Postnatal Baby Blues and Recognition of Postnatal Depression
Comprehensive Nursing Notes for Students
Table of Contents
- 1. Introduction to Postnatal Mood Disorders
- 2. Normal Postnatal Baby Blues
- 3. Postnatal Depression
- 4. Comparison: Baby Blues vs. Postnatal Depression
- 5. Nursing Assessment and Recognition
- 6. Nursing Interventions and Management
- 7. Prevention Strategies
- 8. Mnemonics for Recognition and Assessment
- 9. Global Best Practices
- 10. References
1. Introduction to Postnatal Mood Disorders
The postpartum period represents a time of significant physical, emotional, and social change for new mothers. During this crucial transition, many women experience alterations in their postnatal mood that can range from mild and temporary to severe and persistent. Understanding these postnatal mood disorders is essential for nursing professionals to provide appropriate care and support to new mothers.
Postnatal mood disorders exist on a spectrum, with baby blues at the mild end, postnatal depression in the middle, and postpartum psychosis at the severe end. This educational resource focuses on the recognition and differentiation between normal postnatal baby blues and postnatal depression, equipping nursing students with the knowledge to identify, assess, and support mothers experiencing these conditions.
Note: As nursing professionals, recognizing the difference between normal baby blues and postnatal depression is crucial for appropriate intervention and support. Early recognition can significantly impact maternal well-being and infant development.
2. Normal Postnatal Baby Blues
2.1 Definition and Prevalence
Postnatal baby blues (also called “postpartum blues” or simply “baby blues”) refers to a brief period of mild mood disturbances that commonly occurs in the first few days after childbirth. This condition is considered a normal physiological response to the dramatic hormonal shifts that follow delivery.
- Prevalence: Affects approximately 70-80% of new mothers
- Onset: Typically begins 2-3 days after delivery
- Duration: Usually resolves spontaneously within 10-14 days postpartum
- Impact: Generally mild and does not significantly impair functioning or maternal-infant bonding
The high prevalence of baby blues makes it important for healthcare providers to normalize this experience for new mothers while simultaneously monitoring for signs of progression to more serious conditions.
2.2 Pathophysiology and Hormonal Changes
