
Planning Nursing Services
A comprehensive guide for nursing students
Table of Contents
Introduction to Planning Nursing Services
Planning in nursing services is the systematic process that establishes a roadmap for delivering high-quality patient care. Effective planning ensures that nursing resources are allocated efficiently, staff members understand their roles and responsibilities, and patient outcomes are optimized.
Key Concept
Planning in nursing services operates at multiple levels: strategic (long-term vision), tactical (policies and procedures), and operational (day-to-day implementation). Each level interconnects to create a comprehensive approach to healthcare delivery.

Vision & Mission in Nursing
Vision
A nursing vision statement articulates the aspirational future state that the nursing department strives to achieve. It serves as an inspirational guidepost that motivates staff and informs strategic decision-making.
Characteristics of Effective Vision Statements:
- Future-oriented and aspirational
- Clear, concise, and memorable
- Aligned with organizational goals
- Inspiring to all stakeholders
- Realistic yet challenging
Example:
“To be leaders in advancing exemplary professional nursing practice by providing compassionate and quality patient care while setting new standards for innovation and excellence.”
Mission
A nursing mission statement defines the purpose of the nursing department and outlines its core functions, values, and commitment to patients and the community.
Characteristics of Effective Mission Statements:
- Defines core purpose and functions
- Specifies key stakeholders
- Reflects organizational values
- Outlines services provided
- Explains what makes the nursing service unique
Example:
“To provide science-based, technologically precise, compassionately delivered nursing care; to advocate for patients and families; and to advance nursing knowledge through education and research.”
Vision-Mission Integration

Mnemonic: “CRAFT” for Vision-Mission Development
- Clear and Concise language
- Relevant to all stakeholders
- Aligned with organizational values
- Future-oriented outlook
- Tangible enough to guide action
Nursing Philosophy
A nursing philosophy articulates the fundamental beliefs, values, and principles that guide nursing practice within an organization. It serves as the foundation for decision-making, standards of care, and professional conduct.
Core Components
- Beliefs about nursing: The essence and purpose of the nursing profession
- Beliefs about patients: Views on patient autonomy, dignity, and rights
- Beliefs about healthcare: Stance on access, quality, and delivery of healthcare
- Ethical principles: Fundamental moral guidelines for practice
- Professional values: Core values that define nursing excellence
Development Process
- Engage nursing staff at all levels
- Review professional standards and literature
- Identify shared beliefs and values
- Draft a cohesive statement
- Regularly review and update as the profession evolves

Sample Philosophy Statement
“We believe that nursing is both an art and a science that provides holistic, patient-centered care. Our practice is built on evidence-based approaches while honoring the uniqueness of each individual. We respect the dignity, autonomy, and cultural diversity of all patients and their families. We are committed to continuous learning, interprofessional collaboration, and ethical practice to achieve optimal patient outcomes and advance the nursing profession.”
Connection Between Philosophy, Mission, and Vision
The nursing philosophy forms the foundation that informs the mission (what we do now) and vision (what we aspire to become). Together, they create a coherent framework that guides all nursing activities and decision-making within the organization.
Setting Nursing Objectives
Nursing objectives are specific, measurable goals that translate the vision, mission, and philosophy into actionable targets. Well-defined objectives provide direction and benchmarks for evaluating nursing services.
The SMART Framework
Effective nursing objectives follow the SMART criteria:
S
Specific
Clearly define what you aim to accomplish
M
Measurable
Include metrics to track progress
A
Achievable
Realistic given available resources
R
Relevant
Aligned with nursing mission and values
T
Time-bound
Set deadlines for completion
Example of SMART Objectives:
- Not SMART: “Improve patient satisfaction”
- SMART: “Increase patient satisfaction scores in the medical-surgical unit from 85% to 92% within six months by implementing hourly nursing rounds and post-discharge follow-up calls.”
Types of Nursing Objectives
| Type | Focus Area | Example |
|---|---|---|
| Clinical Care | Direct patient care quality | “Reduce hospital-acquired pressure ulcers by 30% within one year through implementation of a comprehensive skin assessment protocol.” |
| Professional Development | Staff growth and competency | “Increase the percentage of BSN-prepared nurses from 70% to 85% within three years through tuition support and flexible scheduling.” |
| Operational | Efficiency and resource utilization | “Reduce nurse overtime by 15% within six months by implementing an optimized staff scheduling system.” |
| Patient Experience | Patient satisfaction and engagement | “Achieve top-quartile patient satisfaction scores across all nursing units by the end of the fiscal year through enhanced communication training.” |
| Quality Improvement | Clinical outcomes and safety | “Decrease medication administration errors by 25% within 12 months by implementing barcode medication verification technology.” |
Mnemonic: “SCOPE” for Objectives Hierarchy
Remember the hierarchy of nursing objectives with “SCOPE”:
- Strategic objectives (long-term, organizational)
- Comparative objectives (benchmarking against standards)
- Operational objectives (day-to-day functioning)
- Professional objectives (staff development)
- Evaluation objectives (quality assessment)
Nursing Service Policies
Nursing service policies are formal statements that guide nursing practice within an organization. They establish standards, ensure consistency, promote quality care, and help achieve compliance with regulatory requirements.
Components of Effective Policies
- Policy title: Clear identification of the policy focus
- Policy number: Unique identifier for reference
- Purpose: Why the policy exists
- Scope: Who and what the policy applies to
- Definitions: Clarification of key terms
- Policy statement: The directive or rule being established
- Responsibilities: Who is accountable for implementation
- References: Evidence base and standards
- Approval/review details: Dates and authorizing bodies
Types of Nursing Policies
Administrative Policies
Cover organizational structure, staffing, scheduling, reporting relationships, and general operations.
