Physiological Adaptations During Pregnancy
Comprehensive guide for nursing students on maternal physiological changes
- Introduction to Physiological Adaptations
- Reproductive System Changes
- Cardiovascular System Changes
- Respiratory System Changes
- Urinary System Changes
- Gastrointestinal System Changes
- Metabolic Changes
- Skeletal Changes
- Skin Changes
- Endocrine System Changes
- Psychological Changes
- Global Practices in Prenatal Care
Introduction to Physiological Adaptations
Pregnancy represents one of the most profound periods of physiological adaptation in a woman’s life. These adaptations are necessary to accommodate the developing fetus, prepare the maternal body for delivery, and ensure optimal fetal development. Understanding these changes is crucial for nursing care and recognizing deviations from normal physiological adaptations that may indicate pathology.
Key concept: Physiological adaptations during pregnancy are driven by hormonal changes (primarily progesterone and estrogen) and mechanical factors due to the growing uterus. These adaptations affect virtually every organ system in the maternal body.
Reproductive System Changes
Uterine Adaptations
The uterus undergoes remarkable growth during pregnancy, transforming from a 70g pear-shaped organ to a 1100g muscular structure by term. This adaptation allows accommodation of the fetus, placenta, and amniotic fluid.
| Parameter | Pre-pregnancy | Term Pregnancy | Adaptation Purpose |
|---|---|---|---|
| Uterine Weight | 50-70g | 900-1100g | Support growing fetus |
| Uterine Cavity Volume | 10mL | 5000mL | Accommodate fetus, placenta, amniotic fluid |
| Uterine Blood Flow | 50mL/min | 500-700mL/min | Supply oxygen and nutrients to fetus |
| Myometrial Cell Changes | Normal size cells | Hypertrophy of existing cells | Increased contractile strength for labor |
Cervical Adaptations
The cervix undergoes significant adaptations during pregnancy to maintain pregnancy and then facilitate delivery:
- Softening (Goodell’s sign): Due to increased vascularity and water content
- Formation of mucus plug: Creates a protective barrier against ascending infections
- Collagen remodeling: Allows for cervical ripening and eventual dilation during labor
Vaginal Adaptations
The vagina adapts to prepare for the passage of the fetus:
- Increased vascularity and bluish coloration (Chadwick’s sign)
- Hypertrophy and hyperplasia of vaginal mucosa
- Increased vaginal secretions (leukorrhea) due to elevated estrogen levels
- Loosening of connective tissue for expansion during delivery
Breast Changes
The breasts undergo progressive adaptations to prepare for lactation:
- First trimester: Increased sensitivity, tingling, and fullness due to hormonal stimulation
- Second trimester: Enlargement of Montgomery’s tubercles, visible venous network
- Third trimester: Colostrum production, continued growth of glandular tissue
- Throughout pregnancy: Progressive darkening of nipples and areolae