The etiology of baby blues is primarily attributed to the dramatic hormonal fluctuations that occur following childbirth, though psychological and social factors also contribute. Understanding these physiological changes helps explain why mild mood disturbances are so common during this period.
| Hormonal Change | Description | Impact on Mood |
|---|---|---|
| Estrogen & Progesterone | Sharp decline from pregnancy levels (10-fold decrease within days) | Contributes to mood lability, emotional sensitivity, and tearfulness |
| Oxytocin | Fluctuating levels with breastfeeding and infant contact | Affects bonding and emotional responses; contributes to emotional sensitivity |
| Prolactin | Elevated levels, especially with breastfeeding | May contribute to fatigue and mood changes |
| Cortisol | Altered levels following pregnancy | Can affect stress responses and emotional regulation |
| Thyroid Hormones | Potential transient fluctuations postpartum | Thyroid dysregulation can mimic or contribute to mood symptoms |
Additional physiological factors include:
- Sleep deprivation and disrupted sleep patterns
- Physical recovery from childbirth
- Inflammatory processes related to tissue healing
- Changes in neurotransmitter activity (particularly serotonin)
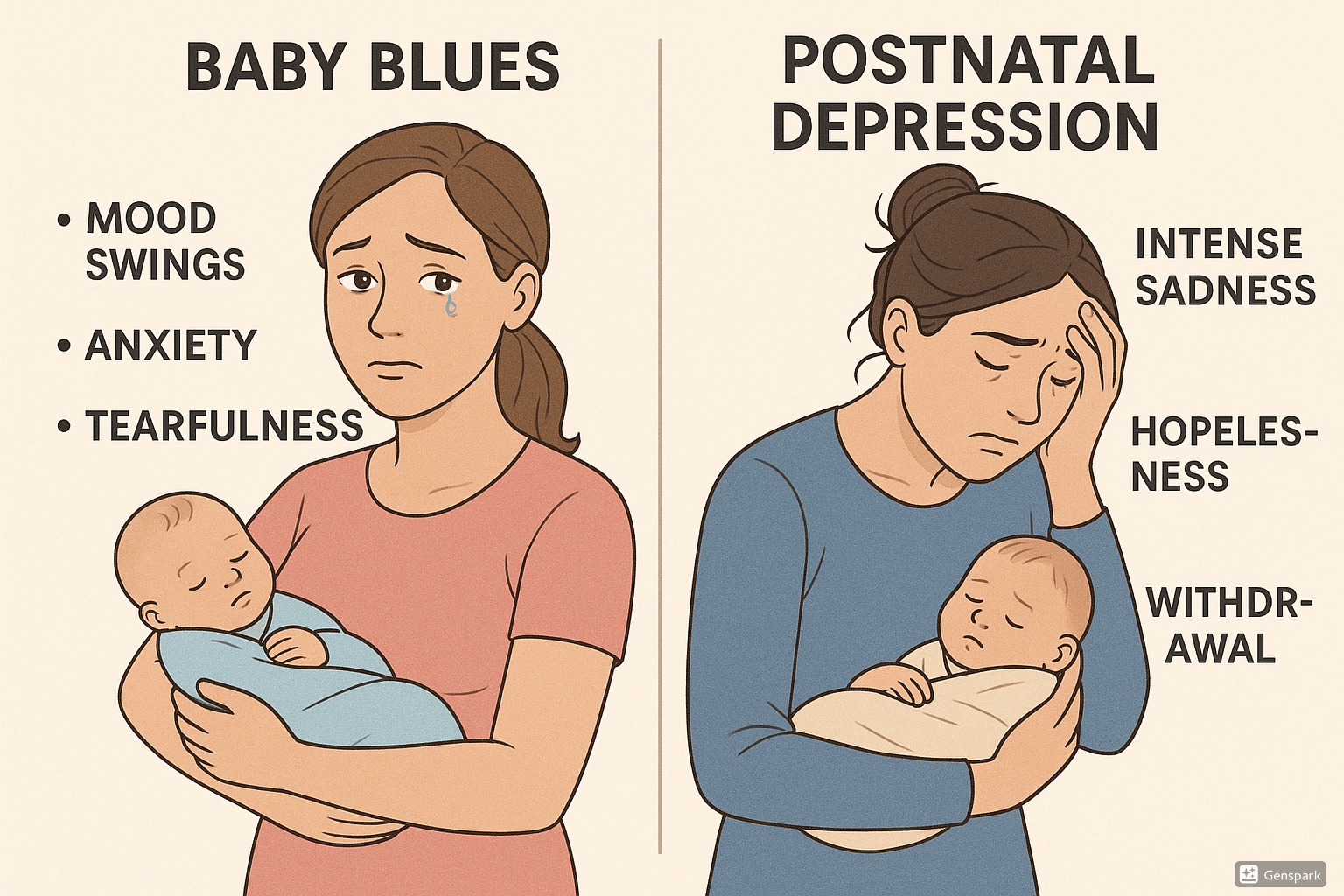
Figure 1: Visual comparison of baby blues versus postnatal depression symptoms and severity
2.3 Signs and Symptoms
The symptoms of baby blues are typically mild and self-limiting. Recognizing these symptoms helps differentiate normal baby blues from more serious postnatal mood disorders.
Mnemonic: “BLUES”
B – Bouts of crying (often for no apparent reason)
L – Labile moods (mood swings)
U – Unsettled feelings (anxiety, restlessness)
E – Exhaustion (fatigue beyond normal tiredness)
S – Sleep difficulties (unrelated to infant care)
Common symptoms of baby blues include:
- Tearfulness and crying episodes
- Emotional sensitivity and mood fluctuations
- Mild anxiety or worry
- Irritability
- Feeling overwhelmed
- Fatigue beyond that expected from sleep disruption
- Concentration difficulties
Important: Despite these symptoms, mothers with baby blues typically:
- Maintain the ability to care for themselves and their baby
- Experience periods of positive emotions and joy
- Don’t have persistent negative thoughts about themselves or the baby
- Don’t experience thoughts of self-harm or harming the baby
2.4 Management and Support
Management of baby blues focuses primarily on support, education, and reassurance rather than medical intervention. As nurses, providing appropriate guidance during this period can help prevent progression to more serious conditions.
