Premature Rupture of Membranes (PROM)
Comprehensive Nursing Education Notes for Understanding, Assessment, and Management
Definition & Overview
Key Definition
Premature Rupture of Membranes (PROM) is the spontaneous rupture of the amniotic sac (chorioamniotic membranes) before the onset of labor, regardless of gestational age. When this occurs before 37 weeks of gestation, it is specifically termed Preterm Premature Rupture of Membranes (PPROM).
Epidemiology
- Occurs in 8-10% of all pregnancies
- PPROM affects 2-3% of pregnancies
- Accounts for 30-40% of preterm deliveries
- Higher incidence in developing countries
Clinical Significance
- Leading cause of perinatal morbidity
- Increased risk of maternal infection
- Fetal complications due to prematurity
- Requires immediate medical attention
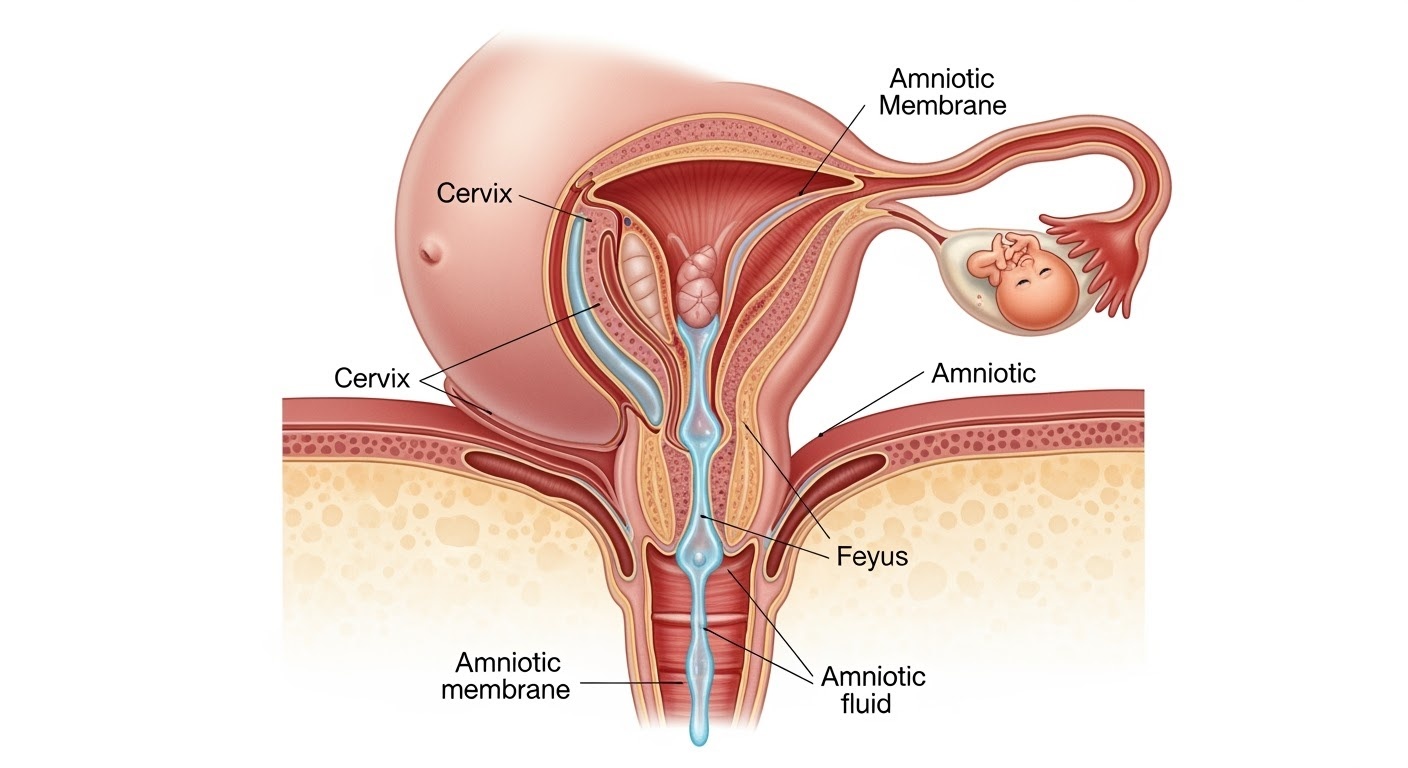
Medical illustration showing premature rupture of membranes with amniotic fluid leakage
Pathophysiology
Normal Membrane Structure
Chorioamniotic Membrane: Consists of two layers
- • Amnion: Inner layer, direct contact with amniotic fluid
- • Chorion: Outer layer, adherent to decidua
Function: Maintains amniotic fluid, protects fetus, prevents infection
Membrane Rupture Process
Weakening Factors:
- • Inflammatory processes
- • Collagen degradation
- • Mechanical stress
- • Enzymatic breakdown
Result: Loss of structural integrity leading to rupture
Molecular Mechanisms
Inflammation
Cytokine release, neutrophil infiltration, tissue damage
Proteolysis
Matrix metalloproteinases breakdown collagen matrix
Apoptosis
Programmed cell death weakens membrane structure
Classification of PROM
| Classification | Gestational Age | Key Features | Management Priority |
|---|---|---|---|
| Term PROM | ≥37 weeks | Lower risk of complications | Labor induction considerations |
| Preterm PROM (PPROM) | <37 weeks | Higher morbidity risk | Balance infection vs prematurity |
| Previable PPROM | <24 weeks | Poor fetal outcomes | Counseling and ethical considerations |
| Late Preterm PPROM | 34-36+6 weeks | Moderate prematurity risks | Delivery often indicated |