B – Bigger size due to hormonal influence
R – Ready for lactation through ductal proliferation
E – Estrogen-driven changes in pigmentation
A – Areolar darkening and Montgomery tubercle development
S – Sensitivity increases, especially in first trimester
T – Tissue preparation for milk production
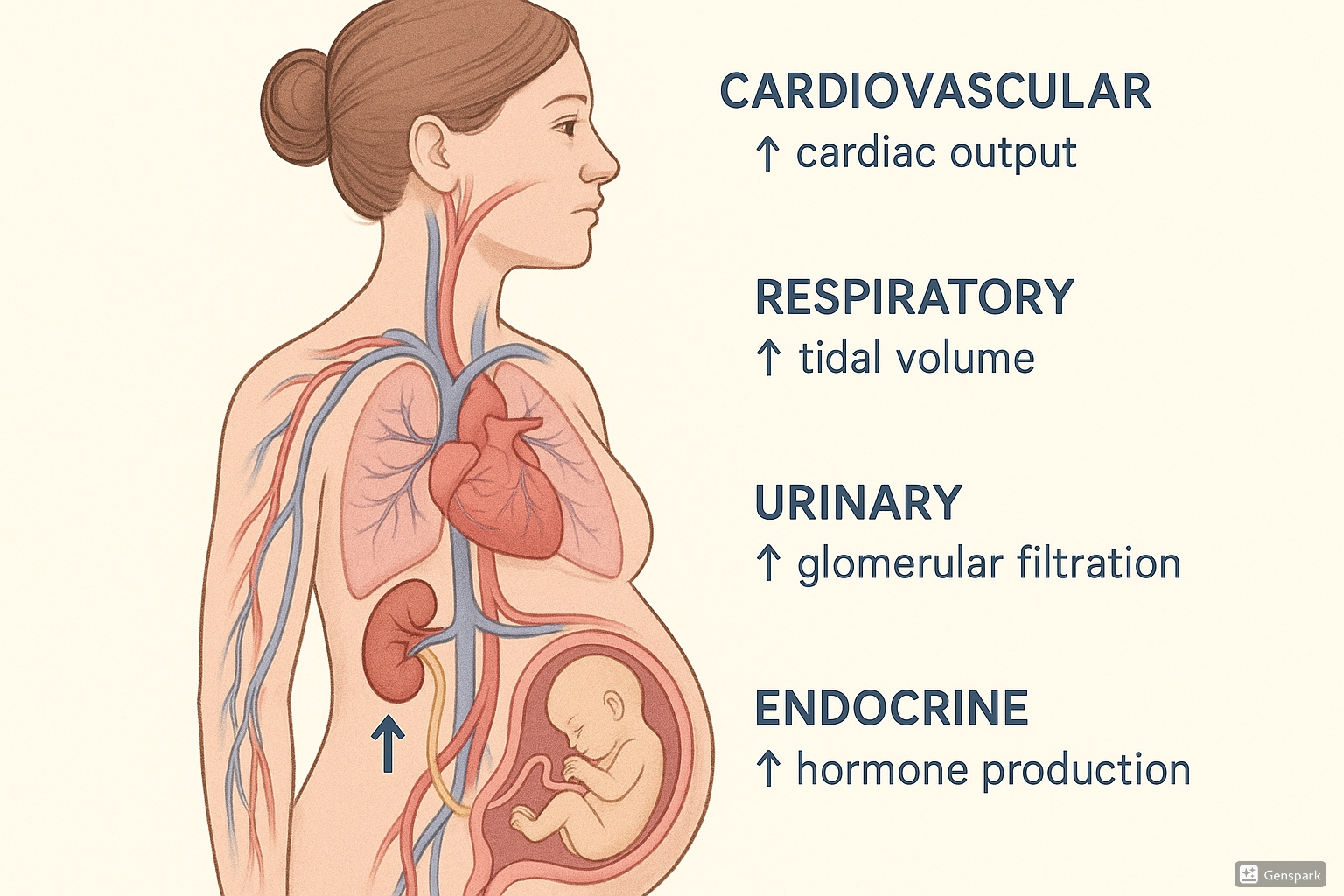
Cardiovascular System Changes
The cardiovascular system undergoes dramatic adaptations during pregnancy to meet the increased metabolic demands of both mother and fetus. These adaptations begin early in pregnancy and peak by the second trimester.
Blood Volume and Composition
One of the most significant cardiovascular adaptations is the increase in blood volume:
- Total blood volume increases by 30-50% (1500mL) by term
- Plasma volume increases by 40-50%
- Red blood cell (RBC) mass increases by 20-30%
- Results in physiologic anemia of pregnancy (dilutional effect)
- Hemoglobin typically decreases to 11-12 g/dL
Cardiac Adaptations
The heart adapts structurally and functionally to accommodate increased blood volume:
- Cardiac output: Increases 30-50% (from ~4.5 to 6-7 L/min)
- Heart rate: Increases by 10-20 beats per minute
- Stroke volume: Increases by 20-30%
- Left ventricular wall thickness: Mild hypertrophy
Cardiac output peaks at 25-30 weeks of gestation and remains elevated until delivery. The increased cardiac output is distributed primarily to the uterus (receiving 20-25% of cardiac output), kidneys, breasts, and skin.
Blood Pressure Changes
| Parameter | First Trimester | Second Trimester | Third Trimester |
|---|---|---|---|
| Systolic BP | Slight decrease | Decreases by 5-10 mmHg | Returns to pre-pregnancy levels |
| Diastolic BP | Slight decrease | Decreases by 10-15 mmHg | Returns to pre-pregnancy levels |
| Mean Arterial Pressure | Minimal change | Decreases | Gradually increases |
| Peripheral Vascular Resistance | Begins to decrease | Decreased by 35-40% | Begins to increase but remains below pre-pregnancy |
Venous System Changes
Venous adaptations during pregnancy include:
- Increased venous pressure in lower extremities
- Venous distensibility increases due to progesterone effect
- Compression of pelvic veins by enlarging uterus
- Predisposition to varicose veins and hemorrhoids
Hemostatic Changes
Pregnancy creates a hypercoagulable state due to:
- Increased clotting factors (I, VII, VIII, IX, X, XII)
- Decreased anticoagulant proteins (protein S)
- Altered fibrinolysis
- Increased platelet aggregation
H – Hypervolemia (increased blood volume)
E – Ejection fraction increases
A – Afterload decreases (reduced peripheral resistance)
R – Rate increases (elevated heart rate)
T – Thoracic displacement (heart shifted upward and to left)
Clinical Relevance: The supine hypotensive syndrome (vena caval syndrome) occurs when the pregnant uterus compresses the inferior vena cava in supine position, reducing venous return and cardiac output. Always position pregnant women in left lateral position during examination or procedures.
