Physiology of Lactation and Lactation Management
Comprehensive Notes for Nursing Students
Table of Contents
- 1. Introduction to Lactation
- 2. Anatomy of the Breast
- 3. Hormonal Control of Lactation
- 4. Stages of Lactation
- 5. Breast Milk Composition
- 6. Physiology of Milk Production and Secretion
- 7. Lactation Management
- 8. Challenges in Lactation and Solutions
- 9. Baby Attachment and Effective Suckling
- 10. Best Practices in Lactation Support
- 11. References
1. Introduction to Lactation
Lactation is the physiological process by which milk is synthesized and secreted from the mammary glands of postpartum females. This complex biological process begins during pregnancy and continues until weaning. The primary purpose of lactation is to provide optimal nutrition and immunological protection for the newborn.
Understanding the physiology of lactation is vital for healthcare professionals, particularly nurses who play a crucial role in supporting mothers through the breastfeeding journey. This knowledge enables healthcare providers to offer evidence-based care, prevent and manage breastfeeding difficulties, and promote successful breastfeeding outcomes.
Key Aspects of Lactation:
- Breast development (mammogenesis)
- Initiation of milk secretion (lactogenesis)
- Ongoing milk production (galactopoiesis)
- Milk ejection reflex (let-down)
- Regulation of milk synthesis and secretion
2. Anatomy of the Breast
The female breast is a specialized organ designed for milk production and delivery. Understanding its structure is fundamental to comprehending lactation physiology.
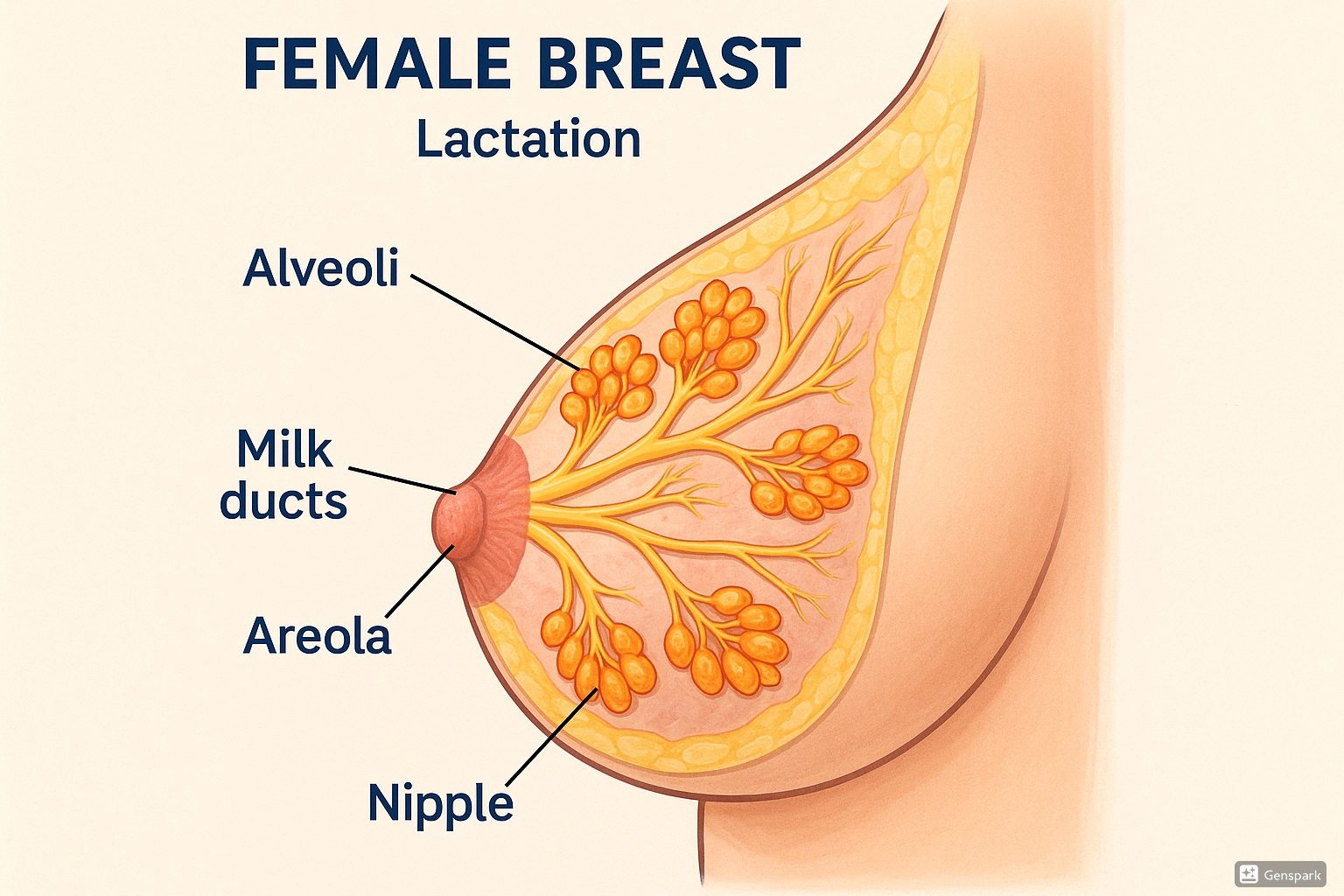
Key Anatomical Structures:
Alveoli (Milk-Producing Units)
Clustered sac-like structures composed of milk-secreting epithelial cells. These are the functional units of the mammary gland where milk components are synthesized and secreted.