Key Support Strategies:
- Education and Normalization: Explain that baby blues are common and temporary
- Emotional Support: Encourage expression of feelings without judgment
- Rest: Promote sleep when possible (e.g., “sleep when baby sleeps”)
- Social Support: Encourage partner/family involvement in infant care and household tasks
- Self-Care: Emphasize the importance of basic self-care (nutrition, hydration, brief periods away from baby)
- Monitoring: Observe for signs that symptoms are persisting beyond two weeks or worsening
When to Be Concerned: If symptoms persist beyond two weeks, worsen rather than improve, or begin to interfere with daily functioning or infant care, further assessment for postnatal depression is warranted.
3. Postnatal Depression
3.1 Definition and Prevalence
Postnatal depression (PND) is a more severe and persistent form of postnatal mood disturbance that meets the clinical criteria for a major depressive episode occurring within the first year after childbirth. Unlike baby blues, PND represents a serious mental health condition requiring professional intervention.
- Prevalence: Affects approximately 10-15% of new mothers
- Onset: Can begin anytime within the first year after delivery, often developing gradually
- Duration: Without treatment, may persist for months or even years
- Impact: Significantly impairs functioning, maternal-infant bonding, and family dynamics
PND is often underdiagnosed and undertreated, highlighting the importance of routine screening and vigilant observation by healthcare providers during the postnatal period.
3.2 Pathophysiology and Risk Factors
The development of postnatal depression involves a complex interplay of biological, psychological, and social factors. Understanding these multifactorial causes is essential for comprehensive assessment and intervention planning.
Biological Factors:
- Hormonal fluctuations (estrogen, progesterone, thyroid hormones)
- Genetic predisposition
- Neurotransmitter dysregulation (serotonin, dopamine, norepinephrine)
- Inflammatory processes
- Sleep deprivation and circadian rhythm disruption
Risk Factors for Postnatal Depression:
| Category | Risk Factors | Relative Risk |
|---|---|---|
| Personal History |
|
High |
| Pregnancy/Birth Factors |
|
Moderate |
| Psychosocial Factors |
|
Moderate to High |
| Demographic Factors |
|
Moderate |
Important: Risk assessment should be conducted during pregnancy and the early postnatal period to identify women who may benefit from closer monitoring and preventive interventions.
3.3 Clinical Presentation and Symptoms
Postnatal depression presents with symptoms similar to major depression occurring at other times of life, but with some specific features related to motherhood and infant care. Recognizing these symptoms is critical for early identification and intervention.
Mnemonic: “MOTHERS”
M – Mood disturbance (persistent sadness, emptiness)
O – Overwhelming anxiety about baby care
T – Tearfulness and emotional lability that persists
H – Hopelessness about the future
E – Energy severely diminished beyond normal fatigue
R – Reduced interest in baby and self-care
S – Suicidal thoughts or thoughts of harming the baby
Key symptoms to watch for include:
- Persistent low mood that doesn’t lift for most of the day, nearly every day
- Anhedonia (loss of interest or pleasure in activities previously enjoyed)
- Fatigue or loss of energy beyond that expected from caring for a newborn
- Feelings of worthlessness or excessive guilt, particularly about mothering abilities
- Difficulty thinking, concentrating, or making decisions
- Sleep disturbances (inability to sleep when baby sleeps)
- Appetite changes (significant weight loss or gain)
- Psychomotor agitation or retardation
- Recurrent thoughts of death or suicide
Motherhood-Specific Symptoms:
- Difficulty bonding with the baby
- Persistent doubts about ability to care for the infant
- Intrusive thoughts about harming the baby (often very distressing to the mother)
- Excessive worry about infant health or safety
- Feeling detached or distant from the baby
Warning Signs Requiring Immediate Attention:
- Suicidal ideation with plan or intent
- Thoughts of harming the baby
- Psychotic symptoms (hallucinations, delusions)
- Severe functional impairment affecting basic self-care or infant care
3.4 Assessment and Screening Tools
Regular screening for postnatal depression is recommended for all women in the postnatal period. The most widely used and validated screening tool is the Edinburgh Postnatal Depression Scale (EPDS).