Clinical Policies
Address direct patient care practices, clinical procedures, and evidence-based protocols.
Regulatory Policies
Ensure compliance with external requirements from accrediting bodies, government agencies, and legal mandates.
Personnel Policies
Cover staff management, professional development, competency requirements, and performance evaluation.
Safety and Quality Policies
Focus on risk management, patient safety, quality improvement, and adverse event reporting.
Policy Development Cycle
1. Identify Need
Recognize gaps or issues requiring policy guidance based on practice trends, incidents, or regulatory changes
2. Research
Gather evidence-based information, best practices, regulatory requirements, and stakeholder input
3. Draft
Create an initial policy document addressing the identified need, following organizational template
4. Review
Circulate draft to stakeholders for feedback (nursing leadership, staff, quality department, legal counsel)
5. Approve
Obtain formal approval from appropriate authority (nursing practice council, CNO, hospital administration)
6. Implement
Distribute, educate staff, and integrate into practice
7. Evaluate
Monitor policy effectiveness, compliance, and outcomes
8. Review & Revise
Periodically review and update as needed (typically every 1-3 years)
Mnemonic: “POLICIES” for Effective Policy Development
- Purpose – Clearly define why the policy exists
- Ownership – Identify who is responsible for the policy
- Legal compliance – Ensure alignment with laws and regulations
- Input from stakeholders – Gather feedback from affected parties
- Clarity in language – Use precise, unambiguous wording
- Implementation plan – Develop strategy for rollout
- Education of staff – Train those affected by the policy
- Systematic review – Schedule regular evaluations
Procedures & Manuals
Nursing Procedures
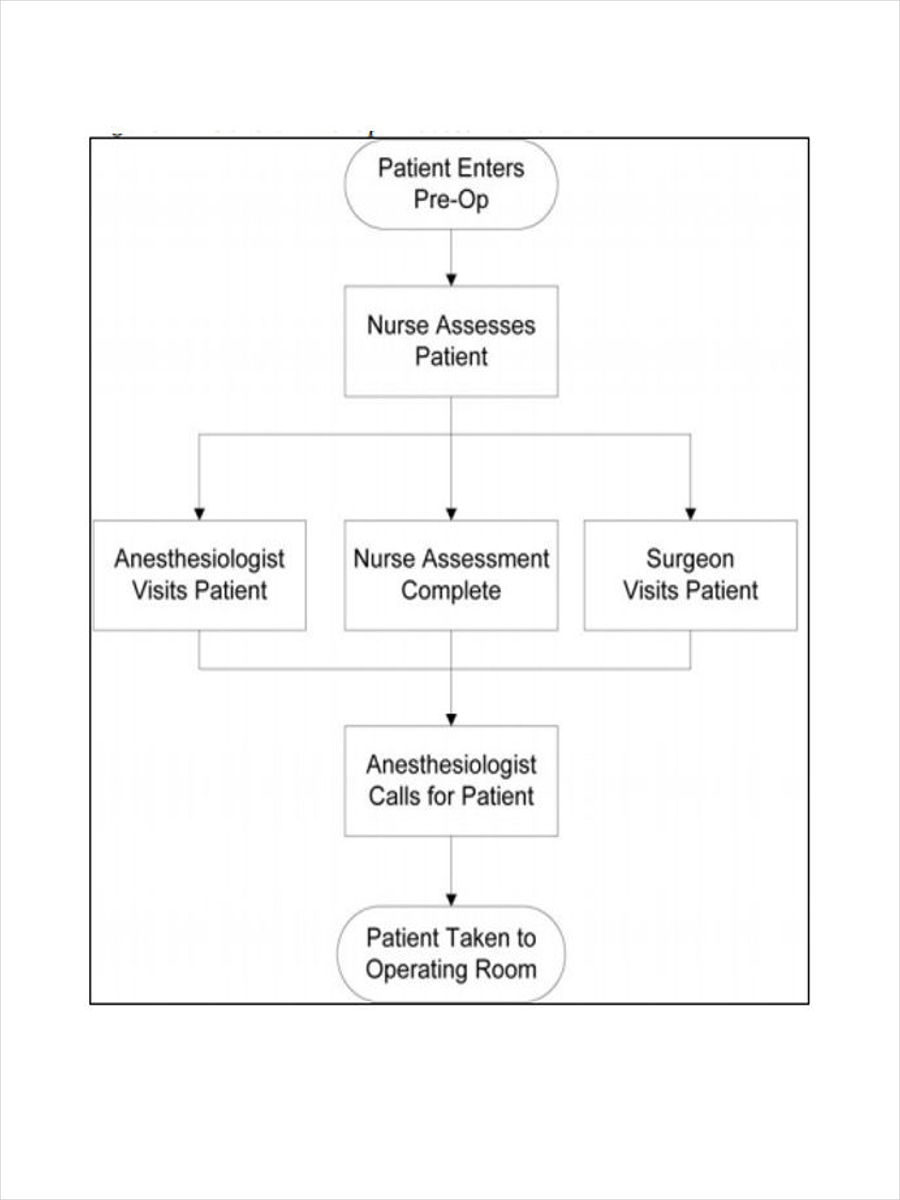
Nursing procedures are detailed, step-by-step instructions for performing specific nursing tasks or activities. They translate policies into actionable processes that guide daily practice.