Myoepithelial Cells
Specialized contractile cells surrounding the alveoli that contract in response to oxytocin, squeezing milk from the alveoli into the duct system.
Lactiferous Ducts
A network of tubular structures that transport milk from the alveoli toward the nipple. Each breast contains approximately 15-20 lactiferous ducts.
Lactiferous Sinuses
Dilated portions of the ducts near the nipple that serve as temporary milk reservoirs during feeding.
Nipple and Areola
The nipple contains multiple duct openings through which milk exits. The areola contains Montgomery’s tubercles that secrete lubricating oils to protect the nipple during breastfeeding.
Supporting Structures
Connective tissue, ligaments (Cooper’s ligaments), adipose tissue, blood vessels, lymphatic vessels, and nerves that support and sustain the functional components of the breast.
3. Hormonal Control of Lactation
Lactation is regulated by a complex interplay of hormones that coordinate the development of the mammary gland, milk production, and milk ejection.
Primary Hormones Involved in Lactation
| Hormone | Source | Primary Function in Lactation |
|---|---|---|
| Prolactin | Anterior Pituitary | Stimulates milk production; levels increase in response to nipple stimulation during suckling |
| Oxytocin | Posterior Pituitary | Triggers milk ejection (let-down reflex) by causing myoepithelial cells to contract |
| Estrogen | Ovaries (non-pregnant state) Placenta (pregnancy) |
Stimulates ductal development during puberty and pregnancy; high levels inhibit lactation during pregnancy |
| Progesterone | Ovaries (luteal phase) Placenta (pregnancy) |
Promotes alveolar development during pregnancy; inhibits lactation during pregnancy |
| Human Placental Lactogen (hPL) | Placenta | Prepares mammary tissue for lactation during pregnancy |
| Insulin | Pancreas | Facilitates milk synthesis by enhancing glucose uptake by mammary cells |
| Cortisol | Adrenal Cortex | Supports milk synthesis by stimulating production of milk proteins and enzymes |
| Thyroid Hormones | Thyroid Gland | Maintain metabolic activity in mammary tissue |
Hormonal Regulation Pathways
Prolactin Pathway
- Infant suckling stimulates sensory nerves in nipple
- Impulses travel to hypothalamus
- Hypothalamus decreases dopamine (prolactin inhibiting factor) release
- Decreased dopamine allows increased prolactin secretion
- Prolactin travels via bloodstream to mammary alveoli
- Stimulates milk synthesis for the next feeding
Oxytocin Pathway
- Nipple stimulation sends sensory signals to hypothalamus
- Hypothalamus triggers oxytocin release from posterior pituitary
- Oxytocin travels via bloodstream to mammary glands
- Binds to receptors on myoepithelial cells
- Causes contraction of myoepithelial cells
- Results in milk ejection (let-down) for current feeding
Mnemonic: “POLL” – Primary hormones of Lactation
- Prolactin – Produces milk
- Oxytocin – Outputs milk (via let-down)
- Low estrogen – Lets lactation begin
- Low progesterone – Launches milk production
Important Note on Oxytocin:
Oxytocin release can be triggered not only by physical nipple stimulation but also by:
- Seeing the baby
- Hearing the baby cry
- Thinking about the baby
- Preparing to breastfeed
This is why a calm, supportive environment is essential for successful lactation. Stress, anxiety, and pain can inhibit oxytocin release and impair the milk ejection reflex.
