preventive interventions and screening recommendations. The nursing assessment should include detailed sexual history, contraceptive practices, and previous infection history to identify women at increased risk for pelvic inflammatory disease.
Diagnostic Evaluation
Diagnostic evaluation of pelvic inflammatory disease presents unique challenges due to the lack of specific symptoms and definitive diagnostic tests. Nursing professionals must understand the diagnostic criteria, laboratory studies, and imaging modalities used to establish the diagnosis while recognizing the importance of clinical judgment in initiating treatment. The Centers for Disease Control and Prevention provides evidence-based diagnostic criteria that guide clinical decision-making.
CDC Diagnostic Criteria for Pelvic Inflammatory Disease
Minimum Criteria (one or more required):
- • Cervical motion tenderness
- • Uterine tenderness
- • Adnexal tenderness
Additional Criteria (supporting evidence):
- • Oral temperature greater than 101°F (38.3°C)
- • Abnormal cervical mucopurulent discharge or cervical friability
- • Presence of white blood cells on saline microscopy of vaginal fluid
- • Elevated erythrocyte sedimentation rate or C-reactive protein
- • Laboratory documentation of cervical infection with gonorrhea or chlamydia
| Diagnostic Test | Purpose | Normal Values | PID Findings |
|---|---|---|---|
| Complete Blood Count | Assess inflammatory response | WBC: 4,500-11,000/μL | Elevated WBC, left shift |
| Erythrocyte Sedimentation Rate | Measure inflammation severity | 0-20 mm/hr | Often elevated >15 mm/hr |
| C-Reactive Protein | Acute phase reactant | < 3.0 mg/L | Significantly elevated |
| Pregnancy Test | Rule out ectopic pregnancy | Negative | Must exclude pregnancy |
| NAAT Testing | Identify causative organisms | Negative | Chlamydia/gonorrhea positive |
Nucleic acid amplification testing represents the gold standard for detecting chlamydia and gonorrhea infections associated with pelvic inflammatory disease. These highly sensitive and specific tests can be performed on endocervical swabs, vaginal swabs, or urine specimens, providing flexibility in specimen collection. Nursing professionals should understand proper specimen collection techniques to ensure accurate results and guide appropriate treatment decisions.
Imaging Studies
Identifies tubo-ovarian abscesses, fluid collections, and structural abnormalities
Reserved for severe cases or suspected complications
Most sensitive for detecting subtle inflammatory changes
Specialized Tests
Gold standard for definitive diagnosis when clinical uncertainty exists
Demonstrates endometritis in research settings
Rarely performed; identifies purulent peritoneal fluid
Differential diagnosis considerations for pelvic inflammatory disease include appendicitis, ovarian cysts, ectopic pregnancy, urinary tract infections, and inflammatory bowel disease. Nursing professionals must assist with comprehensive assessment to exclude these conditions while recognizing that pelvic inflammatory disease diagnosis often relies on clinical judgment and low threshold for treatment initiation to prevent serious complications.
Comprehensive Nursing Assessment
Comprehensive nursing assessment forms the foundation of quality care for women with suspected or confirmed pelvic inflammatory disease. This systematic approach encompasses physical, psychological, and social dimensions of patient care while maintaining sensitivity to the intimate nature of reproductive health concerns. Nursing professionals must develop expertise in conducting thorough assessments that guide evidence-based interventions and promote optimal patient outcomes.