Characteristics of Well-Written Procedures:
- Sequential steps in logical order
- Clear, concise language
- Evidence-based practices
- Safety considerations highlighted
- Required equipment and resources listed
- Expected outcomes defined
Procedure Components:
- Title and identifier
- Purpose and scope
- Equipment/supplies needed
- Pre-procedure preparations
- Step-by-step instructions
- Post-procedure activities
- Documentation requirements
- References and related documents
Nursing Manuals
Nursing manuals are comprehensive reference documents that organize policies, procedures, and other important information for nursing staff. They serve as official guides for nursing practice within an organization.
Types of Nursing Manuals:
- Administrative Manuals: Organizational structure, leadership roles, reporting relationships
- Clinical Procedure Manuals: Step-by-step instructions for clinical procedures
- Policy and Procedure Manuals: Combined reference for policies and related procedures
- Orientation Manuals: Materials for onboarding new nursing staff
- Equipment Manuals: Operating instructions for nursing equipment and technology
Effective Manual Organization:
- Logical arrangement of content (by department, specialty, or function)
- Comprehensive table of contents
- Clear index for quick reference
- Consistent formatting throughout
- Version control and review dates
Understanding the Difference: Policies vs. Procedures
| Aspect | Policies | Procedures |
|---|---|---|
| Focus | The “what” and “why” – guiding principles | The “how” – specific steps to follow |
| Scope | Broad, high-level direction | Detailed, task-specific instructions |
| Format | Declarative statements of intent or rules | Sequential, step-by-step instructions |
| Flexibility | Less detailed, allowing some interpretation | Highly specific with little room for variation |
| Approval Level | Higher-level approval (board, executive) | Department or director-level approval |
| Example | “All patients will be assessed for fall risk upon admission and every shift.” | “To conduct a fall risk assessment: 1. Gather the Morse Fall Scale tool, 2. Interview patient about fall history…” |

Mnemonic: “MANUAL” for Effective Nursing Manuals
- Manageable size and organization
- Accessible to all nursing staff
- Navigable with clear indexing
- Updated regularly
- Accurate and evidence-based
- Legally compliant content
Functional & Operational Planning
Functional and operational planning focuses on the day-to-day management and implementation of nursing services. It translates strategic goals into concrete actions and resource allocations to ensure efficient care delivery.
Functional Planning
Functional planning addresses the organization and structuring of nursing units and services to achieve optimal efficiency and effectiveness. It focuses on how nursing functions are arranged and coordinated.
Key Components:
- Organizational Structure: Reporting relationships, department divisions
- Staffing Models: Team nursing, primary nursing, functional nursing
- Role Delineation: Defining responsibilities for different nursing positions
- Workflow Design: Process mapping for efficient patient care delivery
- Space Utilization: Physical layout of nursing units and work areas
Nursing Care Delivery Models:
- Team Nursing: Groups of nurses with varied skills providing care under team leader
- Primary Nursing: One nurse responsible for total care of assigned patients
- Functional Nursing: Task-oriented approach where nurses specialize in specific functions
- Patient-Centered Care: Focus on individualized care planning with patient involvement
Operational Planning
Operational planning focuses on the tactical aspects of implementing nursing services on a daily basis. It addresses resource allocation, scheduling, and management of ongoing activities.
Key Components:
- Staffing Plans: Nurse-to-patient ratios, shift assignments, skill mix
- Scheduling: Work rotation patterns, shift coverage, leave management
- Resource Allocation: Equipment, supplies, technology distribution
- Budget Management: Cost control, resource utilization
- Daily Operations: Patient assignments, handoffs, workflow management
Operational Planning Cycle:
- Assess current operational performance
- Identify areas for improvement
- Set operational targets and metrics
- Develop action plans
- Allocate resources
- Implement operational changes
- Monitor and adjust as needed
Operational Planning Tools
Daily Management Tools
- Daily staffing matrices
- Patient acuity measurement tools
- Assignment boards
- Bed management systems
- Shift handoff templates
Periodic Planning Tools
- Staff scheduling software
- Productivity dashboards
- Budget variance reports
- Quality indicators tracking
- Resource utilization reports
Mnemonic: “OPERATE” for Operational Excellence
- Organize workflows logically
- Prioritize patient needs
- Evaluate resource utilization
- Respond flexibly to changing demands
- Allocate staff based on acuity
- Track performance metrics
- Ensure continuous improvement
Strategic Planning
Strategic planning is a systematic process of defining nursing’s long-term direction, setting priorities, and making decisions on resource allocation to pursue this direction. It provides a roadmap for nursing services over a 3-5 year horizon.