Respiratory System Changes
The respiratory system undergoes significant anatomical and functional adaptations to meet the increased oxygen demands of pregnancy. These adaptations ensure adequate oxygenation for both mother and fetus.
Anatomical Changes
- Diaphragm elevation: Rises up to 4cm due to enlarging uterus
- Thoracic cage changes: Subcostal angle widens from 68° to 103°
- Rib cage circumference: Increases by 5-7cm
- Upper airway: Capillary engorgement leading to nasal congestion, rhinitis of pregnancy
Ventilation Changes
| Parameter | Pre-pregnancy | Pregnancy Change | Physiological Impact |
|---|---|---|---|
| Tidal Volume (VT) | 500mL | ↑ 30-40% (650-700mL) | Increased gas exchange |
| Respiratory Rate | 12-15/min | Minimal change | Maintained breathing frequency |
| Minute Ventilation | 6-8 L/min | ↑ 40% (10-12 L/min) | Increased oxygen delivery |
| Expiratory Reserve Volume | 1000-1200mL | ↓ 20-25% | Reduced breathing reserve |
| Residual Volume | 1200mL | ↓ 20% | Decreased gas trapping |
| Functional Residual Capacity | 2400mL | ↓ 20-25% | Reduced oxygen reserve |
| Total Lung Capacity | 4200mL | ↓ 5% | Minimal impact on function |
| Vital Capacity | 3000mL | Minimal change | Maintained breathing capacity |
| Inspiratory Capacity | 3600mL | ↑ 5-10% | Enhanced inhalation capacity |
Gas Exchange and Acid-Base Balance
- Oxygen consumption: Increases by 20-30% due to fetal demands and maternal metabolism
- PaO2: Increases slightly to 100-104 mmHg
- PaCO2: Decreases to 28-32 mmHg due to hyperventilation (↓10mmHg)
- pH: Slight respiratory alkalosis (pH 7.40-7.45)
- Renal compensation: Increased bicarbonate excretion maintains pH balance
The increased minute ventilation (40% above pre-pregnant levels) is primarily driven by progesterone acting as a respiratory stimulant and increased maternal CO2 production. This leads to chronic respiratory alkalosis, which facilitates maternal-fetal CO2 exchange.
B – Breathing capacity increases (minute ventilation)
R – Respiratory alkalosis develops
E – Enlarged thoracic diameter
A – Airway congestion due to vascularization
T – Tidal volume increases significantly
H – Hypocapnia (decreased PaCO2)
E – Elevated diaphragm with advancing pregnancy
Clinical Implication: The respiratory adaptations during pregnancy result in limited respiratory reserve. This makes pregnant women more susceptible to hypoxemia during periods of hypoventilation, such as during sedation or general anesthesia.
Urinary System Changes
The urinary system undergoes significant anatomical and functional adaptations during pregnancy to handle increased filtration loads and accommodate the growing uterus.
Anatomical Changes
- Kidney size: Increases by 1-1.5cm in length due to increased renal vascular and interstitial volume
- Renal pelvis and ureter dilation: Begins in first trimester and more pronounced on the right side
- Bladder: Displaced upward and anteriorly flattened by the enlarging uterus
- Urethral elongation: Due to anterior displacement of bladder
Ureter dilation (hydroureter) and renal pelvis dilation (hydronephrosis) occur primarily due to progesterone-induced smooth muscle relaxation and mechanical compression from the enlarging uterus. The right ureter is typically more dilated than the left due to the dextrorotation of the uterus and right ovarian vein crossing.
Functional Changes
| Parameter | Pre-pregnancy | Pregnancy Change | Physiological Impact |
|---|---|---|---|
| Renal Plasma Flow | 600 mL/min | ↑ 50-80% (900-1080 mL/min) | Increased blood filtering |
| Glomerular Filtration Rate | 100-120 mL/min | ↑ 50% (150-180 mL/min) | Enhanced filtration capacity |
| Serum Creatinine | 0.8-1.0 mg/dL | ↓ 0.5-0.6 mg/dL | Reflects increased GFR |
| Blood Urea Nitrogen | 13-20 mg/dL | ↓ 8-10 mg/dL | Reflects increased GFR |
| Uric Acid | 2.5-5.5 mg/dL | ↓ (first half), ↑ (late pregnancy) | Changes in renal handling |
| Urinary Protein Excretion | <150 mg/day | ↑ up to 300 mg/day | Increased glomerular permeability |
| Glucose Filtration | Normal reabsorption | Increased filtration, can exceed reabsorption | Glucosuria without hyperglycemia |
Fluid and Electrolyte Balance
- Water retention: 6-8 liters total (including 3-4 liters in fetus, placenta, amniotic fluid)
- Sodium balance: Increased reabsorption despite increased GFR
- Potassium: Normal serum levels despite increased total body potassium
- Osmolality: Decreased by 10 mOsm/kg (from 290 to 280 mOsm/kg)
Bladder Function
Urinary frequency is a common symptom throughout pregnancy due to:
- First trimester: Hormonal effects and increased blood volume
- Second trimester: Slight improvement as uterus rises into abdomen
- Third trimester: Renewed frequency as presenting part descends into pelvis
- Throughout pregnancy: Increased bladder sensitivity and reduced capacity
U – Ureters dilate (more on right side)
R – Renal plasma flow increases
I – Increased GFR by 50%
N – Nitrogen waste products decrease (BUN, creatinine)
A – Altered tubular function (sodium retention)
R – Renin-angiotensin-aldosterone system activation
Y – Yielding frequent urination patterns
Clinical Relevance: The dilated urinary tract and urinary stasis predispose pregnant women to urinary tract infections. Additionally, the increased GFR can mask renal insufficiency as creatinine levels remain lower than expected despite reduced renal function.