Primary Assessment Priorities
Immediate Assessment
- • Vital signs and hemodynamic stability
- • Pain intensity and characteristics
- • Signs of systemic infection or sepsis
- • Pregnancy status verification
Focused Assessment
- • Sexual and reproductive history
- • Symptom onset and progression
- • Previous infections and treatments
- • Contraceptive and barrier protection use
Communication Strategies for Sensitive Topics
Establishing Rapport
- • Use nonjudgmental language
- • Ensure privacy and confidentiality
- • Explain the importance of honest disclosure
- • Allow adequate time for discussion
- • Validate patient concerns and emotions
Assessment Techniques
- • Begin with general health questions
- • Use open-ended questions initially
- • Progress to specific sexual health topics
- • Clarify terminology and understanding
- • Document findings objectively
Pain assessment in pelvic inflammatory disease requires detailed evaluation of location, intensity, quality, timing, and associated factors. Nursing professionals should utilize standardized pain scales while recognizing that pain patterns may vary significantly among patients. Chronic pain associated with previous episodes or complications requires additional assessment of functional impact and coping strategies.
| Assessment Domain | Key Questions | Clinical Significance |
|---|---|---|
| Sexual History | Number of partners, new partners, sexual practices, protection use | Determines infection risk and transmission patterns |
| Contraceptive History | Current methods, IUD insertion timing, barrier method consistency | Influences risk factors and treatment considerations |
| Menstrual History | Last menstrual period, cycle regularity, bleeding patterns | Excludes pregnancy and identifies symptom relationships |
| Infection History | Previous STIs, PID episodes, treatment compliance, partner treatment | Identifies recurrence patterns and resistance risks |
Psychosocial assessment encompasses evaluation of emotional responses, support systems, educational needs, and barriers to care. Women with pelvic inflammatory disease may experience anxiety, shame, fear about fertility, and relationship concerns. Nursing professionals should assess these dimensions while providing emotional support and connecting patients with appropriate resources.
Cultural considerations significantly impact assessment approaches and patient responses to reproductive health questions. Nursing professionals must demonstrate cultural competence by understanding diverse perspectives on sexuality, gender roles, and healthcare decision-making while adapting assessment techniques to meet individual patient needs and preferences.
Evidence-Based Nursing Interventions
Evidence-based nursing interventions for pelvic inflammatory disease encompass comprehensive care strategies that address immediate treatment needs, symptom management, prevention of complications, and long-term health promotion. Nursing professionals play crucial roles in medication administration, patient monitoring, education delivery, and coordination of interdisciplinary care to optimize patient outcomes and prevent disease recurrence.
Medication Management
Administer prescribed antibiotics according to CDC guidelines, monitor for adverse effects, ensure medication compliance
Provide analgesics as ordered, implement non-pharmacological comfort measures, assess pain relief effectiveness
Administer NSAIDs to reduce inflammation and pain, monitor for gastrointestinal side effects
Comfort Measures
Assist with comfortable positioning, provide pelvic rest education, suggest heat therapy for pain relief
Ensure privacy, minimize noise and interruptions, maintain comfortable room temperature
Provide reassurance, validate concerns, facilitate communication with healthcare team
Antibiotic therapy represents the cornerstone of pelvic inflammatory disease treatment, requiring careful nursing oversight to ensure appropriate administration, monitoring for therapeutic response, and assessment for adverse reactions. The complex antibiotic regimens used for pelvic inflammatory disease often involve multiple medications with specific timing requirements, making patient education and compliance monitoring essential nursing responsibilities.
Critical Monitoring Parameters
Clinical Indicators
- • Temperature trends and fever patterns
- • Pain intensity and character changes
- • Vital sign stability and hemodynamic status
- • Appetite, nausea, and gastrointestinal tolerance
- • Energy levels and activity tolerance
Laboratory Values
- • White blood cell count trends
- • Inflammatory marker progression
- • Liver function with certain antibiotics
- • Renal function monitoring
- • Follow-up culture results
Patient monitoring during treatment involves systematic assessment of treatment response, early identification of complications, and prompt intervention for deteriorating conditions. Nursing professionals must recognize signs indicating need for hospitalization, including high fever, severe pain, inability to tolerate oral medications, or failure to respond to outpatient treatment within 72 hours.