Strategic Planning Process
1. Environmental Assessment
Analyze internal and external factors affecting nursing services (SWOT analysis, market trends, regulatory landscape)
2. Vision and Mission Review
Confirm or refine nursing vision and mission to ensure alignment with organizational direction
3. Strategic Goal Setting
Identify 3-5 key strategic priorities that will guide nursing services over the planning period
4. Strategy Development
Develop specific strategies and initiatives to achieve each strategic goal
5. Resource Allocation
Determine human, financial, and technological resources needed to implement strategies
6. Implementation Planning
Create detailed action plans with timelines, responsibilities, and metrics
7. Monitoring Framework
Establish mechanisms to track progress, measure outcomes, and adjust strategies as needed
8. Evaluation and Revision
Regularly review progress, adjust strategies, and update the plan based on outcomes and changing conditions
SWOT Analysis in Nursing Strategic Planning
Strengths
- Highly skilled nursing staff
- Strong leadership team
- Excellent patient satisfaction scores
- Robust professional development programs
- Effective interdisciplinary collaboration
Weaknesses
- Nursing staff turnover rates
- Inconsistent adherence to protocols
- Limited advanced technology adoption
- Documentation inefficiencies
- Budget constraints
Opportunities
- New care delivery models
- Telehealth expansion
- Community partnership development
- Grant funding for innovation
- Academic partnerships
Threats
- Nursing shortage
- Regulatory changes
- Competing healthcare facilities
- Financial reimbursement challenges
- Changing patient demographics
Components of a Nursing Strategic Plan
Core Elements
- Executive Summary: Overview of plan highlights
- Environmental Analysis: Internal/external assessment findings
- Vision, Mission, Values: Guiding principles
- Strategic Priorities: Key focus areas
- Goals and Objectives: Measurable targets
- Action Plans: Specific implementation strategies
- Resource Requirements: Needed personnel, budget, technologies
- Timeline: Implementation schedule
- Evaluation Plan: How success will be measured
Common Strategic Focus Areas
- Care Quality and Safety: Improving patient outcomes
- Workforce Development: Recruitment, retention, advancement
- Professional Practice: Care model innovation, evidence-based practice
- Technology Integration: EHR optimization, digital solutions
- Patient Experience: Satisfaction, engagement, service excellence
- Operational Excellence: Efficiency, resource management
- Academic Partnerships: Research, education collaboration
- Leadership Development: Succession planning, mentoring

Mnemonic: “STRATEGIC” for Effective Planning
- Scan the environment (internal and external)
- Target key priorities based on assessment
- Review vision, mission, and values
- Align goals with organizational direction
- Tailor strategies to specific contexts
- Engage stakeholders throughout the process
- Generate measurable objectives
- Implement with clear accountability
- Continuously evaluate and adapt
Key Takeaways
- Vision, Mission, and Philosophy form the foundation of nursing services, guiding all aspects of planning and practice.
- Well-defined Objectives translate aspirational goals into measurable targets, providing direction and benchmarks for success.
- Nursing Service Policies establish formal standards and ensure consistency, quality, and regulatory compliance.
- Procedures and Manuals provide detailed guidance for implementing policies and standardizing nursing practice.
- Functional and Operational Planning address the practical, day-to-day aspects of nursing service delivery.
- Strategic Planning sets the long-term direction for nursing services, aligning with organizational goals and adapting to changing healthcare environments.
Effective planning at all levels is essential for nursing services to deliver high-quality, patient-centered care while optimizing resources and adapting to evolving healthcare demands.
References
- National Council of State Boards of Nursing. (2023). Achieving Regulatory Goals Through Strategic Planning. Journal of Nursing Regulation.
- American Nurses Association. (2025). Code of Ethics for Nurses. https://codeofethics.ana.org/home
- McNeese-Smith, D. (2022). Strategic Planning for a Very Different Nursing Workforce. NCBI. https://pmc.ncbi.nlm.nih.gov/articles/PMC8770040/
- ShiftMed. (2024). Developing a Nursing Strategic Plan: Key Components and Benefits. https://www.shiftmed.com/insights/knowledge-center/developing-a-nursing-strategic-plan-key-components-and-benefits/
- Cherry, B., & Jacob, S. R. (2024). Contemporary Nursing: Issues, Trends, & Management. Elsevier.
- Huber, D. (2024). Leadership and Nursing Care Management. Elsevier.
- MCN Solutions. (2025). Exploring the Difference Between Nursing Procedures and Policies. https://www.mcnsolutions.com/exploring-difference-nursing-procedure-policy/
Program Planning, Budgeting, and Hospital Planning
Comprehensive Nursing Education Notes
1. Program Planning
Program planning in healthcare and nursing involves systematic organization and scheduling of activities to achieve specific objectives. Two popular tools for visualizing and managing program timelines are Gantt charts and milestone charts.
1.1 Gantt Chart
Definition: A Gantt chart is a horizontal bar chart that shows the tasks of a project, when each task must take place, and how long each task will take to complete.
Key Components of a Gantt Chart
- Tasks: Activities that need to be completed
- Timeline: The project duration represented horizontally
- Task bars: Horizontal bars representing the duration of each task
- Dependencies: Links showing which tasks must be completed before others can begin
- Milestones: Key events or achievements marked on the chart
- Resources: People or materials assigned to tasks
Benefits of Gantt Charts in Nursing Program Planning
| Benefit | Description |
|---|---|
| Visual Timeline | Provides clear visualization of the entire project schedule |
| Task Management | Shows task dependencies, durations, and overlaps |
| Resource Allocation | Helps identify when and where resources are needed |
| Progress Tracking | Allows monitoring of actual progress against planned schedule |
| Communication Tool | Facilitates communication about project status to stakeholders |
Creating a Gantt Chart for Nursing Projects
Practical Tip
Nursing projects like implementing a new patient care protocol or organizing a health camp can be efficiently managed using Gantt charts. This helps in coordinating multidisciplinary teams and ensures timely completion of critical healthcare interventions.
1.2 Milestone Chart
Definition: A milestone chart is a visual representation that focuses on significant events or achievements (milestones) within a project’s timeline rather than detailing every task.
