Placental Function: Blood-Brain Barrier
Comprehensive Study Notes for Nursing Students
Table of Contents
1. Introduction to Protective Barriers
The human body contains several specialized that protect vital tissues from harmful substances while allowing essential molecules to pass through. Among these, the placental barrier and blood-brain barrier (BBB) represent two of the most critical protective interfaces in human physiology.
These barriers share the fundamental purpose of maintaining homeostasis and protecting vulnerable tissues—the developing fetus and the central nervous system, respectively—but they differ significantly in structure, development, and specific mechanisms.
Key Concept
Both the placental barrier and blood-brain barrier serve as selective semi-permeable membranes that regulate the exchange of substances between two distinct environments, providing crucial that maintain optimal conditions for their respective protected tissues.
2. Placental Barrier
2.1 Structure and Development
The placenta forms after implantation of the blastocyst and develops into a complex organ that connects the developing fetus to the maternal uterine wall. The of the placenta is formed by multiple layers of tissue separating maternal and fetal blood.
Components of the Placental Barrier:
- Syncytiotrophoblast – Multinucleated outer layer in direct contact with maternal blood
- Cytotrophoblast – Single-celled inner layer (becomes discontinuous later in pregnancy)
- Basement Membrane – Supporting structure beneath the trophoblast layers
- Connective Tissue – Contains Wharton’s jelly in the chorionic villi
- Fetal Capillary Endothelium – Inner lining of fetal blood vessels
Important Note
The placental barrier’s thickness and permeability change throughout pregnancy. During the first trimester, the barrier is thicker with a complete cytotrophoblast layer, providing maximum protection during critical fetal organ development. As pregnancy progresses, the barrier becomes thinner, allowing for increased nutrient transfer to support fetal growth.
2.2 Functions and Mechanisms
The placental provides several critical roles in fetal development and protection:
Protection
- Shields fetus from potentially harmful substances in maternal blood
- Filters out many pathogens and toxins
- Employs specialized transporters for protective efflux
- Contains immunological defenses
Nutrient Transfer
- Facilitates transfer of oxygen and nutrients
- Provides glucose via GLUT transporters
- Transfers amino acids, fatty acids, vitamins, and minerals
- Uptake increases as fetal demands grow
Waste Elimination
- Removes carbon dioxide and metabolic waste
- Transfers urea and other nitrogenous waste
- Prevents toxic accumulation in fetal circulation
Endocrine Function
- Produces hormones essential for pregnancy maintenance
- Secretes human chorionic gonadotropin (hCG)
- Produces estrogen, progesterone, and human placental lactogen
- Regulates maternal-fetal metabolic adaptations
The of the placenta is not absolute. While it effectively blocks many harmful substances, others can cross the barrier depending on their molecular properties:
| Substance Properties | Barrier Permeability | Examples |
|---|---|---|
| Lipophilic, small molecules | Easily crosses | Alcohol, nicotine, some medications |
| Hydrophilic, small molecules | Limited crossing via transporters | Glucose, amino acids, electrolytes |
| Large molecules | Highly restricted | Proteins, most antibodies |
| Most pathogens | Blocked (with exceptions) | Most bacteria (exceptions: Listeria, some viruses) |
3. Blood-Brain Barrier
3.1 Structure and Development
The blood-brain barrier (BBB) is a selective semi-permeable membrane between blood and brain interstitial fluid that provides a crucial protecting the central nervous system (CNS).
Components of the Blood-Brain Barrier:
- Brain Microvascular Endothelial Cells – Non-fenestrated endothelium with tight junctions
- Tight Junctions – Highly specialized junctional complexes between endothelial cells that restrict paracellular transport
- Basement Membrane – Supporting extracellular matrix structure
- Pericytes – Embedded in basement membrane, involved in vascular stability and BBB maintenance
- Astrocyte End-Feet – Surround the capillaries and help maintain BBB integrity
Development of the BBB:
Angiogenesis
Early gestation during neural tube development. Formation of new blood vessels guided by VEGF signals.
Differentiation
Recruitment of pericytes and astrocytes to the newly formed vessels. Induction of tight junctions.
Maturation
Stabilization and maintenance of the neurovascular unit. Complete formation by third trimester.
Development Fact
Contrary to previous beliefs, the BBB is not absent in the developing fetus. Recent research shows that it is functional very early in development, with many of the barrier properties already present from early gestational time points in humans, rats, and sheep.