PROM Classification Mnemonic: “TIME”
T – Term (≥37 weeks)
I – Immature (<24 weeks)
M – Moderate preterm (24-33+6)
E – Early term (34-36+6)
Etiology & Risk Factors
Infectious Causes
Ascending Infection:
- • Group B Streptococcus (GBS)
- • Escherichia coli
- • Bacteroides species
- • Ureaplasma urealyticum
Other Infections:
- • Urinary tract infections
- • Sexually transmitted infections
- • Respiratory tract infections
Maternal Risk Factors
Demographic:
- • Young maternal age (<18 years)
- • Low socioeconomic status
- • African American ethnicity
- • Poor prenatal care
Medical:
- • Previous PROM history
- • Cervical insufficiency
- • Connective tissue disorders
- • Nutritional deficiencies
Pregnancy-Related Factors
Uterine Factors:
- • Polyhydramnios (excess amniotic fluid)
- • Multiple gestation
- • Uterine overdistension
- • Abnormal fetal presentation
Placental Issues:
- • Placental abruption
- • Placenta previa
- • Decidual bleeding
Environmental & Lifestyle
- Smoking during pregnancy
- Alcohol consumption
- Illicit drug use
- Poor living conditions
- Malnutrition
Risk Factors Mnemonic: “MEMBRANE”
M – Multiple gestation
E – Early maternal age
M – Maternal infection
B – Bacterial vaginosis
R – Race (African American)
A – Amniotic fluid excess
N – Nutritional deficiency
E – Environmental toxins
Clinical Presentation
Primary Symptom
Fluid Leakage
Sudden gush or continuous trickling of clear, odorless amniotic fluid from the vagina
Associated Signs
- Decreased fetal movement
- Uterine contractions (may be absent initially)
- Vaginal bleeding (if associated with abruption)
- Pelvic pressure or cramping
Infection Signs
- Maternal fever (>38°C/100.4°F)
- Maternal tachycardia (>100 bpm)
- Fetal tachycardia (>160 bpm)
- Foul-smelling amniotic fluid
- Uterine tenderness
Differential Diagnosis Considerations
Urinary Incontinence
Check for urea/creatinine levels
Vaginal Discharge
Assess consistency and pH
Cervical Mucus
Consider gestational age
Semen
Recent sexual activity history
Comprehensive Nursing Assessment
Initial History Taking
Essential Questions:
- When did the fluid leakage begin?