Key Components of a Milestone Chart
- Milestones: Key events or achievements in the project
- Timeline: Dates or periods when milestones should be reached
- Status indicators: Visual markers showing whether milestones are completed, in progress, or pending
Benefits of Milestone Charts in Nursing Program Planning
| Benefit | Description |
|---|---|
| Simplified Overview | Provides a high-level view of project progress without overwhelming details |
| Focus on Key Achievements | Emphasizes important accomplishments rather than everyday tasks |
| Stakeholder Communication | Easily communicates progress to executives and stakeholders |
| Motivation Tool | Celebrates achievements and motivates team members |
| Deadline Management | Helps track critical deadlines for important deliverables |
Creating a Milestone Chart for Nursing Projects
Mnemonic: “SMART Milestones”
Specific: Clearly defined and understood by all stakeholders
Measurable: Can be definitively completed or achieved
Achievable: Realistic given the resources available
Relevant: Directly related to project goals
Time-bound: Associated with a specific date or timeframe
1.3 Comparison: Gantt vs. Milestone Charts
- Shows detailed activities with their durations
- Displays task dependencies and relationships
- Focuses on the entire project timeline and all tasks
- More complex and detailed
- Useful for day-to-day management and coordination
- Best for operational planning and tracking
- Shows only key events or achievements
- Focuses on important dates rather than tasks
- Provides a high-level overview of project progress
- Simpler and less detailed
- Useful for executive reporting and stakeholder communications
- Best for strategic planning and monitoring
When to Use Each Chart
Use a Gantt Chart when: You need detailed project management, resource allocation, and task dependency tracking.
Use a Milestone Chart when: You need a simplified overview focusing on key achievements and deadlines for stakeholder reporting.
Nursing Application Example
For a complex nursing intervention program like implementing a new wound care protocol:
- Gantt Chart: Use for detailed planning of staff training sessions, equipment procurement, pilot testing, and full implementation with specific dates and durations.
- Milestone Chart: Use for tracking and reporting key achievements like “Staff Training Completed,” “Pilot Testing Successful,” and “Protocol Fully Implemented” to nursing leadership and hospital administration.
2. Budgeting in Healthcare
Budgeting is a critical aspect of healthcare management that ensures financial resources are allocated efficiently to deliver quality patient care while maintaining fiscal responsibility.
2.1 Budgeting Concepts
Definition: Healthcare budgeting is the process of estimating revenue and expenses over a specified timeframe to allocate resources effectively for optimal patient outcomes and organizational sustainability.
Key Budgeting Concepts in Healthcare
| Concept | Description |
|---|---|
| Revenue Forecasting | Estimating income from various sources including patient services, insurance reimbursements, grants, and donations |
| Expense Projection | Predicting costs for staffing, supplies, equipment, facilities, and other operational expenses |
| Variance Analysis | Comparing actual financial performance against budgeted amounts to identify and address discrepancies |
| Cost Centers | Organizational units or departments for which costs are separately identified and allocated |
| Fiscal Year | The 12-month period used for financial planning and reporting |
| Break-Even Analysis | Determining the point at which revenue equals expenses with no profit or loss |
The Healthcare Budgeting Process
2.2 Budgeting Principles
Mnemonic: “CAREFUL Budgeting”
Comprehensive: Include all financial aspects of operations
Accurate: Based on realistic estimates, not wishful thinking
Realistic: Achievable within the constraints of resources
Efficient: Maximizing outputs from limited inputs
Flexible: Adaptable to changing circumstances
Understandable: Clear to all stakeholders
Linking: Connected to organizational goals and strategic plans
Core Principles of Healthcare Budgeting
- Transparency: Clear documentation and communication of budget decisions
- Accountability: Responsibility for budget management assigned to specific individuals
- Participatory Approach: Involving department heads and frontline staff in budget development
- Evidence-Based: Using historical data and benchmarks to inform projections
- Priority Setting: Allocating resources based on organizational priorities and patient needs
- Risk Management: Identifying and mitigating financial risks
- Continuous Monitoring: Regular review and adjustment throughout the fiscal year
Nurse Manager’s Role in Budgeting
Nurse managers play a crucial role in healthcare budgeting by:
- Forecasting staffing needs based on patient acuity and volume
- Managing supply utilization and identifying cost-saving opportunities
- Monitoring overtime and agency staff usage
- Justifying capital equipment purchases
- Creating business cases for new services or programs
- Analyzing variances and implementing corrective actions
2.3 Types of Budgets
| Type of Budget | Description | Application in Healthcare |
|---|---|---|
| Operating Budget | Covers daily operational expenses and revenues | Staff salaries, medical supplies, utilities, routine maintenance |
| Capital Budget | Funds major investments in long-term assets | Medical equipment, building renovations, health information systems |
| Cash Flow Budget | Projects timing of cash inflows and outflows | Managing timing disparities between service delivery and payment collection |
| Program Budget | Allocates resources to specific service lines or initiatives | Diabetes education program, wound care clinic, vaccination campaigns |
| Zero-Based Budget | Starts from zero and justifies all expenses | Comprehensive review of all departmental expenses during financial constraints |
| Flexible Budget | Adjusts based on activity levels | Adapting staffing and supply costs based on patient census fluctuations |
| Fixed Budget | Remains constant regardless of activity levels | Administrative overhead, facility maintenance, contracted services |
| Incremental Budget | Based on previous year with incremental changes | Annual adjustments based on inflation, volume changes, and new initiatives |
Advantages
- Simple and familiar
- Less time-consuming
- Promotes stability and continuity
Disadvantages
- Perpetuates historical inefficiencies
- May not align with changing priorities
- Less rigorous justification for spending
Advantages
- Eliminates wasteful spending
- Aligns resources with current priorities
- Encourages innovation and efficiency
Disadvantages
- Time and resource intensive
- May create uncertainty and stress
- Requires extensive justification
Budget Implementation Tips for Nurse Leaders
- Develop a clear understanding of financial terminology and principles
- Engage staff in cost-saving initiatives to promote ownership
- Monitor key performance indicators regularly (e.g., hours per patient day, supply costs)
- Collaborate with finance departments to develop accurate forecasts
- Document justifications for budget variances thoroughly
- Consider patient outcomes when making financial decisions
3. Budget Proposal
A budget proposal is a formal document that presents a financial plan for a specific project, department, or organization. In healthcare, well-crafted budget proposals are essential for securing funding for initiatives that improve patient care and operational efficiency.