3.2 Functions and Mechanisms
The of the BBB is critical for maintaining the specialized environment required for proper neuronal function. It serves several vital purposes:
Protection
- Shields the brain from circulating toxins and pathogens
- Prevents entry of most blood-borne substances
- Protects from fluctuations in plasma composition
- Restricts entry of immune cells and antibodies
Nutrient Supply
- Facilitates selective transport of essential nutrients
- Provides glucose via GLUT1 transporters
- Transports amino acids and other essential molecules
- Regulates ion balance for neuronal function
Waste Removal
- Removes metabolic waste products
- Clears potential neurotoxins
- Helps regulate brain interstitial fluid composition
Homeostasis
- Maintains stable neuronal environment
- Regulates ion concentrations
- Controls cerebral blood flow
- Helps maintain proper pH for neuronal function
The BBB’s relies heavily on specialized transport mechanisms to regulate what enters and exits the brain:
| Transport System | Function | Examples |
|---|---|---|
| Passive Diffusion | Small lipophilic molecules cross freely | O₂, CO₂, alcohol, steroid hormones |
| Carrier-Mediated Transport | Facilitates entry of essential nutrients | Glucose (GLUT1), amino acids, nucleosides |
| Efflux Transport | Pumps potentially harmful substances out of brain | P-glycoprotein (P-gp), BCRP, MRPs |
| Receptor-Mediated Transcytosis | Transports large molecules across BBB | Insulin, transferrin, leptin |
| Adsorptive-Mediated Transcytosis | Transports cationic proteins | Albumin, histones |
Clinical Note
The BBB poses a significant challenge in drug delivery to the CNS. It is estimated that more than 90% of small-molecule drugs and nearly 100% of large-molecule therapeutics cannot effectively cross the BBB, making CNS disorders particularly difficult to treat pharmacologically.
4. Comparative Analysis of Barrier Functions
While both the placental barrier and the blood-brain barrier serve as crucial protective interfaces, they have important similarities and differences in their :
| Characteristic | Placental Barrier | Blood-Brain Barrier |
|---|---|---|
| Primary Function | Regulates exchange between maternal and fetal circulation | Regulates exchange between blood and brain interstitial fluid |
| Development Timeline | Forms after implantation of the blastocyst | Develops early in gestation during neural tube formation |
| Structural Changes | Becomes thinner and more permeable as pregnancy progresses | Maintains consistent structure throughout life |
| Key Cellular Components | Syncytiotrophoblast, cytotrophoblast, basement membrane, fetal endothelium | Brain endothelial cells with tight junctions, pericytes, astrocyte end-feet |
| Primary Protective Mechanism | Physical barrier + active transport systems | Tight junctions + active transport systems |
| Permeability to Water-Soluble Substances | Moderately restrictive | Highly restrictive |
| Presence of Tight Junctions | Present but less extensive | Extensive and highly complex |
| Longevity | Temporary (duration of pregnancy) | Permanent throughout life |
| Major Transporters | P-gp, BCRP, MRP1, OATP2B1, OATP4A1, OCT3, OAT4 | P-gp, BCRP, GLUT1, MCT1, LAT1, various SLCs |
Integrated Function
During fetal development, both barriers work in concert to protect the developing brain. The placenta provides the first line of defense against maternal blood-borne toxins, while the fetal BBB provides a second layer of protection specific to the developing CNS. This dual system is essential for proper neurodevelopment.
5. Clinical Applications
Understanding the of the placenta and BBB has important clinical implications for nursing practice:
Placental Barrier Applications
- Medication Administration During Pregnancy: Knowledge of which drugs cross the placental barrier is crucial for safe medication practices during pregnancy.
- Fetal Monitoring: Understanding normal placental function helps in interpreting fetal assessment findings.
- Pregnancy Complications: Recognition of conditions that compromise placental barrier integrity (preeclampsia, placental insufficiency).
- Patient Education: Providing evidence-based information about substances that cross the placenta (alcohol, tobacco, medications).
- Vaccination: Understanding which maternal antibodies cross the placenta to provide passive immunity to the newborn.
Blood-Brain Barrier Applications
- Neurological Medications: Knowledge of which drugs can penetrate the BBB affects nursing administration and monitoring practices.
- CNS Infections: Understanding compromised BBB function during meningitis, encephalitis, and other infections.
- Neurodegenerative Disorders: Awareness of BBB dysfunction in conditions like Alzheimer’s and multiple sclerosis.
- Traumatic Brain Injury: Recognition of increased BBB permeability after head trauma and implications for secondary injury.
- Neonatal Care: Special consideration for drugs administered to neonates, especially premature infants with immature BBB function.
Nursing Alert
When caring for pregnant women receiving medications, always consult current drug references regarding placental barrier crossing. Similarly, when administering medications to patients with neurological conditions, verify whether the drug can effectively cross the BBB to reach therapeutic concentrations in the CNS.