- Was it a sudden gush or gradual leaking?
- What is the color and odor of the fluid?
- Are you experiencing contractions?
- When was your last prenatal visit?
- Any recent infections or illnesses?
Physical Assessment
Maternal Vital Signs:
Abdominal Assessment:
- • Fundal height measurement
- • Uterine contractions assessment
- • Fetal presentation and position
- • Uterine tenderness evaluation
Fetal Assessment
Continuous Monitoring:
Assessment Priority:
Immediate fetal well-being evaluation to detect signs of distress or compromise
Infection Screening
Clinical Signs:
Assessment Mnemonic: “FLUID”
F – Fetal status
Heart rate, movement, well-being
L – Leakage characteristics
Color, odor, amount, timing
U – Uterine activity
Contractions, tenderness
I – Infection signs
Fever, tachycardia, malodor
D – Delivery readiness
Cervical status, presentation
Diagnostic Methods
Clinical Diagnosis
Sterile Speculum Examination:
- • Visualization of amniotic fluid pooling in posterior fornix
- • Avoid digital cervical examination (increases infection risk)
- • Observe for fluid leakage from cervical os
- • Note color, consistency, and odor of fluid
Golden Standard: Direct visualization of amniotic fluid leakage
Laboratory Tests
pH Testing:
- • Normal vaginal pH: 3.5-4.5
- • Amniotic fluid pH: 7.1-7.3
- • Use nitrazine paper or pH strips
- • False positives: blood, semen, bacterial vaginosis
Ferning Test:
- • Dried amniotic fluid shows fern-like crystallization
- • Viewed under microscope
- • High specificity for amniotic fluid
- • False positives: cervical mucus, fingerprints
Advanced Biomarker Tests
PAMG-1 (PartoSure®)
- • Placental alpha microglobulin-1
- • Highly specific for amniotic fluid
- • Sensitivity: 98.9%, Specificity: 100%
- • Quick bedside test (10 minutes)
IGFBP-1 (Actim PROM®)
- • Insulin-like growth factor binding protein-1
- • Rapid immunochromatographic test
- • Results in 5-10 minutes
- • High accuracy in clinical studies
Ultrasound Assessment
Oligohydramnios Evaluation:
AFI Method:
- • Normal: 8-25 cm
- • Oligohydramnios: <5 cm
MVP Method:
- • Normal: >2 cm
- • Oligohydramnios: <2 cm
Note: Normal amniotic fluid levels do not rule out PROM (resealing may occur)
| Diagnostic Test | Sensitivity | Specificity | Time to Result | Limitations |
|---|---|---|---|---|
| Clinical Visualization | 95-98% | 99% | Immediate | Requires active leakage |
| Nitrazine Test | 90-97% | 16-70% | 2-3 minutes | Many false positives |
| Ferning Test | 85-98% | 70-85% | 5-10 minutes | Requires microscope |
| PAMG-1 Test | 98.9% | 100% | 10 minutes | Cost, availability |
| IGFBP-1 Test | 96-100% | 88-100% | 5-10 minutes | Cost, training needed |
Management & Treatment
Term PROM Management (≥37 weeks)
Immediate Approach:
- Delivery recommended within 12-24 hours
- Labor induction if spontaneous labor doesn’t occur
- GBS prophylaxis if indicated
- Monitor for signs of infection
Goal: Balance infection risk with delivery timing
Preterm PROM (PPROM) Management
Conservative Management (24-34 weeks):
- Hospitalization for close monitoring
- Antibiotic prophylaxis (7-10 days)
- Corticosteroids for fetal lung maturity
- Tocolytics generally contraindicated
Pharmacological Interventions
Antibiotic Prophylaxis:
First-line regimen (7 days):
- • Ampicillin 2g IV q6h × 48 hours
- • Then Amoxicillin 250mg PO q8h × 5 days
- • Plus Erythromycin 250mg PO q6h × 7 days
Corticosteroids:
Betamethasone course:
- • 12mg IM × 2 doses, 24 hours apart
- • Indicated 24-34 weeks gestation
- • Reduces neonatal morbidity
Emergency Indications for Delivery
- Clinical chorioamnionitis
- Non-reassuring fetal heart rate patterns