Gastrointestinal System Changes
The gastrointestinal system undergoes various adaptations during pregnancy due to hormonal influences and mechanical pressure from the enlarging uterus.
Oral Cavity
- Gingival hyperemia: Increased vascularity and edema due to estrogen effects
- Gingival bleeding: More common during tooth brushing
- Ptyalism (excessive salivation): Can occur in some women, especially with nausea
Esophagus and Stomach
- Lower esophageal sphincter pressure: Decreases due to progesterone effect
- Gastric displacement: Stomach is pushed upward and rotated by the enlarging uterus
- Gastric emptying time: Generally unchanged in early pregnancy, may be prolonged in labor
- Gastric acid secretion: Decreases during pregnancy
- Heartburn: Affects 30-50% of pregnant women due to reduced LES tone and mechanical factors
Intestines
- Intestinal transit time: Prolonged due to progesterone effect on smooth muscle
- Small intestine absorption: Enhanced for certain nutrients (calcium, iron)
- Large intestine: Increased water absorption contributing to constipation
- Displacement: Intestines are pushed laterally and posteriorly by the enlarging uterus
Gallbladder and Hepatobiliary System
- Gallbladder emptying: Incomplete and sluggish due to progesterone effect
- Bile composition: More lithogenic (increased cholesterol saturation)
- Gallstone formation: Increased risk due to bile stasis and composition changes
Liver Function
| Parameter | Change in Pregnancy | Clinical Significance |
|---|---|---|
| Liver Size | No significant change | Palpable liver may indicate pathology |
| Serum Albumin | ↓ from 4.3 to 3.5 g/dL | Hemodilution effect; impacts drug binding |
| Alkaline Phosphatase | ↑ 2-4 times normal | Placental isoenzyme production |
| AST, ALT, GGT, Bilirubin | Normal or slightly decreased | Elevation suggests liver pathology |
| Plasma Proteins | ↓ Total protein, altered globulin profiles | Affects drug distribution and metabolism |
| Lipid Metabolism | ↑ Cholesterol, triglycerides, phospholipids | Meets fetal needs and prepares for lactation |
Common Gastrointestinal Symptoms
- Nausea and vomiting: Affects 50-90% of pregnancies, typically in first trimester
- Heartburn/GERD: Due to LES relaxation and mechanical pressure
- Constipation: Due to reduced motility and mechanical compression
- Hemorrhoids: Due to venous congestion and constipation
- Food cravings and aversions: Possibly protective mechanism or hormonal influence
D – Delayed emptying of stomach and intestines
I – Increased absorption of certain nutrients
G – Gastro-esophageal reflux due to LES relaxation
E – Elevated pressure from enlarging uterus
S – Slow intestinal transit time
T – Tendency for constipation and hemorrhoids
Clinical Relevance: The physiologic changes in the GI system during pregnancy can mask symptoms of underlying pathology. Right upper quadrant pain should always be evaluated carefully to differentiate between normal adaptation and potentially serious conditions like preeclampsia, HELLP syndrome, or acute fatty liver of pregnancy.
Metabolic Changes
Pregnancy induces profound metabolic adaptations to ensure adequate nutrition for the growing fetus while maintaining maternal homeostasis.