6. Mnemonics for Learning
Memorizing the components and functions of these complex can be challenging. Use these mnemonics to help remember key concepts:
Placental Barrier: “PLACE”
- P – Protection from toxins and pathogens
- L – Lipophilic substances can cross easily
- A – Active transport of nutrients to fetus
- C – Change in thickness during gestation
- E – Endocrine functions (hormone production)
BBB Components: “TAPPS”
- T – Tight junctions between endothelial cells
- A – Astrocyte end-feet surround vessels
- P – Pericytes embedded in basement membrane
- P – Protein transporters (influx and efflux)
- S – Specialized endothelial cells (non-fenestrated)
What Crosses Both Barriers: “SLOPE”
BBB Transport Mechanisms: “PEARL”
7. Pathological Conditions Affecting Barrier Functions
Several pathological conditions can compromise the integrity and of both the placental barrier and BBB:
Placental Barrier Disruptions
| Condition | Effect on Barrier | Clinical Implications |
|---|---|---|
| Preeclampsia | Altered transporter expression and function | Compromised fetal development, increased risk of toxin exposure |
| Placental Insufficiency | Reduced exchange capacity | Intrauterine growth restriction (IUGR), hypoxia |
| Chorioamnionitis | Inflammatory changes in barrier | Increased risk of fetal infection, preterm labor |
| Gestational Diabetes | Altered nutrient transfer dynamics | Fetal macrosomia, metabolic disturbances |
| Viral Infections | Some viruses can cross the barrier | Congenital infections (TORCH infections) |
BBB Disruptions
| Condition | Effect on Barrier | Clinical Implications |
|---|---|---|
| Traumatic Brain Injury | Physical disruption of barrier integrity | Cerebral edema, inflammation, secondary injury |
| Multiple Sclerosis | Inflammation and BBB breakdown | Leukocyte infiltration, demyelination |
| Alzheimer’s Disease | Reduced P-gp function, tight junction damage | Amyloid-beta accumulation, neuroinflammation |
| Meningitis/Encephalitis | Pathogen-induced breakdown | CNS infection, increased ICP, neurological deficits |
| Stroke | Ischemia-induced disruption | Vasogenic edema, hemorrhagic transformation |
Clinical Connection
In both barriers, disruption often involves alteration in tight junction proteins, changes in transporter expression, and inflammatory responses. Recognizing the signs of barrier compromise is crucial for early intervention and prevention of serious complications.
8. Transport Mechanisms Across Barriers
Both the placental barrier and BBB employ specialized transport mechanisms to maintain their while allowing essential substances to cross:
Key Transport Protein Families:
ABC Transporters
ATP-binding cassette transporters that primarily function in efflux/protective capacity.
- P-glycoprotein (P-gp/ABCB1): Exports xenobiotics
- BCRP (ABCG2): Breast cancer resistance protein
- MRPs (ABCC family): Multidrug resistance proteins
SLC Transporters