- Placental abruption
- Cord prolapse
- Preterm labor progression
Decision-Making Algorithm
≥37 weeks
Proceed with delivery within 12-24 hours
24-36 weeks
Conservative management with close monitoring
<24 weeks
Counseling about outcomes and options
Management Mnemonic: “DELIVER”
D – Determine gestational age
E – Evaluate for infection
L – Labs (CBC, cultures)
I – Initiate antibiotics if indicated
V – Vital signs monitoring
E – Evaluate fetal well-being
R – Ready for delivery if needed
Complications of PROM
Maternal Complications
Chorioamnionitis:
- • Incidence: 15-25% with PROM
- • Higher risk with longer latency period
- • Can lead to maternal sepsis
- • Requires immediate antibiotic treatment
Other Complications:
- Endometritis (postpartum infection)
- Increased cesarean delivery risk
- Placental abruption
- Retained placenta
Risk Timeline
Infection Risk by Duration:
- • <6 hours: Minimal risk increase
- • 6-12 hours: Moderate risk increase
- • 12-24 hours: Significant risk increase
- • >24 hours: High risk of complications
Fetal & Neonatal Complications
Immediate Complications:
- • Cord prolapse (1-2% incidence)
- • Variable fetal heart rate decelerations
- • Fetal distress from oligohydramnios
- • Cord compression
Prematurity-Related:
- • Respiratory distress syndrome
- • Intraventricular hemorrhage
- • Necrotizing enterocolitis
- • Developmental delays
Infection-Related:
- • Early-onset neonatal sepsis
- • Pneumonia
- • Meningitis
- • Long-term neurological sequelae
Severe Complications Requiring Immediate Action
Chorioamnionitis Signs
Cord Prolapse Emergency
Complication Statistics by Gestational Age
Nursing Interventions
Immediate Nursing Actions
Initial Assessment:
- Obtain complete set of vital signs
- Assess fetal heart rate and patterns
- Document time and characteristics of fluid leakage
- Position patient appropriately
Time is critical – prompt assessment and notification of healthcare provider
Infection Prevention
Strict Aseptic Technique:
- Hand hygiene before and after all patient contact
- Avoid unnecessary vaginal examinations
- Use sterile technique for all procedures
- Maintain clean, dry perineal area
Continuous Monitoring
Vital Signs:
- • Temperature every 2-4 hours
- • Pulse and blood pressure every 4 hours
- • Respiratory rate as indicated
- • Report temperature >38°C immediately
Fetal Monitoring:
- • Continuous electronic fetal monitoring
- • Assess for variable decelerations
- • Monitor fetal movement patterns
- • Document any changes in FHR patterns
Documentation Requirements
- Time of membrane rupture
- Amount, color, and odor of amniotic fluid
- Fetal presentation and station
- Contraction patterns
- Patient response to interventions
Nursing Care Plan for PROM
| Nursing Diagnosis | Goals/Outcomes | Interventions | Evaluation |
|---|---|---|---|
| Risk for infection | Absence of infection signs | Monitor vital signs, aseptic technique, antibiotic administration | Temperature normal, no signs of infection |
| Risk for fetal injury | Maintained fetal well-being | Continuous FHR monitoring, position changes, cord prolapse prevention | FHR within normal limits, no cord prolapse |
| Anxiety related to pregnancy complications | Reduced anxiety levels | Provide information, emotional support, involve family | Patient verbalizes understanding and reduced anxiety |
| Knowledge deficit | Understanding of condition and treatment | Patient education, written materials, answer questions | Patient demonstrates understanding of care plan |
Nursing Interventions Mnemonic: “MONITOR”
M – Monitor vital signs
O – Observe for infection signs