Edinburgh Postnatal Depression Scale (EPDS):
- 10-item self-report questionnaire
- Takes approximately 5 minutes to complete
- Each item scored 0-3, with a maximum score of 30
- Cut-off scores:
- ≥ 10: Possible depression (mild)
- ≥ 13: Likely depression (moderate to severe)
- Includes item assessing suicidal thoughts (Question 10)
Other assessment tools include:
- Patient Health Questionnaire-9 (PHQ-9)
- Postpartum Depression Screening Scale (PDSS)
- Beck Depression Inventory (BDI)
Clinical assessment should include:
- Comprehensive psychiatric history
- Evaluation of risk factors
- Assessment of support systems
- Screening for comorbid anxiety disorders
- Evaluation of mother-infant interaction
- Assessment of risk to mother and infant
4. Comparison: Baby Blues vs. Postnatal Depression
Understanding the key differences between normal baby blues and postnatal depression is essential for accurate assessment and appropriate intervention planning. The following table highlights the distinguishing features of these postnatal mood disorders.
| Feature | Baby Blues | Postnatal Depression |
|---|---|---|
| Prevalence | 70-80% of new mothers | 10-15% of new mothers |
| Onset | 2-3 days after delivery | Can occur anytime within first year, often gradual onset |
| Duration | Self-limiting; resolves within 10-14 days | Persists beyond 2 weeks; may continue for months without treatment |
| Severity | Mild mood fluctuations | Moderate to severe symptoms meeting criteria for clinical depression |
| Impact on functioning | Minimal impact; able to function and care for self/baby | Significant impairment in daily functioning and infant care |
| Mood | Tearful at times but with periods of positive mood | Persistent low mood most of the day, nearly every day |
| Bonding with baby | Generally intact, occasional worry about care abilities | May be significantly impaired; detachment, disinterest, or excessive anxiety |
| Thoughts | Normal concerns, no persistent negative thinking | Persistent negative thoughts, feelings of worthlessness or guilt |
| Risk of self-harm | Not present | May include suicidal thoughts or thoughts of harming baby |
| Treatment needed | Support, reassurance, education | Professional intervention (therapy, medication, social support) |
Clinical Pearl: When symptoms persist beyond two weeks, increase in severity, or significantly impact mother-infant interaction, postnatal depression should be suspected rather than baby blues.
5. Nursing Assessment and Recognition
5.1 Edinburgh Postnatal Depression Scale (EPDS)
The Edinburgh Postnatal Depression Scale (EPDS) is the gold standard screening tool for postnatal mood disorders. As nurses, understanding how to administer and interpret this tool is essential for effective screening.
Key Points about the EPDS:
- Validated specifically for use during the perinatal period
- Focuses on symptoms of depression rather than normal physiological changes of motherhood
- Available in multiple languages
- Can be administered in various settings (hospital, clinic, home visits)
- Recommended timing:
- First screening: 6-8 weeks postpartum (routine)
- Earlier screening for women with risk factors
- Repeat screening at 3-4 months and 6-9 months
EPDS Screening Process:
- Explain purpose of screening in non-stigmatizing manner
- Provide privacy and time to complete questionnaire
- Score responses (0-3 points per question, maximum 30 points)
- Interpret results:
- Score < 10: Likely normal adjustment
- Score 10-12: Possible depression, monitor closely
- Score ≥ 13: Probable depression, requires further assessment
- Any score > 0 on Question 10 (thoughts of self-harm): Requires immediate attention regardless of total score
- Document results and follow-up plan
Important: The EPDS is a screening tool, not a diagnostic instrument. A high score indicates the need for further clinical assessment, not a definitive diagnosis of depression.