Weight Gain
The recommended total weight gain during pregnancy varies based on pre-pregnancy BMI:
| Pre-pregnancy BMI | Classification | Recommended Weight Gain |
|---|---|---|
| <18.5 kg/m² | Underweight | 12.5-18 kg (28-40 lbs) |
| 18.5-24.9 kg/m² | Normal weight | 11.5-16 kg (25-35 lbs) |
| 25.0-29.9 kg/m² | Overweight | 7-11.5 kg (15-25 lbs) |
| ≥30.0 kg/m² | Obese | 5-9 kg (11-20 lbs) |
Distribution of weight gain at term in a normal-weight woman:
- Fetus: 3.5 kg
- Placenta: 0.7 kg
- Amniotic fluid: 0.8 kg
- Uterus and breast tissue: 1.5 kg
- Maternal blood volume: 1.5 kg
- Maternal fluid: 1.5 kg
- Maternal fat stores: 3.5 kg
Carbohydrate Metabolism
Pregnancy is characterized by progressive insulin resistance and compensatory hyperinsulinemia:
- Fasting glucose: Decreases by 10-20% in early pregnancy
- Postprandial glucose: Increases due to insulin resistance
- Insulin production: Increases by 200-250% to maintain normoglycemia
- Insulin sensitivity: Decreases by 50-70% by late pregnancy
The development of insulin resistance during pregnancy facilitates glucose transfer to the fetus. This adaptation is mediated by placental hormones, including human placental lactogen (hPL), progesterone, estrogen, and cortisol. This “diabetogenic state” of pregnancy serves to ensure glucose availability for the fetus.
Lipid Metabolism
Pregnancy is associated with hyperlipidemia to support fetal growth:
- Total cholesterol: Increases by 25-50%
- Triglycerides: Increase by 200-400%
- LDL cholesterol: Increases by 50%
- HDL cholesterol: Increases in early pregnancy, then decreases
- Free fatty acids: Increase to provide alternative fuel for mother
Protein Metabolism
- Positive nitrogen balance throughout pregnancy
- Increased protein synthesis for fetal and placental growth
- Enhanced amino acid transport across the placenta
- Decreased protein catabolism during fasting
Basal Metabolic Rate and Energy Requirements
- BMR: Increases by 15-20% by term
- Total energy requirement: Increases by approximately 300 kcal/day
- First trimester: Minimal increased requirement
- Second trimester: Additional 340 kcal/day
- Third trimester: Additional 450 kcal/day
Water and Electrolyte Balance
- Total body water increases by 6-8 liters
- Sodium retention increases by 500-900 mEq
- Potassium retention increases by 300-350 mEq
- Decreased plasma osmolality by 10 mOsm/kg
Vitamin and Mineral Metabolism
| Nutrient | Change in Requirement | Significance |
|---|---|---|
| Folate | ↑ 100% (600 μg/day) | Neural tube development, DNA synthesis |
| Iron | ↑ 50% (27 mg/day) | Increased erythropoiesis, fetal stores |
| Calcium | ↑ 50% (1000-1300 mg/day) | Fetal skeletal development |
| Vitamin D | ↑ (600-800 IU/day) | Calcium absorption and metabolism |
| Vitamin B12 | ↑ (2.6 μg/day) | Cell division, neural development |
| Zinc | ↑ (11-13 mg/day) | Cell division, protein synthesis |
| Iodine | ↑ (220-250 μg/day) | Thyroid hormone synthesis |
M – More energy requirements (+300 kcal/day)
E – Enhanced insulin production
T – Triglycerides and lipids increase
A – Anabolic state with positive nitrogen balance
B – Basal metabolic rate increases
O – Obligatory weight gain for maternal/fetal tissues
L – Lipolysis in fasting state to spare glucose
I – Insulin resistance develops
S – Substrate prioritization for fetal needs
M – Mineral requirements increase significantly
Skeletal Changes
During pregnancy, the skeletal system adapts to accommodate the growing fetus and prepare for delivery. These adaptations are primarily driven by hormonal changes, particularly relaxin, progesterone, and estrogen.
Pelvic Adaptations
- Pelvic joints relaxation: Softening and increased mobility of symphysis pubis and sacroiliac joints
- Symphysis pubis: Separation increases by 3-8 mm
- Pelvic diameter: Increases by 1-3 cm in preparation for childbirth
- Sacrococcygeal joint: Increased mobility for passage of fetus
Spinal Changes
- Lumbar lordosis: Progressive increase to maintain center of gravity
- Thoracic kyphosis: Compensatory increase
- Intervertebral disc pressure: Increases, especially in L4-L5 and L5-S1 regions
The progressive lordosis during pregnancy is a compensatory mechanism to maintain the center of gravity over the lower limbs as the abdomen enlarges. This postural adaptation, combined with joint laxity, contributes to the characteristic “waddling gait” of late pregnancy and can lead to lower back pain in up to 70% of pregnant women.