3.1 Components of a Budget Proposal
Essential Elements of a Healthcare Budget Proposal
- Executive Summary: Brief overview of the proposal, highlighting key points and requested funding amount
- Background and Need: Context and justification for the budget request
- Goals and Objectives: Specific, measurable outcomes the funding will achieve
- Methodology: How the funds will be used to achieve stated objectives
- Itemized Budget: Detailed breakdown of all anticipated expenses
- Budget Narrative: Explanation and justification for each budget line item
- Cost-Benefit Analysis: Comparison of costs versus expected benefits
- Timeline: Schedule for implementation and fund utilization
- Evaluation Plan: Methods to assess effectiveness and financial performance
- Sustainability Plan: Strategy for continued funding or self-sustainability
Types of Expenses in Healthcare Budget Proposals
| Expense Category | Examples | Budgeting Considerations |
|---|---|---|
| Personnel | Salaries, benefits, overtime, contract staff | Include all related costs (taxes, benefits); account for annual increases |
| Equipment | Medical devices, computers, furniture | Include maintenance, depreciation, training costs |
| Supplies | Medical supplies, medications, office supplies | Consider usage patterns, inflation, storage costs |
| Facility | Rent, utilities, maintenance, renovations | Account for seasonal variations and potential increases |
| Training | Staff education, certifications, conferences | Include travel costs, materials, replacement staffing |
| Technology | Software licenses, IT support, system upgrades | Consider implementation and ongoing support costs |
| Administrative | Insurance, legal fees, accreditation costs | Include often overlooked indirect expenses |
Tips for Creating Effective Healthcare Budget Proposals
- Align budget requests with organizational strategic priorities
- Use data from reliable sources to support projections
- Include contingency planning for unexpected expenses
- Highlight return on investment and patient outcome improvements
- Be transparent about assumptions used in calculations
- Consider multiple funding scenarios (minimum, preferred, optimal)
- Use visual aids like charts and graphs to illustrate key points
- Have financial experts review your proposal before submission
3.2 Cost-Benefit Analysis
Definition: Cost-benefit analysis (CBA) is a systematic approach to estimating the strengths and weaknesses of alternatives by determining benefits and costs, allowing healthcare organizations to evaluate the value of decisions or investments.
Steps in Conducting a Healthcare Cost-Benefit Analysis
Types of Benefits in Healthcare Analysis
| Benefit Type | Description | Examples |
|---|---|---|
| Direct Financial Benefits | Monetary gains directly attributable to the intervention | Revenue increases, cost savings, reduced length of stay |
| Indirect Financial Benefits | Secondary monetary effects | Reduced staff turnover, decreased liability costs |
| Quantifiable Non-Financial Benefits | Measurable but not directly monetary | Reduced readmission rates, increased patient satisfaction scores |
| Qualitative Benefits | Difficult to quantify but valuable | Improved staff morale, enhanced reputation, better work environment |
Key Financial Metrics for Cost-Benefit Analysis
| Metric | Description | Formula |
|---|---|---|
| Return on Investment (ROI) | Ratio of net profit to investment cost | (Net Profit / Cost of Investment) × 100% |
| Net Present Value (NPV) | Current value of all future cash flows | Sum of (Cash Flow / (1 + Discount Rate)^t) for all periods |
| Benefit-Cost Ratio (BCR) | Ratio of benefits to costs | Present Value of Benefits / Present Value of Costs |
| Payback Period | Time required to recoup the initial investment | Initial Investment / Annual Cash Flow |
| Internal Rate of Return (IRR) | Discount rate that makes NPV zero | Complex calculation requiring iterative approach |
Mnemonic: “COSTS & BENEFITS”
Capital expenditures (one-time costs)
Operational expenses (ongoing costs)
Staffing requirements and changes
Training and implementation costs
Supportive infrastructure needs
&
Better patient outcomes
Efficiency improvements
New revenue opportunities
Enhanced safety measures
Financial savings
Improved staff satisfaction
Time savings in processes
Strengthened competitive position
Common Pitfalls in Healthcare Cost-Benefit Analysis
- Overlooking indirect costs or benefits
- Failing to consider the time value of money
- Overly optimistic projections of benefits
- Underestimating implementation challenges
- Not accounting for staff resistance or adoption barriers
- Ignoring qualitative benefits that may be significant
- Insufficient sensitivity analysis for variable factors
Nursing Application Example
Cost-Benefit Analysis for a Pressure Ulcer Prevention Program:
Costs:
- Staff training: $10,000
- Specialized mattresses: $60,000
- Documentation system updates: $5,000
- Additional nursing time for positioning: $45,000/year
Benefits:
- Reduced treatment costs: $120,000/year
- Shorter lengths of stay: $80,000/year
- Decreased liability risk: $40,000/year
- Improved quality metrics and reimbursement: $20,000/year
Analysis:
- First-year ROI: [($260,000 – $120,000) ÷ $120,000] × 100% = 117%
- Payback period: $75,000 ÷ ($260,000 – $45,000) = 0.35 years (about 4 months)
This analysis demonstrates that despite significant upfront and ongoing costs, the pressure ulcer prevention program is financially beneficial within a short timeframe, not to mention the qualitative benefits of improved patient comfort and satisfaction.