4. Stages of Lactation
Lactation develops through several distinct stages, from pregnancy through weaning. Each stage involves specific physiological changes in the mammary gland.
| Stage | Timing | Key Events | Hormonal Controls |
|---|---|---|---|
| Mammogenesis | Puberty and Pregnancy | Development of mammary gland structure; Preparation of breast tissue for milk production | Estrogen, progesterone, prolactin, human placental lactogen, growth hormone |
| Lactogenesis I | Mid-pregnancy (15-20 weeks) | Differentiation of alveolar cells into secretory cells; Limited secretory capability develops | Prolactin, human placental lactogen, cortisol (inhibited by estrogen and progesterone) |
| Lactogenesis II | Postpartum days 2-5 | “Milk coming in”; Transition from colostrum to mature milk; Copious milk production begins | Drop in progesterone after placental delivery; Continued prolactin stimulus |
| Galactopoiesis | Established lactation until weaning | Maintenance of established milk production | Primarily prolactin and oxytocin; Regulated by milk removal |
| Involution | After weaning | Regression of lactating tissue; Reduction in milk production | Decreased prolactin due to reduced stimulation; Local factors in the breast |
Mnemonic: “MILKY” – Stages of Lactation
- Mammogenesis – Mammary tissue development
- Initiation (Lactogenesis I) – Initial secretory capability
- Lactogenesis II – Launching milk production
- Keeping it going (Galactopoiesis) – Keeping milk production active
- Yielding to cessation (Involution) – Yielding to natural end of lactation
Colostrum vs. Transitional vs. Mature Milk
| Characteristic | Colostrum | Transitional Milk | Mature Milk |
|---|---|---|---|
| Timing | Birth to 2-5 days | 5-14 days postpartum | After 14 days postpartum |
| Appearance | Yellow, thick, sticky | Whiter, increased volume | Thin, white or slightly bluish |
| Volume | 40-50 mL/day | Increasing to 500-750 mL/day | 750-800 mL/day (average) |
| Protein | High (especially immunoglobulins) | Decreasing | Lower than colostrum |
| Fat | Lower | Increasing | Higher than colostrum |
| Lactose | Lower | Increasing | Higher than colostrum |
| Immunological Properties | Very high (IgA, leukocytes, etc.) | Decreasing but still significant | Lower than colostrum but still present |
| Key Functions | Immunological protection, laxative effect (meconium clearance) | Transition to nutritional focus | Complete nutrition for infant growth |
5. Breast Milk Composition
Human breast milk is a complex biological fluid that contains all the essential nutrients required for optimal infant growth and development, as well as numerous bioactive components that provide protection against infection and support organ development.
Macronutrients in Mature Breast Milk
| Component | Concentration | Characteristics | Functions |
|---|---|---|---|
| Carbohydrates (primarily lactose) | 7 g/100 mL | Disaccharide unique to milk; Oligosaccharides also present | Primary energy source; Promotes calcium absorption; Oligosaccharides support gut microbiome development |
| Proteins | 0.9 g/100 mL | Whey:casein ratio = 60:40 (differs from cow milk); Contains alpha-lactalbumin, lactoferrin, secretory IgA | Growth and development; Immune protection; Easily digestible |
| Fats | 3.5 g/100 mL | Concentration increases during a feeding (foremilk vs. hindmilk); Contains essential fatty acids including DHA and ARA | Main energy source (provides ~50% of energy); Brain and nervous system development; Fat-soluble vitamin carrier |
| Water | 87.5% | Hydration fluid | Maintains hydration; No additional water needed for exclusively breastfed infants |
Micronutrients and Bioactive Components
Vitamins and Minerals
- Fat-soluble vitamins: A, D, E, K
- Water-soluble vitamins: B complex, C
- Minerals: Calcium, phosphorus, magnesium, sodium, potassium
- Trace elements: Iron, zinc, copper, selenium
- Note: Vitamin D is relatively low, supplementation often recommended
Immune Factors
- Secretory IgA: Protects mucosal surfaces
- Lactoferrin: Iron-binding protein with antimicrobial properties
- Lysozyme: Enzyme that destroys bacterial cell walls
- Leukocytes: White blood cells that provide active immunity
- Oligosaccharides: Prevent bacterial attachment to mucosal surfaces
Growth Factors
- Epidermal Growth Factor: Promotes intestinal maturation
- Nerve Growth Factors: Support neurological development
- Insulin-like Growth Factors: Promote cell growth and differentiation
- Vascular Endothelial Growth Factor: Supports blood vessel development
Enzymes and Other Bioactive Components
- Bile Salt-Stimulated Lipase: Aids fat digestion
- Amylase: Helps digest complex carbohydrates
- Cytokines: Immune system modulators
- Nucleotides: Support immune function and gut development
- MicroRNAs: Regulate gene expression in the infant
Dynamic Nature of Breast Milk:
Breast milk composition is not static but varies:
- During a feeding: Fat content increases as the feed progresses (foremilk vs. hindmilk)
- Over 24 hours: Some components show diurnal variations
- Over the course of lactation: Changes from colostrum to transitional to mature milk
- According to infant’s gestational age: Milk for preterm infants differs from milk for term infants
- With maternal diet: Some nutrients and flavors reflect mother’s food intake
This dynamic composition allows breast milk to uniquely meet the changing needs of the growing infant.