N – Notify provider of changes
I – Implement infection control
T – Track fetal well-being
O – Offer emotional support
R – Record all findings
Patient & Family Education
Understanding PROM
Key Teaching Points:
- Explain what premature rupture of membranes means
- Discuss potential causes and risk factors
- Review importance of timing in management
- Address common fears and misconceptions
Emphasize that PROM is not caused by anything the patient did wrong
Warning Signs to Report
Call Healthcare Provider Immediately for:
- Fever over 100.4°F (38°C)
- Foul-smelling or colored vaginal discharge
- Severe abdominal or back pain
- Decreased fetal movement
- Regular contractions
- Heavy bleeding
Home Care Instructions
Activity Restrictions:
- No sexual intercourse
- No douching or tampons
- No baths (showers only)
- Bed rest as prescribed
- Light activity only if permitted
Hygiene Practices:
- • Gentle cleansing with warm water
- • Pat dry, don’t rub perineal area
- • Change perineal pads frequently
- • Wipe front to back only
Medication Compliance
Antibiotic Education:
- Take medications exactly as prescribed
- Complete the entire course even if feeling better
- Take at same times each day
- Take with food if stomach upset occurs
Emotional Support & Coping
Addressing Anxiety
- • Acknowledge fears and concerns as normal
- • Provide accurate, honest information
- • Encourage questions and open communication
- • Discuss relaxation techniques
- • Connect with support groups if available
Family Involvement
- • Include partner/family in education sessions
- • Teach family members warning signs
- • Encourage family support and assistance
- • Discuss role changes during bed rest
- • Address family concerns and questions
Patient Education Mnemonic: “TEACH”
T – Tell about condition
Explain PROM clearly
E – Explain warning signs
When to seek help
A – Activity restrictions
Rest and limitations
C – Compliance with meds
Proper medication use
H – Hygiene practices
Infection prevention
Global Best Practices & Innovations
United Kingdom – NICE Guidelines
Key Innovations:
- Routine use of PAMG-1 testing for diagnosis
- Expectant management protocols for 24-34 weeks
- Standardized antibiotic regimens
- Quality metrics tracking for outcomes
Result: 15% reduction in neonatal morbidity rates
Canada – Maternal-Fetal Medicine Networks
Integrated Care Model:
- Telemedicine consultations for remote areas
- Rapid transport protocols to tertiary centers
- Standardized nursing education modules
- National registry for outcome tracking
Japan – Technology Integration
Innovative Technologies:
- Mobile apps for patient symptom tracking
- AI-assisted risk stratification algorithms
- Continuous remote fetal monitoring devices
- Point-of-care biomarker testing
Outcome: 40% reduction in unnecessary hospitalizations
Nordic Countries – Midwifery Model
Holistic Approach:
- Home-based monitoring when appropriate
- Family-centered care approaches
- Natural birth promotion when safe
- Psychological support integration
Achievement: Highest maternal satisfaction scores globally
Emerging Global Trends
Genomic Testing
Genetic risk assessment for PROM susceptibility
Targeted Therapies
Personalized antibiotic and steroid protocols
Remote Monitoring
Wearable devices for continuous maternal-fetal assessment
AI Integration
Machine learning for outcome prediction and optimization
Key Takeaways for Nursing Practice
Evidence-Based Practices:
- • Early and accurate diagnosis is crucial
- • Standardized protocols improve outcomes
- • Multidisciplinary care enhances safety
- • Patient education reduces anxiety