Calcium Metabolism
Pregnancy increases calcium demands for fetal skeletal development:
- Calcium requirement: Increases to 1000-1300 mg/day
- Intestinal absorption: Doubles during pregnancy
- Fetal accumulation: 25-30 g of calcium by term (mostly in third trimester)
- Maternal bone turnover: Increases, with modest decrease in BMD (recovered postpartum)
Postural Changes
- Center of gravity: Shifts anteriorly as pregnancy progresses
- Stance: Feet placed wider apart for increased stability
- Gait: Development of characteristic “waddling gait” in late pregnancy
- Weight distribution: Shift to heels and lateral foot borders
Common Musculoskeletal Symptoms
| Symptom | Prevalence | Primary Cause | Management |
|---|---|---|---|
| Lower back pain | 50-70% | Lordosis, joint laxity, weight gain | Proper body mechanics, supportive garments, physical therapy |
| Pelvic girdle pain | 20-45% | Joint laxity, altered biomechanics | Pelvic support belt, modified activity, physical therapy |
| Carpal tunnel syndrome | 20-45% | Fluid retention, vascular compression | Wrist splinting, elevation, modified activities |
| Leg cramps | 30-50% | Calcium/magnesium changes, fatigue | Stretching, calcium supplementation, hydration |
| Round ligament pain | 10-30% | Stretching of supporting ligaments | Position changes, heat application, support garments |
P – Pelvic joint relaxation
O – Orthopedic changes in spinal curvature
S – Symphysis pubis widens
T – Thoracic kyphosis increases
U – Unstable joints due to ligament laxity
R – Relaxin hormone effects on ligaments
E – Enlarged abdomen shifts center of gravity
Clinical Relevance: While joint laxity is a normal physiological adaptation, severe symphyseal separation (>10 mm) or significant pelvic pain may indicate symphysis pubis dysfunction (SPD) that requires specialized management including physical therapy, pelvic support belts, and modified activity.
Skin Changes
The skin undergoes numerous physiological adaptations during pregnancy due to hormonal, immunological, and mechanical factors. Many of these changes regress postpartum, but some may persist.
Pigmentary Changes
- Melasma (chloasma): Symmetrical hyperpigmentation on face, affects 50-70% of pregnant women
- Linea nigra: Vertical hyperpigmented line from pubis to umbilicus or xiphoid
- Areolar darkening: Increased pigmentation of nipples and areolae
- Genital darkening: Hyperpigmentation of vulva, perineum, and perianal region
- Axillary darkening: Increased pigmentation in axillae
- Nevus darkening: Existing moles may darken during pregnancy
Pigmentary changes during pregnancy are primarily due to increased melanocyte-stimulating hormone (MSH), estrogen, and progesterone. Melasma is often called the “mask of pregnancy” and tends to be more pronounced in women with darker skin tones. Sun exposure exacerbates these pigmentary changes, making sun protection particularly important during pregnancy.
Vascular Changes
- Spider angiomas: Small, dilated blood vessels, typically on face, neck, chest, and arms
- Palmar erythema: Redness of the palms, especially thenar and hypothenar eminences
- Varicosities: Vulvar, rectal, and leg veins may become dilated
- Gingival hyperemia: Increased vascularity of gums
- Non-pitting edema: Especially in hands, face, and ankles
Connective Tissue Changes
- Striae gravidarum (stretch marks): Affect 50-90% of pregnant women
- Location: Primarily on abdomen, breasts, thighs, and buttocks
- Appearance: Initially pink/purple, later fade to silvery-white
- Risk factors: Younger maternal age, higher BMI, positive family history, excessive weight gain
Hair and Nail Changes
| Structure | Changes During Pregnancy | Postpartum Changes |
|---|---|---|
| Scalp Hair | Increased anagen (growth) phase, decreased telogen (resting) phase, thicker appearance | Telogen effluvium (hair shedding) 2-4 months postpartum |
| Body Hair | Hirsutism in androgen-dependent areas (face, abdomen, chest) | Usually resolves postpartum |
| Nails | Faster growth, increased brittleness, distal onycholysis | Return to pre-pregnancy status |
| Sebaceous Glands | Increased activity (may worsen acne or improve pre-existing acne) | Return to pre-pregnancy activity |
| Eccrine Glands | Increased activity, hyperhidrosis | Return to pre-pregnancy activity |
Specific Dermatoses of Pregnancy
- Pruritic urticarial papules and plaques of pregnancy (PUPPP): Most common pregnancy-specific dermatosis
- Pemphigoid gestationis: Autoimmune blistering disorder specific to pregnancy
- Intrahepatic cholestasis of pregnancy: Liver disorder with skin manifestation of intense pruritus
- Prurigo of pregnancy: Small, excoriated papules due to intense itching
S – Spider angiomas develop
K – Kevlar-like stretch marks (striae gravidarum)
I – Increased pigmentation (melasma, linea nigra)
N – Nail changes and hair cycle alterations
Clinical Relevance: While most skin changes during pregnancy are benign and resolve postpartum, generalized pruritus without a rash, especially in the third trimester, should prompt investigation for intrahepatic cholestasis of pregnancy, which can be associated with adverse fetal outcomes if left untreated.