Mnemonic: “PERFECT MILK” – Unique Components of Human Milk
- Protective antibodies (sIgA, etc.)
- Enzymes for digestion
- Right fat profile (including DHA, ARA)
- Factors for growth and development
- Easily digestible proteins
- Carbohydrates (lactose and oligosaccharides)
- Tailored to infant needs
- Minerals in bioavailable forms
- Immune cells (leukocytes)
- Lactoferrin and lysozyme
- Key vitamins for development
6. Physiology of Milk Production and Secretion
The physiological processes involved in milk production and secretion are complex and involve several coordinated mechanisms at the cellular and organ level.
Milk Synthesis in the Alveolar Cells
Protein Synthesis
- Amino acids taken up from maternal circulation
- Milk proteins synthesized in rough endoplasmic reticulum
- Processed through Golgi apparatus
- Packaged into secretory vesicles
- Released into alveolar lumen by exocytosis
Fat Synthesis
- Fatty acids obtained from diet, maternal stores, or synthesized in the cell
- Triglyceride synthesis occurs in smooth endoplasmic reticulum
- Lipid droplets form and grow in cytoplasm
- Droplets migrate to apical cell membrane
- Secreted by unique budding process (milk fat globule formation)
Lactose Synthesis
- Glucose enters alveolar cell from maternal circulation
- Some glucose converted to galactose
- Lactose synthase enzyme combines glucose and galactose
- Lactose synthesis occurs in Golgi apparatus
- Secreted via exocytosis along with proteins
Note: Lactose draws water into milk by osmosis, determining milk volume
Other Components
- Vitamins and minerals: Transported from maternal circulation
- Immunoglobulins: Transported from maternal circulation (IgA) or produced locally
- Water: Follows lactose via osmosis
- Electrolytes: Transported via various mechanisms
Milk Secretion Pathways
| Pathway | Components Secreted | Mechanism |
|---|---|---|
| Exocytotic Pathway (I) | Proteins, lactose, calcium, phosphate, citrate | Secretory vesicles fuse with apical plasma membrane |
| Lipid Pathway (II) | Lipids, fat-soluble vitamins | Milk fat globules enveloped by plasma membrane during secretion |
| Transcytotic Pathway (III) | Immunoglobulins, hormones, growth factors | Transport of intact proteins from interstitial space to milk |
| Membrane Transport Pathway (IV) | Sodium, potassium, chloride, glucose | Via specific membrane transporters between compartments |
| Paracellular Pathway (V) | Plasma components, leukocytes | Between cells through tight junctions (primarily during pregnancy, involution, and inflammation) |
Regulation of Milk Production
Endocrine (Hormonal) Control
- Primary in initiating lactation
- Prolactin essential for milk synthesis
- Oxytocin necessary for milk ejection
- Other hormones provide supportive roles
- Dominant in early lactation (first few weeks)
Autocrine (Local) Control
- Dominant in established lactation
- Feedback Inhibitor of Lactation (FIL)
- Present in milk itself
- Accumulates when milk is not removed
- Inhibits further milk production
- Explains supply-and-demand nature of milk production
Supply and Demand Principle:
The autocrine control of lactation explains why:
- More frequent feeding increases milk production
- Decreased breast emptying leads to decreased supply
- Each breast regulates its production independently
- Milk production generally matches infant needs
- Complete breast emptying is essential to maintain supply
Understanding this principle is fundamental for clinical management of lactation.
The Milk Ejection (Let-Down) Reflex
Sequence of Events
- Stimulation of nipple/areola mechanoreceptors during suckling
- Afferent nerve impulses to hypothalamus
- Oxytocin release from posterior pituitary
- Oxytocin travels via bloodstream to breast
- Binds to receptors on myoepithelial cells around alveoli and small ducts
- Myoepithelial cell contraction
- Milk ejection from alveoli into duct system
- Milk becomes available to the infant
Clinical Signs of Milk Ejection
In the Mother:
- Tingling or pins-and-needles sensation in breasts
- Milk dripping from opposite breast
- Uterine cramping (especially early postpartum)
- Increased thirst during feeding
- Feeling of relaxation or drowsiness
In the Infant:
- Change from short, quick sucks to deep, rhythmic suckling
- Audible swallowing
- Milk visible in infant’s mouth or dripping
- Relaxation of infant’s hands
- Milk dripping from corner of mouth
Factors That Can Inhibit Milk Ejection:
- Pain (during breastfeeding or otherwise)
- Psychological stress or anxiety
- Embarrassment or self-consciousness
- Cold environment
- Alcohol and certain medications
- Excessive fatigue
Milk ejection inhibition can lead to inadequate milk transfer despite adequate production, resulting in infant frustration and potentially reduced milk supply over time.