4. Planning Hospital and Patient Care Unit
Hospital planning involves the systematic organization of physical spaces, workflows, and resources to optimize healthcare delivery. Effective planning ensures that facilities support efficient operations, enhance patient experiences, and improve clinical outcomes.
4.1 Hospital Planning Principles
Definition: Hospital planning is the strategic process of designing healthcare facilities to optimize patient care, staff efficiency, and resource utilization while maintaining flexibility for future healthcare delivery changes.
Key Principles of Hospital Planning
Mnemonic: “SPACES”
Safety: Prioritize patient and staff safety in all design decisions
Patient-centered: Design with patient needs and experiences in mind
Accessibility: Ensure spaces are accessible to all users
Cost-effectiveness: Balance quality with financial constraints
Efficiency: Optimize workflows and minimize unnecessary movement
Sustainability: Consider environmental impact and long-term viability
Hospital Planning Considerations
| Planning Aspect | Key Considerations |
|---|---|
| Site Selection |
|
| Space Programming |
|
| Circulation Planning |
|
| Infrastructure Planning |
|
| Equipment Planning |
|
Hospital Planning Process
Evidence-Based Design in Hospital Planning
Evidence-based design (EBD) uses research findings to inform healthcare facility design decisions. Key EBD principles include:
- Single-patient rooms reduce infections and improve patient satisfaction
- Access to natural light improves patient outcomes and staff wellbeing
- Decentralized nurse stations reduce walking distances and increase patient care time
- Noise reduction strategies improve patient sleep and reduce stress
- Appropriate HVAC systems with proper filtration minimize airborne infections
- Clear wayfinding systems reduce stress and improve efficiency
- Standardized room layouts reduce medical errors
4.2 Patient Care Unit (Ward) Design
Definition: A patient care unit or ward is a designated area within a healthcare facility where inpatient care is provided to a specific patient population, typically organized around nursing care delivery models.
Types of Ward Layouts
| Ward Type | Description | Advantages | Disadvantages |
|---|---|---|---|
| Open Ward (Nightingale) | Large open space with multiple beds arranged along walls |
|
|
| Bay Ward | Semi-partitioned areas with 4-6 beds per bay |
|
|
| Corridor (Racetrack) | Patient rooms arranged along corridor(s), with central support services |
|
|
| Cruciform/Cluster | Rooms arranged around a central nursing station |
|
|
| Courtyard | Rooms arranged around a central courtyard or atrium |
|
|
Key Elements in Patient Care Unit Planning
- Nursing Station Design
- Centralized vs. decentralized configurations
- Line of sight to patient rooms
- Integration of technology and communication systems
- Balance of privacy and collaboration spaces
- Patient Room Design
- Single vs. multi-occupancy considerations
- Standardization for safety and efficiency
- Family accommodation spaces
- Technology integration
- Accessibility features
- Support Spaces
- Medication rooms/areas
- Clean and soiled utility rooms
- Storage areas for supplies and equipment
- Staff workspaces and break areas
- Family/visitor spaces
- Workflow Considerations
- Medication delivery systems
- Supply chain and logistics
- Waste management
- Patient transport routes
Mnemonic: “NURSE WARD”
Noise control features (acoustic treatments, quiet areas)
Utility spaces strategically located (clean/dirty, medication rooms)
Room standardization for safety and efficiency
Staff workspace optimization (charting, collaboration)
Ergonomic considerations for patient and staff safety
Wayfinding that’s intuitive and clear
Accessibility for all users (patients, staff, visitors)
Resilient design for emergencies and disasters
Daylight and views to improve well-being
Acuity-Adaptable Room Design
Acuity-adaptable patient rooms are designed to accommodate varying levels of patient acuity, reducing the need to transfer patients as their conditions change. Benefits include:
- Reduced Transfers: Decreases complications associated with moving patients
- Continuity of Care: Same care team throughout hospitalization
- Improved Patient Safety: Fewer handoff errors
- Enhanced Patient Satisfaction: More stable environment for patients and families
- Space Efficiency: Flexible use of rooms based on census and acuity
These rooms require careful planning for medical gas outlets, monitoring capabilities, and appropriate space for equipment at various acuity levels.
Nursing Workflow Considerations in Ward Design
Nurse leaders should advocate for unit designs that support efficient nursing workflows:
- Decentralized supplies located close to point of use
- Medication preparation areas with minimal interruptions
- Documentation stations with visibility to patients
- Appropriate staff-to-patient ratios based on unit layout
- Support for team communication and collaboration
- Technology integration that minimizes workarounds
- Workspaces that reduce nursing fatigue and injury
5. Planning for Emergency and Disaster
Emergency and disaster planning in healthcare settings involves developing comprehensive strategies to prepare for, respond to, and recover from unexpected events that can disrupt normal operations and threaten patient safety.
5.1 Disaster Management Cycle
Definition: The disaster management cycle is a continuous process of planning, organizing, coordinating, and implementing measures to prevent, prepare for, respond to, and recover from disasters and emergencies.