Nursing Care Plan Framework
Priority Nursing Diagnoses
- • Acute pain related to pelvic inflammatory process
- • Risk for infection related to sexually transmitted pathogens
- • Anxiety related to reproductive health concerns
- • Deficient knowledge regarding disease management and prevention
Expected Outcomes
- • Patient reports pain relief within 48-72 hours of treatment initiation
- • Laboratory values demonstrate decreasing inflammatory markers
- • Patient verbalizes understanding of treatment regimen and prevention strategies
- • Patient demonstrates ability to perform self-care activities
Collaboration with interdisciplinary team members enhances comprehensive care delivery for women with pelvic inflammatory disease. Nursing professionals coordinate care with physicians, pharmacists, social workers, and reproductive health specialists to address complex patient needs and ensure continuity of care across healthcare settings. This collaborative approach optimizes treatment outcomes and supports patient-centered care delivery.
Comprehensive Patient Education
Comprehensive patient education represents a fundamental nursing intervention for women with pelvic inflammatory disease, directly impacting treatment success, complication prevention, and long-term reproductive health outcomes. Effective education addresses immediate treatment requirements, prevention strategies, partner notification, and long-term health promotion while adapting content to individual learning needs and health literacy levels.
Treatment Education Priorities
- • Complete antibiotic course importance
- • Medication timing and administration
- • Expected side effects and management
- • Signs requiring immediate medical attention
- • Follow-up appointment significance
- • Activity restrictions and pelvic rest
Prevention Education Focus
- • Safe sexual practices and barrier protection
- • Partner evaluation and treatment
- • Regular STI screening recommendations
- • Recognition of early symptoms
- • Douching avoidance education
- • Risk factor modification strategies
Medication adherence education requires detailed explanation of antibiotic importance, proper administration techniques, and completion of full treatment courses even when symptoms improve. Nursing professionals should address common barriers to adherence including cost concerns, side effect management, and complex dosing schedules while providing practical strategies to support medication compliance.
Partner Notification and Treatment
Partner notification and treatment represent critical components of pelvic inflammatory disease management, requiring sensitive nursing communication and education approaches.
Key Messages
- • All recent sexual partners require evaluation
- • Partners should be treated even if asymptomatic
- • Sexual activity should be avoided until treatment completion
- • Reinfection risks without partner treatment
Communication Support
- • Provide conversation scripts and guidance
- • Address fears about relationship disclosure
- • Offer resources for partner education
- • Discuss anonymous notification options
Long-term reproductive health education encompasses fertility awareness, contraceptive counseling, and ongoing preventive care recommendations. Women with pelvic inflammatory disease face increased risks for ectopic pregnancy, infertility, and chronic pelvic pain, making education about these potential complications and reproductive planning essential components of comprehensive nursing care.
| Education Topic | Key Teaching Points | Evaluation Methods |
|---|---|---|
| Medication Compliance | Complete entire course, timing importance, side effect management | Teach-back method, pill counting, symptom monitoring |
| Safe Sexual Practices | Condom use, partner communication, STI testing schedules | Demonstration, verbal repetition, written materials |
| Warning Signs | Fever, worsening pain, new symptoms, when to seek care | Scenario discussions, emergency contact information |
| Follow-up Care | Appointment importance, ongoing screening, reproductive planning | Calendar scheduling, appointment reminders, care planning |
Educational effectiveness requires ongoing assessment and reinforcement through multiple interactions and various teaching modalities. Nursing professionals should utilize written materials, visual aids, digital resources, and peer support programs to accommodate diverse learning preferences while ensuring patients demonstrate understanding through teach-back methods and return demonstrations of key concepts and skills.
Complications and Long-term Sequelae
Complications associated with pelvic inflammatory disease represent serious threats to women’s reproductive health and overall well-being, underscoring the critical importance of early recognition, prompt treatment, and comprehensive nursing care. Understanding these complications enables nursing professionals to provide appropriate patient education, implement preventive strategies, and recognize early indicators requiring immediate intervention.