7. Lactation Management
Effective lactation management involves supporting the physiological processes of lactation while addressing potential challenges. Healthcare providers, particularly nurses, play a crucial role in this support.
Essential Components of Lactation Management
1. Establishing Lactation
- Early initiation (within first hour after birth)
- Skin-to-skin contact
- Frequent feeding (8-12 times/24 hours)
- Proper latch and positioning
- Rooming-in to facilitate on-demand feeding
- Avoiding unnecessary supplementation
- Avoiding pacifiers and artificial nipples initially
2. Maintaining Lactation
- Frequent, effective milk removal
- Adequate rest and nutrition for mother
- Managing maternal health issues
- Education on milk expression techniques
- Support for working mothers
- Monitoring infant growth and development
- Addressing challenges promptly
3. Special Situations
- Premature infants
- Multiples (twins, triplets)
- Maternal illness or medication use
- Infant with special needs
- Relactation and induced lactation
- Weaning (when appropriate)
- Return to work planning
The First Week: Critical Period for Establishing Lactation
| Timeframe | Physiological Events | Management Strategies |
|---|---|---|
| First Hour (Golden Hour) | Infant alert and primed for first feeding; Colostrum available | Immediate skin-to-skin contact; Support for first latch; Delay routine procedures when possible |
| First 24 Hours | Colostrum feeds; Frequent infant wakening for feeds | 8+ feedings/24 hours; Rooming-in; Position and latch education; Hand expression instruction |
| Days 2-3 | Lactogenesis II beginning; Increased feeding frequency; Potential engorgement | Recognition of hunger cues; Ensuring effective milk transfer; Managing engorgement; Monitoring output |
| Days 4-5 | Milk volume increasing; Transitional milk; Potential nipple discomfort | Continued latch assessment; Nipple care; Monitoring infant weight; Addressing maternal concerns |
| Days 6-7 | Mature milk transitioning; Supply regulation beginning | Evaluating milk transfer; Addressing family support needs; Follow-up care planning |
Signs of Adequate Milk Transfer
Assessment of Infant
- Output: 6+ wet diapers/24 hours by day 5-7
- Stool: Transition from meconium to yellow, seedy stools by day 5; 3+ stools/24 hours
- Weight: Return to birth weight by 10-14 days; then gain of 20-30g/day
- Behavior: Alert when awake, satisfied after feeds
- Feeding: Audible swallowing during feeds; feeds 8-12 times/24 hours
- Physical: Good skin turgor, moist mucous membranes
Assessment of Mother
- Breasts: Softer after feeding; milk ejection sensation
- Nipples: No damage or persistent pain
- Comfort: Breastfeeding comfortable after initial latch
- Milk expression: Able to express milk if needed
- Perception: Mother feels infant is satisfied
Maternal Nutrition During Lactation
Nutritional Recommendations
- Caloric intake: Additional 450-500 kcal/day above pre-pregnancy needs
- Fluid intake: Minimum 2-3 liters/day; drink to thirst
- Protein: 65-75g/day (additional 15-20g above non-lactating needs)
- Calcium: 1000-1300 mg/day
- Vitamin D: 600 IU/day (supplementation often needed)
- DHA: 200-300 mg/day (from fatty fish or supplements)
- Iron: 9-10 mg/day
- Balanced diet: Emphasis on variety of whole foods
Note: Quality of breast milk is relatively preserved even with suboptimal maternal nutrition, but maternal health and energy may be affected.