5.2 Assessment Process
A comprehensive nursing assessment for postnatal mood disorders involves more than just administering screening tools. The following approach ensures thorough evaluation:
Key Components of Assessment:
- Observation:
- Mother’s affect, appearance, and behavior
- Quality of interaction with the baby
- Level of engagement in conversation
- Interview:
- Current mood and emotional state
- Sleep patterns (beyond normal disruption from infant care)
- Appetite changes
- Energy levels and motivation
- Thoughts about self as a mother
- Concerns about caring for the baby
- Support systems and resources
- Risk Assessment:
- Previous mental health history
- Family history of perinatal mood disorders
- Current stressors
- History of trauma
- Substance use
- Thoughts of self-harm or harming the baby
- Physical Assessment:
- Physical recovery from childbirth
- Signs of fatigue beyond expected
- Signs of poor self-care
Mnemonic: “NURSE”
N – Notice mood changes and behavioral cues
U – Understand risk factors and previous history
R – Recognize differences between blues and depression
S – Screen using validated tools like EPDS
E – Evaluate support systems and safety concerns
Documentation should include:
- Screening results with specific scores
- Observed behaviors and interactions
- Mother’s self-report of symptoms
- Risk factors identified
- Support systems available
- Plan for follow-up or referral
6. Nursing Interventions and Management
6.1 Interventions for Baby Blues
For women experiencing normal baby blues, nursing interventions focus on support, education, and promoting self-care strategies. These interventions aim to normalize the experience and prevent progression to more severe postnatal mood disorders.
Key Nursing Interventions:
- Education:
- Explain that baby blues are common and temporary
- Discuss hormonal changes and normal adjustment to motherhood
- Teach signs that would indicate development of postnatal depression
- Emotional Support:
- Provide active listening and validation of feelings
- Normalize emotional responses to motherhood
- Create safe space for expression of ambivalent feelings
- Practical Support:
- Provide guidance on infant care and feeding
- Assist with problem-solving for common challenges
- Encourage acceptance of help from support network
- Self-Care Promotion:
- Emphasize importance of rest when possible
- Encourage adequate nutrition and hydration
- Recommend brief periods of self-care activities
- Support System Engagement:
- Involve partner/family in education about baby blues
- Discuss division of responsibilities
- Identify specific support needs
6.2 Interventions for Postnatal Depression
When postnatal depression is identified or suspected, nursing interventions become more intensive and involve coordination with other healthcare providers. The nurse plays a crucial role in supporting treatment adherence and monitoring response.
Key Nursing Interventions:
| Intervention Category | Specific Interventions |
|---|---|
| Assessment & Monitoring |
|
| Referral & Coordination |
|
| Therapeutic Support |
|
| Practical Assistance |
|
| Medication Management |
|
| Mother-Infant Relationship |
|
Emergency Interventions: In cases involving suicidal ideation, psychosis, or thoughts of harming the infant, immediate psychiatric evaluation is required. Never leave the mother and infant alone if there are safety concerns.
7. Prevention Strategies
Prevention of postnatal mood disorders, particularly postnatal depression, involves identifying at-risk women and implementing strategies to reduce risk and enhance protective factors.
Evidence-Based Preventive Approaches:
- Antenatal Screening: Identifying women at risk during pregnancy
- Psychoeducation: Information about normal postpartum adjustment and warning signs of depression
- Sleep Protection: Strategies to maximize sleep quality and quantity
- Support Enhancement: Strengthening social support networks
- Psychological Interventions: Preventive cognitive-behavioral therapy for high-risk women
- Physical Activity: Regular, moderate exercise during pregnancy and postpartum
- Nutritional Support: Balanced diet with attention to omega-3 fatty acids, vitamin D, and B vitamins
Best Practice: Preventive Counseling
The U.S. Preventive Services Task Force recommends counseling interventions, such as cognitive behavioral therapy and interpersonal therapy, for pregnant and postpartum women at increased risk of perinatal depression. These interventions have shown effectiveness in preventing postnatal depression when initiated during pregnancy or early postpartum.
Nursing Role in Prevention:
- Conduct thorough risk assessment during pregnancy and early postpartum
- Provide anticipatory guidance about normal postpartum adjustment
- Help develop a postpartum support plan before delivery
- Facilitate connections to community resources
- Teach stress management and self-care strategies
- Implement routine screening protocols
- Support partner involvement in infant care and maternal support
8. Mnemonics for Recognition and Assessment
Mnemonics are valuable tools for nursing students to remember key aspects of postnatal mood disorders. The following mnemonics can aid in assessment and intervention planning.