Solute carrier family proteins that facilitate influx of essential nutrients.
- GLUT1 (SLC2A1): Glucose transport
- LAT1 (SLC7A5): Large neutral amino acids
- MCT1 (SLC16A1): Monocarboxylates, lactate
Receptor-Mediated Systems
Transport large molecules via vesicular trafficking.
- Transferrin receptor: Iron transport
- Insulin receptor: Insulin transport
- LDL receptor-related proteins
Factors Influencing Transport Across Barriers:
Molecular Properties
- Lipophilicity: Increases passive diffusion
- Molecular Weight: Smaller molecules cross more easily
- Charge: Affects interaction with transporters
- Protein Binding: Bound substances typically cannot cross
- Ionization: Nonionized forms cross more readily
Physiological/Pathological Factors
- Blood Flow: Affects delivery to barrier
- Inflammation: Can increase permeability
- Development: Gestational age affects barrier maturity
- Disease States: Can compromise barrier integrity
- Genetics: Polymorphisms in transporters
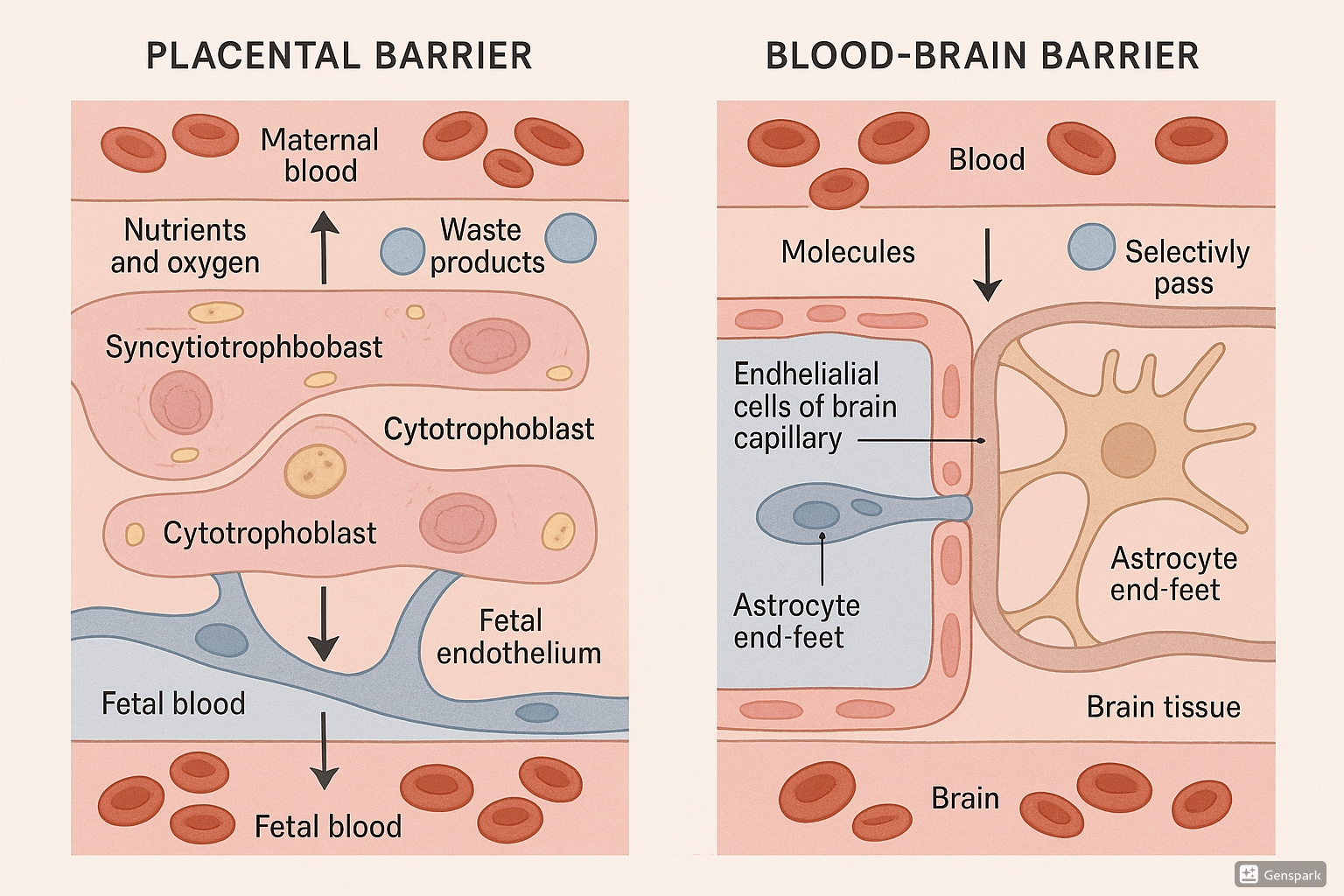
9. Visual Comparison of Barriers
The following illustration compares the structure and of the placental barrier and blood-brain barrier:
Key Visual Takeaways
Note the key structural differences: the placental barrier consists of syncytiotrophoblast, cytotrophoblast, basement membrane, and fetal endothelium separating maternal and fetal circulation. The BBB features specialized endothelial cells with tight junctions, surrounded by pericytes and astrocyte end-feet. Both barriers employ similar transporter systems but in different cellular contexts to maintain their protective .
10. References
- Saunders, N. R., Dziegielewska, K. M., Møllgård, K., & Habgood, M. D. (2016). Review: The blood-brain barrier; protecting the developing fetal brain. Placenta, 48, S103-S109.
- Dotiwala A, McCausland C, & Samra N. (2023). Anatomy, Head and Neck: Blood Brain Barrier. In: StatPearls. Treasure Island (FL): StatPearls Publishing.
- van der Velpen, V., Teutonico, A., Tomczak, S., et al. (2022). Transporter Regulation in Critical Protective Barriers: Focus on Brain and Placenta. Pharmaceutics, 14(7), 1519.
- Ballabh, P., Braun, A., & Nedergaard, M. (2004). The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiology of Disease, 16(1), 1-13.
- Gude, N. M., Roberts, C. T., Kalionis, B., & King, R. G. (2004). Growth and function of the normal human placenta. Thrombosis Research, 114(5-6), 397-407.
- Abbott, N. J., Patabendige, A. A., Dolman, D. E., et al. (2010). Structure and function of the blood-brain barrier. Neurobiology of Disease, 37(1), 13-25.
- Nishimura, M., & Naito, S. (2005). Tissue-specific mRNA expression profiles of human ATP-binding cassette and solute carrier transporter superfamilies. Drug Metabolism and Pharmacokinetics, 20(6), 452-477.
- Pardridge, W. M. (2012). Drug transport across the blood-brain barrier. Journal of Cerebral Blood Flow & Metabolism, 32(11), 1959-1972.