Mnemonic: “BREAST” – Key Principles of Lactation Management
- B – Begin early (within first hour)
- R – Regular removal of milk (8-12 times/24 hours)
- E – Effective positioning and attachment
- A – Assessment of milk transfer (output, weight gain)
- S – Support for mother (physical, emotional, practical)
- T – Troubleshoot problems promptly
8. Challenges in Lactation and Solutions
Understanding common lactation challenges and their management is essential for healthcare providers supporting breastfeeding families.
| Challenge | Potential Causes | Management Strategies | Prevention |
|---|---|---|---|
| Sore Nipples | Poor latch, friction, infection, vasospasm, skin condition | Correct latch, express milk to start flow, apply breast milk or lanolin, moist wound healing, pain management | Proper positioning and latch from start, varied feeding positions, proper suction release |
| Engorgement | Milk coming in (normal physiological process), delayed/infrequent feeds, ineffective milk removal | Frequent feeding, cold compresses between feeds, gentle massage, reverse pressure softening, analgesics if needed | Early and frequent breastfeeding, ensuring effective milk removal, gentle hand expression if needed |
| Plugged Ducts | Inadequate milk drainage, pressure on ducts, restrictive clothing, sudden change in feeding pattern | Frequent feeding starting on affected side, varied positions, gentle massage toward nipple, warm compresses, NSAIDS for pain | Regular, complete breast emptying, avoid restrictive clothing/bras, varied feeding positions |
| Mastitis | Milk stasis, bacterial entry via cracked nipples, lowered maternal immunity | Continue breastfeeding, rest, fluids, analgesia, antibiotics if indicated (fever >101°F, symptoms >24h, or visible infection), probiotics | Prompt treatment of plugged ducts, proper latch, adequate milk removal, avoidance of breast trauma |
| Perceived Low Milk Supply | Normal variations in breast fullness, insufficient glandular tissue, infrequent feeding, ineffective milk removal, hormonal issues | Assessment of actual supply (weight gain, output), increase feeding frequency, breast compression, skin-to-skin contact, relaxation techniques | Early establishment of good feeding practices, education about normal feeding patterns and signs of adequate intake |
| Actual Low Milk Supply | Insufficient glandular tissue, retained placental fragments, prior breast surgery, hormonal disorders, medications, infrequent milk removal | Increase feeding/pumping frequency, optimize milk removal, galactogogues if indicated, supplementation with expressed milk/donor milk/formula if medically necessary | Early intervention for breastfeeding problems, recognition of risk factors, proactive management |
| Oversupply | Over-stimulation of breasts, excessive pumping, genetic predisposition | Block feeding (use one breast per feed or for block of time), laid-back positions, hand expression to comfort before feeds | Avoid excessive pumping, follow infant cues rather than scheduled expression |
| Infant with Poor Latch | Anatomical variations (tongue/lip tie, palatal issues), prematurity, neurological issues, prior bottle feeding | Positioning modifications, latch assistance techniques, referral for frenotomy if indicated, temporary alternative feeding methods | Early assessment of oral anatomy, skilled latch assistance, avoidance of unnecessary artificial nipples |
Special Considerations for Specific Populations
Preterm Infants
- Initiate milk expression within 6 hours of birth
- Focus on frequent expression (8+ times/24 hours)
- Utilize dual electric pumping with massage
- Provide kangaroo care when medically stable
- Support non-nutritive suckling at breast when appropriate
- Transition to direct breastfeeding based on developmental cues
- Consider supplementation with fortified breast milk as needed
Multiples (Twins, Triplets)
- Establish milk supply through frequent expression if needed
- Learn individual feeding techniques for each infant
- Develop effective simultaneous feeding positions
- Consider alternating breasts between infants for equal stimulation
- Create feeding logs if needed during early weeks
- Ensure adequate maternal nutrition and rest
- Mobilize practical support network
Red Flags Requiring Urgent Referral:
- For infant: Excessive weight loss (>10% of birth weight), jaundice requiring treatment, dehydration signs, failure to regain birth weight by 2 weeks
- For mother: Mastitis with significant systemic symptoms, breast abscess, severe persistent nipple pain, signs of postpartum depression affecting lactation
9. Baby Attachment and Effective Suckling
Proper attachment of the baby to the breast is fundamental for effective milk transfer, preventing nipple trauma, and maintaining milk production. Understanding the mechanics of infant suckling is essential for supporting optimal breastfeeding.