Endocrine System Changes
Pregnancy induces profound adaptations in the endocrine system, involving both maternal endocrine glands and the development of the placenta as a temporary endocrine organ.
Placental Hormones
- Human Chorionic Gonadotropin (hCG):
- Production begins shortly after implantation
- Peaks at 8-10 weeks of gestation
- Maintains corpus luteum function in early pregnancy
- Stimulates maternal thyroid gland
- Basis for pregnancy tests
- Human Placental Lactogen (hPL):
- Increases progressively throughout pregnancy
- Promotes insulin resistance and lipolysis
- Ensures glucose availability for fetus
- Promotes mammary gland development
- Estrogens:
- Produced in increasing amounts throughout pregnancy
- Promote uterine growth and vascularity
- Stimulate breast development
- Increase protein synthesis
- Progesterone:
- Essential for maintaining pregnancy
- Reduces uterine contractility
- Promotes mammary gland development
- Causes smooth muscle relaxation
Pituitary Gland Changes
| Hormone | Change During Pregnancy | Physiological Effect |
|---|---|---|
| Prolactin | ↑ 10-20 fold by term | Prepares breasts for lactation |
| Growth Hormone | ↓ Replaced by placental GH variant | Placental GH mediates insulin resistance |
| ACTH | Slight ↑ | Stimulates adrenal cortex |
| TSH | Slight ↓ in first trimester, then normalizes | Response to increased thyroid hormones |
| FSH/LH | Suppressed | No ovulation during pregnancy |
| Oxytocin | ↑ At term and during labor | Uterine contractions and milk ejection |
| Vasopressin (ADH) | Slight ↑ in response to decreased osmolality | Water retention |
The pituitary gland enlarges by approximately 135% during pregnancy due to hyperplasia and hypertrophy of lactotroph cells that produce prolactin. This increased size can occasionally lead to visual field defects if a pre-existing pituitary adenoma is present.
Thyroid Gland Changes
- Gland size: Increases by 10-15%
- Total T4 and T3: Increase by 50% due to increased TBG
- Free T4 and T3: Initially increase, then return to normal range
- Thyroid-binding globulin (TBG): Increases due to estrogen effect
- Iodine requirements: Increase by 50%
- First trimester: hCG has TSH-like activity, causing temporary suppression of TSH
Parathyroid and Calcium Homeostasis
- PTH: Initially decreases, then increases in late pregnancy
- Ionized calcium: Generally maintained within normal limits
- Vitamin D metabolism: Increased conversion to active form
- Calcitonin: Increases throughout pregnancy
- Intestinal calcium absorption: Doubles during pregnancy
Adrenal Gland Changes
- Cortisol: Total levels increase 2-3 fold (free cortisol increases less)
- CBG (Cortisol binding globulin): Increases due to estrogen effect
- DHEA-S: Decreases due to increased clearance
- Aldosterone: Increases 3-10 fold
- Renin activity: Increases 8-10 fold
- Angiotensinogen: Increases due to estrogen stimulation
Pancreatic Changes
- Insulin response: Biphasic pattern
- First half: Enhanced insulin sensitivity
- Second half: Progressive insulin resistance
- β-cell hyperplasia: Increased insulin production
- Fasting glucose: Decreased by 10-20%
- Postprandial glucose: Increased due to insulin resistance
H – hCG maintains corpus luteum function
O – Oxytocin increases at term for labor
R – Relaxin promotes joint laxity
M – Metabolic changes from placental hormones
O – Ovarian function suppressed
N – New insulin resistance develops
E – Estrogen and progesterone increase
S – Stimulated thyroid function
Clinical Relevance: The increased metabolic demands and insulin resistance of pregnancy can unmask subclinical thyroid disorders or diabetes. Screening for gestational diabetes is recommended between 24-28 weeks of gestation, while thyroid function should be monitored in women with pre-existing thyroid disease or risk factors.
Psychological Changes
Pregnancy is a time of significant psychological adaptation as women prepare for the transition to motherhood. These changes are influenced by hormonal factors, social context, personal history, and cultural expectations.