Immediate Complications Requiring Emergency Intervention
Tubo-ovarian Abscess
- • High fever and severe pelvic pain
- • Palpable adnexal mass on examination
- • Risk for rupture and peritonitis
- • Requires hospitalization and IV antibiotics
Sepsis and Shock
- • Systemic inflammatory response syndrome
- • Hemodynamic instability
- • Altered mental status
- • Life-threatening emergency requiring ICU care
Long-term reproductive consequences of pelvic inflammatory disease include infertility, ectopic pregnancy, and chronic pelvic pain, with risk directly correlated to the number of episodes and severity of infection. Research demonstrates that even a single episode of pelvic inflammatory disease increases infertility risk by 10-15%, while multiple episodes can result in infertility rates exceeding 50%.
Infertility
Mechanism: Tubal scarring and adhesions preventing fertilization
Risk Factors: Multiple episodes, delayed treatment, severe infections
Prevention: Early treatment, partner therapy, safe sexual practices
Ectopic Pregnancy
Mechanism: Damaged tubes impair normal embryo transport
Risk Increase: 6-10 fold higher than general population
Recognition: Abdominal pain, bleeding, positive pregnancy test
Chronic Pelvic Pain
Prevalence: Affects 20% of women with PID history
Impact: Significantly affects quality of life and function
Management: Multidisciplinary approach including pain specialists
Nursing assessment for complications involves systematic monitoring of treatment response, early recognition of deteriorating conditions, and prompt communication with healthcare providers. Signs indicating potential complications include persistent or worsening fever after 72 hours of treatment, increasing pain intensity, development of new symptoms, or hemodynamic instability.
Long-term Follow-up Considerations
Reproductive Health Monitoring
- • Annual gynecological examinations
- • Preconception counseling for future pregnancies
- • Fertility evaluation if conception difficulties arise
- • Contraceptive counseling and planning
Preventive Care
- • Regular STI screening protocols
- • Partner evaluation and treatment strategies
- • Risk reduction education and counseling
- • Psychological support for chronic conditions
Prevention of complications requires comprehensive patient education about early symptom recognition, adherence to treatment regimens, and implementation of risk reduction strategies. Nursing professionals play essential roles in connecting patients with appropriate specialist care, supporting adherence to follow-up recommendations, and providing ongoing education about reproductive health maintenance following pelvic inflammatory disease treatment.
Evidence-Based Practice and Current Guidelines
Evidence-based practice guidelines for pelvic inflammatory disease provide the foundation for quality nursing care, ensuring that interventions are supported by current research and best practice recommendations. Nursing professionals must stay current with evolving guidelines from organizations such as the Centers for Disease Control and Prevention, the American College of Obstetricians and Gynecologists, and international reproductive health organizations.
Current CDC Treatment Guidelines (2021)
Outpatient Treatment Regimens
- • Ceftriaxone 500mg IM single dose PLUS
- • Doxycycline 100mg orally twice daily for 14 days
- • Alternative regimens for specific situations
- • Metronidazole addition for anaerobic coverage
Inpatient Treatment Criteria
- • Surgical emergencies cannot be excluded
- • Pregnancy
- • Lack of response to oral antimicrobials
- • Inability to follow or tolerate outpatient regimen
- • Severe illness, nausea, vomiting, or high fever
- • Tubo-ovarian abscess
Recent research developments in pelvic inflammatory disease management include advances in diagnostic technologies, antimicrobial resistance patterns, and prevention strategies. Nucleic acid amplification testing has revolutionized pathogen detection, while concerns about antibiotic resistance continue to influence treatment recommendations and surveillance programs.