Signs of Good Attachment
External Signs
- More areola visible above baby’s top lip than below lower lip
- Mouth wide open (120-140° angle)
- Lower lip turned outward
- Chin touching or almost touching breast
- Cheeks appear full and rounded, not dimpled
- Rhythmic sucking with pauses
- Audible swallowing
What Happens Inside the Mouth
- Nipple drawn to back of mouth, near junction of hard/soft palate
- Breast tissue forms “teat” with nipple forming only 1/3 of teat
- Tongue extends over lower gum
- Tongue cups around breast in U-shape
- Peristaltic wave motion of tongue from front to back
- Jaw movement compresses milk sinuses
Signs of Poor Attachment
Observable Signs
- Equal amounts of areola visible above and below, or more below
- Mouth not open wide (narrow angle)
- Lower lip pointing forward or inward
- Chin away from breast
- Cheeks dimpling or sucking in
- Rapid, shallow sucking
- Clicking sounds during feeding
- Mother experiencing pain beyond initial latch
Consequences of Poor Attachment
- Inefficient milk transfer
- Nipple pain and trauma
- Inadequate breast emptying
- Risk of engorgement, plugged ducts, mastitis
- Reduced milk production over time
- Inadequate infant weight gain
- Maternal discouragement and early weaning
Positioning for Optimal Attachment
Key Principles for Any Position
- B.A.C.K. principles:
- Body aligned (ear, shoulder, hip in line)
- Attached properly (wide open mouth)
- Close to mother (no gaps between bodies)
- Keep chin touching breast
Mother’s Position
- Comfortable and well-supported (back, arms)
- No leaning or hunching over baby
- Relaxed shoulders and arms
- Able to maintain position for duration of feed
- Supports breast if needed (C-hold or U-hold)
Common Breastfeeding Positions
| Position | Description | Particularly Useful For |
|---|---|---|
| Cradle Hold | Baby’s head in crook of mother’s arm, bodies facing each other, baby’s lower arm around mother’s waist | Term infants with good head control; Most comfortable position once breastfeeding is established |
| Cross-cradle Hold | Baby’s head supported by hand opposite to feeding breast, bodies facing each other, controlled head support | Newborns; Learning to latch; Smaller babies; When more control of baby’s head is needed |
| Football/Clutch Hold | Baby tucked under mother’s arm on same side as feeding breast, legs extending behind mother, direct control of head positioning | Post-cesarean recovery; Large breasts; Twins; Preterm infants; When visualizing latch is important |
| Side-lying | Mother and baby lying on their sides facing each other, baby’s mouth level with nipple | Nighttime feeding; Post-cesarean recovery; When sitting is uncomfortable; Mothers with strong milk ejection |
| Laid-back/Biological Nurturing | Mother semi-reclined, baby prone on mother’s body, gravity helping attachment | Newborns with natural feeding reflexes; Oversupply/forceful let-down; Babies who gag/choke during feeding |
| Koala Hold | Baby sitting upright straddling mother’s thigh, facing breast | Older babies with good head control; Babies with reflux; Babies with tongue-tie/oral issues |
Infant Sucking Patterns
Early Feed Pattern
- Short, rapid sucks to stimulate let-down (no swallowing)
- Transition to slower, deeper sucking when milk begins to flow
- Sucking in bursts of 10-30 sucks with brief pauses
- Swallowing audible with milk transfer
- Suck-swallow ratio approximately 1:1 or 2:1 during active milk flow
Later Feed Pattern
- Slower sucking rate as feed progresses
- Longer pauses between bursts of sucking
- Suck-swallow ratio changes to approximately 3:1 or 4:1
- Less audible swallowing (but still present)
- May return to non-nutritive sucking at end of feed
- Baby typically releases breast spontaneously when satisfied
Mnemonic: “LATCH” – Assessing Effective Breastfeeding
- L – Lip turned outward
- A – Audible swallowing
- T – Type of sucking (deep, rhythmic)
- C – Comfort of mother (pain-free after initial latch)
- H – Hold/position (appropriate, supportive)
10. Best Practices in Lactation Support
Evidence-based practices for supporting lactation have evolved significantly over recent decades. Healthcare providers play a crucial role in implementing these practices.