First Trimester Psychological Adaptations
- Ambivalence: Mixed feelings about pregnancy, even in planned pregnancies
- Emotional lability: Rapid mood swings possibly related to hormonal fluctuations
- Introspection: Focus turns inward as woman processes pregnancy reality
- Identity adjustment: Beginning to integrate motherhood into self-concept
- Anxiety: Concerns about pregnancy viability and fetal health
Second Trimester Psychological Adaptations
- Emotional stabilization: Often described as the “honeymoon period”
- Body image adjustments: Acceptance of changing body as pregnancy becomes visible
- Fetal bonding: Intensifies after quickening (feeling fetal movements)
- Nesting behaviors: Begin preparing home and acquiring items for baby
- Role transition: Active mental preparation for maternal role
Third Trimester Psychological Adaptations
- Increased anxiety: Concerns about labor, delivery, and parenting abilities
- Physical discomfort impact: Sleep disturbances and physical limitations may affect mood
- Impatience: Desire for pregnancy to end and meet the baby
- Vulnerability: Heightened emotional sensitivity and need for support
- Future orientation: Mental rehearsal for labor, delivery, and early parenting
Developmental Tasks of Psychological Adaptation
| Developmental Task | Description | Manifestation |
|---|---|---|
| Accepting the pregnancy | Emotional reconciliation with pregnancy reality | Moving from surprise/shock to acceptance |
| Developing maternal identity | Integrating mother role into self-concept | Imagining self as mother, relationship with child |
| Resolving relationship with own mother | Reprocessing childhood experiences | Reconciling how one was mothered with how one will mother |
| Establishing relationship with fetus | Developing emotional connection with baby | Talking to baby, name selection, preparing space |
| Preparing for birth and parenting | Practical and emotional preparation | Education, support system development, planning |
Hormonal Influences on Mood
- Estrogen: Affects serotonin, norepinephrine, and dopamine systems
- Progesterone: Has anxiolytic and sedative effects via GABA receptors
- Cortisol: Elevated levels may affect mood regulation
- Oxytocin: Promotes bonding behaviors and reduces stress
- Thyroid hormones: Fluctuations can impact mood and energy
Risk Factors for Psychological Distress
- Personal history: Prior depression, anxiety, or trauma
- Social factors: Limited support, relationship conflict, financial stress
- Obstetric factors: Pregnancy complications, history of loss
- Life stressors: Major life changes coinciding with pregnancy
- Physical factors: Severe pregnancy symptoms, sleep disruption
Between 15-25% of women experience significant depressive symptoms during pregnancy. Untreated prenatal depression is associated with poor self-care, inadequate nutrition, substance use, and increased risk of postpartum depression. Screening for depression should be conducted at least once during pregnancy using validated tools such as the Edinburgh Postnatal Depression Scale (EPDS) or the Patient Health Questionnaire (PHQ-9).
M – Mood changes throughout pregnancy
O – Opportunity for personal growth
T – Transition in identity and relationships
H – Hormonal influences on emotional state
E – Expectations adjustment (self and societal)
R – Relationship changes with partner and family
Clinical Relevance: Psychological adaptation during pregnancy is as important as physical adaptation for maternal-fetal wellbeing. Normalizing common emotional reactions while screening for more serious mood disorders is an essential component of comprehensive prenatal care. Supporting healthy psychological adaptation can improve pregnancy outcomes and postpartum adjustment.
Global Practices in Prenatal Care
Different cultures and healthcare systems around the world have developed various approaches to managing the physiological adaptations of pregnancy. Here are some notable practices:
Scandinavian Model
- Emphasizes midwife-led continuity of care throughout pregnancy
- Focuses on pregnancy as a normal physiological process rather than a medical condition
- Incorporates comprehensive psychological support alongside physical monitoring
- Uses fewer interventions while maintaining excellent maternal-fetal outcomes
- Prioritizes work-life balance with generous parental leave policies
Japanese Approach
- Incorporates traditional concept of “Anzan” (safe birth) through dietary recommendations
- Promotes specific prenatal exercises to facilitate optimal fetal positioning
- Emphasizes “Satogaeri bunben” – returning to maternal family home for support during later pregnancy and early postpartum
- Uses abdominal binding techniques postpartum to support physiological recovery
Ayurvedic Traditions (India)
- Classifies pregnancy into three trimesters with specific dietary and lifestyle recommendations for each
- Uses selected herbs to support maternal physiological adaptations
- Incorporates oil massage techniques to relieve musculoskeletal discomfort
- Emphasizes balance of doshas (bodily humors) for optimal pregnancy health
Group Prenatal Care Models
- Pioneered in the United States and spreading globally
- Combines individual clinical assessment with group education and support
- Improves health literacy regarding normal physiological changes
- Reduces social isolation and normalizes pregnancy experiences
- Shows improved outcomes especially for vulnerable populations
Research suggests that culturally congruent care that respects physiological processes while providing appropriate monitoring leads to improved satisfaction and outcomes. Integration of beneficial practices across cultural approaches represents an opportunity to enhance modern obstetric care.
Best Practice: Regardless of cultural context, the most effective prenatal care models share common elements: respect for the normal physiological processes of pregnancy, appropriate monitoring for deviations from normal, continuity of care, comprehensive education, psychological support, and cultural sensitivity. These elements help women navigate the significant physiological and psychological adaptations of pregnancy with confidence.