Emerging Research Areas
- • Mycoplasma genitalium as emerging pathogen
- • Biomarker development for early diagnosis
- • Immunological factors in disease susceptibility
- • Novel antimicrobial agents and resistance
- • Microbiome influences on infection outcomes
Prevention Innovations
- • HPV vaccination program expansions
- • Point-of-care testing technologies
- • Mobile health applications for education
- • Partner notification technology platforms
- • Community-based intervention programs
Quality improvement initiatives in pelvic inflammatory disease care focus on reducing time to treatment initiation, improving patient education delivery, and enhancing follow-up compliance. Nursing professionals contribute to these initiatives through participation in quality metrics monitoring, patient satisfaction assessments, and outcome evaluation programs that drive continuous improvement in care delivery.
Key Performance Indicators for PID Care
Process Measures
- • Time from presentation to antibiotic initiation
- • Appropriate antibiotic selection and dosing
- • Partner notification and treatment rates
- • Patient education documentation completeness
Outcome Measures
- • Clinical cure rates at follow-up
- • Complication development rates
- • Patient satisfaction scores
- • Recurrence rates within specified timeframes
Implementation of evidence-based practice requires ongoing professional development, critical appraisal of research literature, and integration of new knowledge into clinical practice. Nursing professionals should engage in continuing education programs, participate in professional organizations, and contribute to research initiatives that advance understanding of pelvic inflammatory disease management and outcomes.
Future directions in pelvic inflammatory disease research include development of rapid diagnostic tools, personalized treatment approaches based on individual risk factors, and innovative prevention strategies targeting high-risk populations. Nursing professionals play vital roles in translating research findings into clinical practice and advocating for evidence-based policy changes that improve reproductive health outcomes for all women.
Conclusion and Key Takeaways
Pelvic inflammatory disease represents a complex reproductive health condition requiring comprehensive nursing knowledge, skilled clinical assessment, and evidence-based intervention strategies. The multifaceted nature of this condition demands that nursing professionals maintain expertise in pathophysiology, clinical manifestations, treatment protocols, and prevention strategies while demonstrating cultural competence and sensitivity in delivering care to affected women.
Essential Nursing Competencies for PID Care
Clinical Skills
- • Comprehensive reproductive health assessment
- • Pain management and comfort measures
- • Medication administration and monitoring
- • Recognition of complications and emergencies
Communication and Education
- • Sensitive sexual health discussions
- • Patient and partner education delivery
- • Cultural competence in care provision
- • Advocacy for patient needs and rights
The significance of early recognition and prompt treatment cannot be overstated, as delays in diagnosis and treatment directly correlate with increased risk of serious complications including infertility, ectopic pregnancy, and chronic pelvic pain. Nursing professionals serve as frontline healthcare providers in recognizing subtle symptoms, conducting thorough assessments, and initiating appropriate interventions that can prevent long-term reproductive health consequences.
Patient education emerges as a critical nursing intervention that extends beyond immediate treatment needs to encompass comprehensive prevention strategies, partner notification protocols, and long-term reproductive health planning. The effectiveness of educational interventions directly impacts treatment compliance, prevention of reinfection, and overall health outcomes for women affected by pelvic inflammatory disease.
Future Nursing Practice Implications
As healthcare continues to evolve, nursing professionals caring for women with pelvic inflammatory disease must adapt to emerging technologies, changing treatment guidelines, and evolving patient populations while maintaining focus on evidence-based, patient-centered care delivery.
Technology Integration
- • Electronic health record optimization
- • Telemedicine and remote monitoring
- • Mobile health applications
- • Point-of-care testing technologies
Quality Improvement
- • Outcome measurement and reporting
- • Patient satisfaction enhancement
- • Care coordination optimization
- • Evidence-based protocol development
The comprehensive approach to pelvic inflammatory disease care outlined in this study guide provides nursing professionals with the knowledge foundation necessary for delivering quality, evidence-based care to women affected by this significant reproductive health condition. Continued professional development, engagement with current research, and commitment to patient-centered care principles will ensure that nursing professionals remain prepared to meet the evolving challenges associated with pelvic inflammatory disease management and prevention in diverse healthcare settings.