Ten Steps to Successful Breastfeeding
The WHO/UNICEF Baby-Friendly Hospital Initiative framework:
Hospital Policies and Staff Education
- Maintain a written breastfeeding policy routinely communicated to staff
- Train all healthcare staff in skills necessary to implement the policy
- Inform all pregnant women about benefits and management of breastfeeding
Clinical Practices
- Help mothers initiate breastfeeding within one hour of birth
- Show mothers how to breastfeed and maintain lactation even if separated
- Give infants no food or drink other than breast milk unless medically indicated
- Practice rooming-in (allow mothers and babies to remain together 24 hours/day)
- Encourage breastfeeding on demand
- Give no artificial nipples or pacifiers to breastfeeding infants
- Foster the establishment of breastfeeding support groups and refer mothers to them
Evidence-Based Lactation Support Interventions
| Intervention | Description | Evidence of Effectiveness |
|---|---|---|
| Skin-to-skin contact | Direct skin-to-skin positioning of newborn on mother’s chest immediately after birth and continued regularly | Increases duration of exclusive breastfeeding; Improves infant temperature regulation; Facilitates successful first latch; Reduces infant stress response to painful procedures |
| Early initiation | Supporting breastfeeding within first hour after birth | Associated with longer breastfeeding duration; Reduced infant mortality; Earlier establishment of milk production |
| Rooming-in | Mother and baby remain together 24 hours/day | Facilitates feeding on cue; Increases milk production; Improves mother’s confidence; Enhances bonding |
| Feeding on cue | Responding to infant feeding cues rather than scheduled feeds | Better milk transfer; Reduced engorgement; Improved maternal comfort; Better weight gain; Longer breastfeeding duration |
| Hands-on teaching | Practical assistance with positioning and attachment | Reduces nipple trauma; Improves milk transfer; Increases maternal confidence; Resolves early difficulties |
| Professional support | Access to skilled lactation professionals during hospital stay and after discharge | Increases exclusive breastfeeding rates; Longer breastfeeding duration; Early identification and resolution of problems |
| Peer support | Connection with experienced breastfeeding mothers or peer counselors | Particularly effective in communities where breastfeeding is not the norm; Provides practical and emotional support |
Role of the Nurse in Lactation Support
Assessment
- Evaluate maternal history for risk factors
- Assess breast anatomy and infant oral anatomy
- Observe breastfeeding sessions
- Monitor infant output and weight
- Evaluate maternal comfort and concerns
- Identify early signs of complications
- Assess family support systems
Intervention
- Provide evidence-based information
- Demonstrate positioning techniques
- Assist with latch optimization
- Teach milk expression methods
- Provide anticipatory guidance
- Implement comfort measures
- Support maternal confidence
- Facilitate skin-to-skin contact
Referral and Follow-up
- Identify need for specialized help
- Refer to lactation consultants when needed
- Connect with community resources
- Ensure continuity of care after discharge
- Schedule appropriate follow-up
- Document breastfeeding progress
- Communicate between healthcare team members
Global Best Practices in Lactation Support
Innovative Global Approaches
- Kangaroo Mother Care (Colombia & globally): Continuous skin-to-skin contact for premature infants, originally developed in Colombia, now widely implemented globally as a standard of care for preterm infants.
- Community Doulas (Brazil & United States): Trained community members providing in-home breastfeeding support, particularly effective in marginalized communities.
- Baby-Friendly Communities (Norway): Extending Baby-Friendly principles beyond hospitals to entire communities, contributing to Norway’s high breastfeeding rates.
- Mobile Health Support (India & Africa): Text message and smartphone app-based lactation support systems reaching mothers in remote areas.
- Breast Milk Banks (Brazil): World’s largest network of human milk banks, providing safe donor milk to vulnerable infants.
- Workplace Support (Sweden & Nordic countries): Comprehensive parental leave policies and workplace accommodations supporting continued breastfeeding.
- Peer Counselor Programs (Bangladesh): Community-based peer support systems that have significantly increased exclusive breastfeeding rates.
The Future of Lactation Support:
Emerging trends in lactation support include:
- Telehealth lactation consultations improving access to expert support
- Integration of lactation care into regular primary healthcare
- Enhanced lactation education in healthcare professional curricula
- Digital technologies for monitoring and supporting breastfeeding
- Greater emphasis on family-centered approaches including partner support
- Focus on addressing disparities in breastfeeding rates and support
11. References
- Lawrence, R. A., & Lawrence, R. M. (2016). Breastfeeding: A guide for the medical profession (8th ed.). Philadelphia, PA: Elsevier.
- World Health Organization. (2018). Implementation guidance: protecting, promoting and supporting breastfeeding in facilities providing maternity and newborn services – the revised Baby-friendly Hospital Initiative.
- Academy of Breastfeeding Medicine. (2021). Clinical protocols. Available at: https://www.bfmed.org/protocols
- Riordan, J., & Wambach, K. (2014). Breastfeeding and human lactation (5th ed.). Burlington, MA: Jones & Bartlett Learning.
- Walker, M. (2017). Breastfeeding management for the clinician: Using the evidence (4th ed.). Burlington, MA: Jones & Bartlett Learning.
- American Academy of Pediatrics. (2022). Breastfeeding and the use of human milk. Pediatrics, 129(3), e827-e841.
- Kent, J. C., Prime, D. K., & Garbin, C. P. (2012). Principles for maintaining or increasing breast milk production. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 41(1), 114-121.
- Neville, M. C., & Morton, J. (2001). Physiology and endocrine changes underlying human lactogenesis II. The Journal of Nutrition, 131(11), 3005S-3008S.
- Ballard, O., & Morrow, A. L. (2013). Human milk composition: nutrients and bioactive factors. Pediatric Clinics of North America, 60(1), 49-74.
- Geddes, D., & Perrella, S. (2019). Breastfeeding and human lactation. Nutrients, 11(4), 802.