Mnemonic: “DEPRESSION” – Symptoms of Postnatal Depression
D – Depressed mood most of the day, nearly every day
E – Energy loss or fatigue beyond normal postpartum tiredness
P – Pleasure loss (anhedonia) in activities previously enjoyed
R – Relentless guilt or feelings of worthlessness as a mother
E – Eating changes (significant appetite increase or decrease)
S – Sleep disturbances (beyond infant care disruptions)
S – Suicidal thoughts or thoughts of harming the baby
I – Impaired concentration or indecisiveness
O – Overwhelmed by responsibilities of motherhood
N – Notable psychomotor agitation or retardation
Mnemonic: “SUPPORT” – Nursing Interventions for Postnatal Mood Disorders
S – Screen regularly using validated tools
U – Understand and validate the mother’s experience
P – Provide information about resources and treatment options
P – Promote self-care and adequate rest
O – Offer practical assistance with infant care when needed
R – Refer to appropriate mental health services
T – Track symptoms and response to interventions
Mnemonic: “RISKS” – Risk Factors for Postnatal Depression
R – Recent stressful life events
I – Insufficient social support
S – Suffered previous depression (personal history)
K – Kin with mental health disorders (family history)
S – Stressful pregnancy or delivery complications
9. Global Best Practices
Approaches to managing postnatal mood disorders vary around the world, with some countries implementing innovative and effective practices that can inform nursing care globally.
Notable International Approaches:
- Australia: National Perinatal Depression Initiative with universal screening and integrated care pathways
- United Kingdom: Specialist perinatal mental health teams and mother-baby psychiatric units
- Netherlands: Postpartum doula care (kraamzorg) provided for all new mothers
- Japan: Traditional postpartum care (“Satogaeri”) involving maternal family support
- Canada: Telephone-based support programs and online therapy options
- Sweden: Extended parental leave policies supporting parental mental health
Emerging Best Practices:
- Peer Support Models: Trained peer supporters with lived experience of perinatal mood disorders
- Digital Health Interventions: Mobile apps and online platforms for screening and support
- Group Interventions: Group therapy and education sessions combining professional and peer support
- Couple-Based Approaches: Involving partners in assessment and treatment
- Culturally Adapted Interventions: Tailoring approaches to specific cultural contexts and beliefs
- Integrated Care Models: Embedding mental health care within maternal-child health services
Cultural Considerations
Cultural beliefs and practices significantly influence how postpartum mood disorders are understood, expressed, and treated. Nurses should consider cultural factors when assessing and supporting women from diverse backgrounds, including:
- Cultural expressions of emotional distress
- Traditional postpartum practices and their protective effects
- Family dynamics and decision-making processes
- Stigma and beliefs about mental health
- Language barriers and communication preferences
10. References
- American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text revision).
- World Health Organization. (2022). Maternal mental health.
- National Institute for Health and Care Excellence. (2020). Antenatal and postnatal mental health: Clinical management and service guidance.
- Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatry, 150(6), 782-786.
- U.S. Preventive Services Task Force. (2019). Interventions to prevent perinatal depression: U.S. Preventive Services Task Force recommendation statement. JAMA, 321(6), 580-587.
- O’Hara, M. W., & McCabe, J. E. (2013). Postpartum depression: Current status and future directions. Annual Review of Clinical Psychology, 9, 379-407.
- Pearlstein, T., Howard, M., Salisbury, A., & Zlotnick, C. (2009). Postpartum depression. American Journal of Obstetrics and Gynecology, 200(4), 357-364.
- Centers for Disease Control and Prevention. (2023). Depression among women.
- Dennis, C. L., & Dowswell, T. (2013). Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database of Systematic Reviews, (2).
- Wisner, K. L., Sit, D. K., McShea, M. C., Rizzo, D. M., Zoretich, R. A., Hughes, C. L., … & Hanusa, B. H. (2013). Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry, 70(5), 490-498.