Four Phases of the Disaster Management Cycle
| Phase | Description | Key Activities |
|---|---|---|
| Mitigation & Prevention | Activities that reduce the likelihood or impact of disasters |
|
| Preparedness | Activities that build capacity to respond effectively to disasters |
|
| Response | Immediate actions during an emergency to save lives and limit damage |
|
| Recovery | Activities to restore operations and services to normal |
|
Mnemonic: “DISASTER Preparedness”
Develop plans for various scenarios
Inventory critical resources and supplies
Staff training and role assignments
Assess vulnerabilities and risks
Standardize communication protocols
Test plans through regular drills
Establish mutual aid agreements
Review and revise plans periodically
Types of Disasters Affecting Healthcare Facilities
| Category | Examples | Specific Planning Considerations |
|---|---|---|
| Natural Disasters | Hurricanes, earthquakes, floods, wildfires |
|
| Technological Disasters | Power outages, IT system failures, medical gas failures |
|
| Human-Caused Incidents | Active shooter, terrorism, civil unrest, mass casualty incidents |
|
| Public Health Emergencies | Pandemics, bioterrorism, radiation exposure |
|
| Internal Disasters | Fire, hazardous material spills, structural failure |
|
5.2 Hospital Emergency Response
Hospital Incident Command System (HICS)
Definition: HICS is an emergency management system that uses a standardized organizational structure to help hospitals prepare for, respond to, and recover from emergencies of all types.
Key Components of a Hospital Emergency Operations Plan
- Emergency Management Committee: Multidisciplinary team responsible for planning and oversight
- Hazard Vulnerability Analysis (HVA): Assessment of potential threats and their likely impact
- Incident Command Structure: Clear chain of command during emergencies
- Communication Plans: Internal and external notification procedures
- Resource Management: Processes for obtaining and allocating supplies and personnel
- Evacuation and Shelter-in-Place Procedures: Guidelines for when and how to move patients
- Surge Capacity Planning: Strategies to expand service capacity during crises
- Training and Exercise Program: Regular drills to test plans and build competency
- Documentation Systems: Methods for tracking patients, resources, and decisions
- Recovery Procedures: Steps to restore normal operations
Nursing Roles in Emergency and Disaster Response
| Role | Responsibilities |
|---|---|
| Direct Care Provider |
|
| Unit Leader |
|
| Triage Officer |
|
| Planning Section Member |
|
| Public Health Liaison |
|
Essential Emergency Supplies for Hospital Units
- Clinical Supplies: Extra IV fluids, wound care supplies, medications
- Documentation Tools: Paper forms, patient tracking boards, identification bands
- Communication Devices: Handheld radios, backup phones, runner vests
- Personal Protective Equipment: Various levels based on potential hazards
- Lighting: Flashlights, headlamps, battery-powered lanterns
- Power: Extension cords, power strips, battery chargers
- Patient Support: Blankets, comfort items, hydration supplies
- Staff Support: Food, water, personal hygiene items
- Evacuation Equipment: Stair chairs, patient sleds, transfer devices
These supplies should be regularly inventoried, maintained, and staff should be trained on their location and proper use.
Emergency Response Training for Healthcare Staff
(All Staff)
(Direct Care Providers)
(Unit Leaders)
(Incident Command)
| Training Level | Content | Frequency |
|---|---|---|
| Awareness Level |
|
Annually and at orientation |
| Operation Level |
|
Bi-annually with quarterly drills |
| Technical Level |
|
Quarterly training with functional exercises |
| Management Level |
|
Monthly training with full-scale exercises twice yearly |
Common Emergency Planning Pitfalls to Avoid
- Creating plans that are too complex or difficult to implement
- Failing to update plans based on lessons learned from exercises
- Insufficient training of staff on their roles during emergencies
- Not accounting for special populations (pediatrics, geriatrics, disabilities)
- Overlooking staff personal/family needs during extended emergencies
- Inadequate communication plans for internal and external stakeholders
- Failing to coordinate with community partners and resources
- Not testing backup systems regularly under load conditions
Mnemonic: “RAPID Emergency Response”
Recognize the emergency or disaster situation
Activate the emergency plan and notification systems
Protect patients, visitors, and staff from harm
Implement triage and treatment protocols
Document actions, decisions, and patient information
Post-Disaster Evaluation and Improvement
After every emergency response, whether real or simulated, a thorough evaluation should be conducted:
- Hot Wash: Immediate post-event discussion to capture key observations
- Formal Debriefing: Structured review with all participants
- After-Action Report: Detailed analysis of what worked and what didn’t
- Improvement Plan: Specific corrective actions with assigned responsibilities
- Plan Revisions: Updates to emergency plans based on lessons learned
- Training Adjustments: Modifications to training programs to address gaps
This continuous improvement cycle is essential for maintaining effective emergency preparedness.
Conclusion
Effective program planning, budgeting, and hospital planning are essential skills for nursing professionals, especially those in leadership and management positions. These competencies enable nurses to participate meaningfully in healthcare decision-making, improve resource allocation, enhance patient care environments, and prepare for emergencies and disasters.
By understanding and applying the concepts of Gantt charts, milestone charts, budgeting principles, cost-benefit analysis, hospital design, and emergency planning, nurses can contribute significantly to organizational success while advancing their own professional development.
Remember that these tools and frameworks should always be implemented with the ultimate goal of improving patient outcomes, enhancing staff efficiency, and promoting the overall quality of healthcare delivery.
