Promoting Safety in Health Care Environment
Physical Environment Factors for Nursing Students
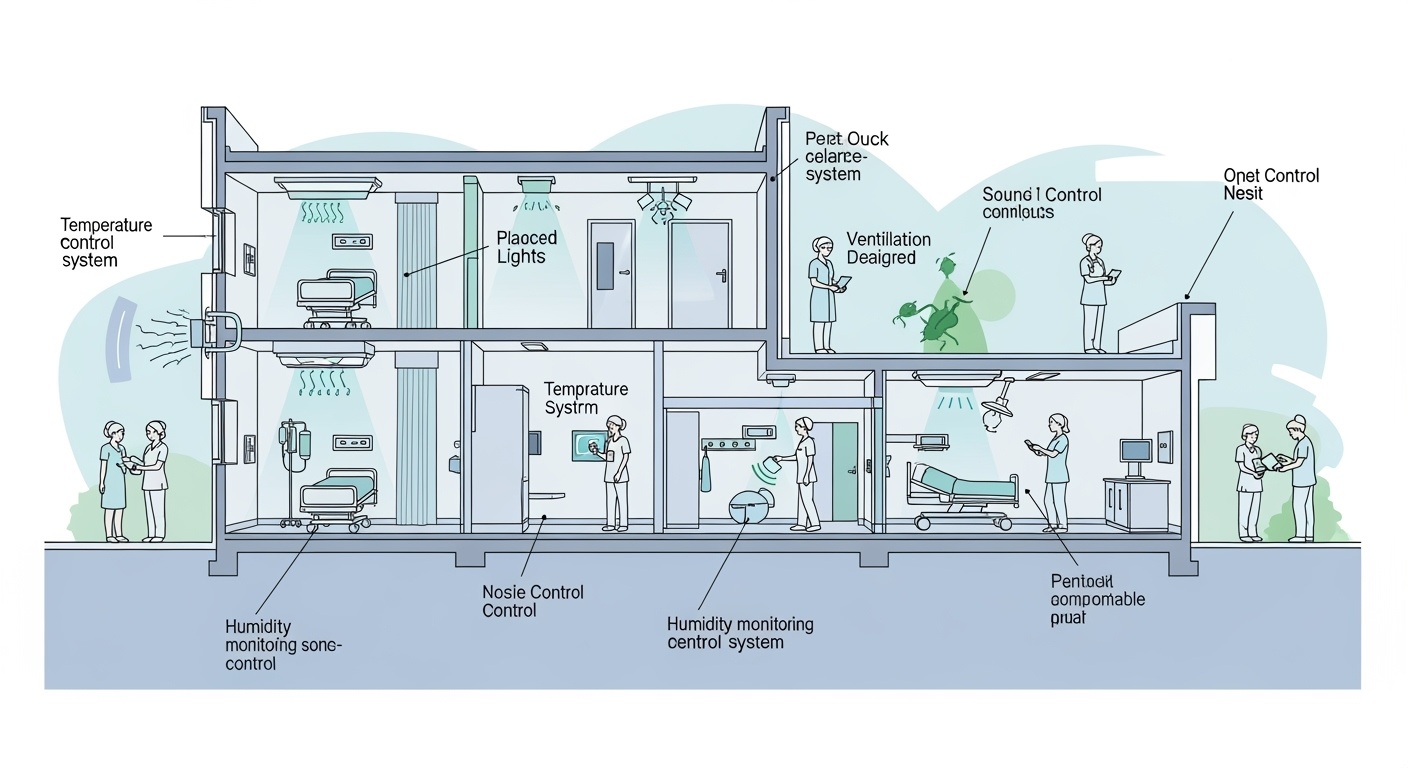
Figure 1: Comprehensive Healthcare Environmental Safety Systems
Introduction to Healthcare Environmental Safety
Healthcare environmental safety is a critical component of patient care that directly impacts clinical outcomes, staff wellbeing, and overall healthcare quality. As nursing professionals, understanding and managing physical environmental factors is essential for creating healing environments that promote recovery while preventing healthcare-associated complications.
The physical healthcare environment encompasses multiple interconnected systems that must work harmoniously to maintain optimal conditions for patient care. These systems include temperature control, humidity management, noise reduction, ventilation systems, lighting optimization, odor control, and pest management.
Master Mnemonic: “THRILL-VP”
Temperature • Humidity • Room Air Quality • Illumination • Light Management • Low Noise • Ventilation • Pest Control
Temperature Control
Optimal Temperature Ranges
- Patient Rooms: 68-75°F (20-24°C)
- Operating Rooms: 68-73°F (20-23°C)
- Nurseries: 72-78°F (22-26°C)
- Laboratory: 72-78°F (22-26°C)
- Pharmacy: 68-77°F (20-25°C)
Physiological Impact
- Too Hot: Increased metabolic rate, dehydration, heat stress
- Too Cold: Vasoconstriction, shivering, hypothermia risk
- Cardiac Impact: Temperature extremes increase cardiac workload
- Respiratory: Cold air can trigger bronchospasm
Nursing Implementation Strategies
Assessment & Monitoring
- • Monitor patient comfort levels q4h
- • Check room thermostats regularly
- • Assess for signs of thermal stress
- • Document temperature complaints
Interventions
- • Adjust bedding and clothing
- • Coordinate with facilities management
- • Provide comfort measures (blankets, fans)
- • Educate patients on thermal comfort
Critical Considerations
Vulnerable Populations: Elderly patients, neonates, and immunocompromised individuals are particularly sensitive to temperature variations. Continuous monitoring and rapid response to temperature concerns are essential.
Humidity Management
Optimal Humidity Levels
Too Low (<30%)
- • Dry skin and mucous membranes
- • Increased static electricity
- • Respiratory irritation
- • Increased infection risk
Optimal (30-60%)
- • Comfortable breathing
- • Reduced static electricity
- • Optimal skin condition
- • Minimized pathogen survival
Too High (>60%)
- • Mold and bacteria growth
- • Equipment corrosion
- • Allergic reactions
- • Condensation problems
Humidity Mnemonic: “MOIST”
Monitor levels • Optimal 30-60% • Infection control • Skin comfort • Technical equipment protection
Nursing Assessment & Intervention
Assessment Techniques
- Visual inspection for condensation
- Tactile assessment of air moisture
- Use of hygrometers when available
- Patient reports of comfort/discomfort
Intervention Strategies
- Coordinate with facilities management
- Provide humidification or dehumidification
- Monitor for mold or bacterial growth
- Document humidity-related issues
Noise Management
Noise Level Standards
Common Noise Sources
- Medical Equipment: Monitors, ventilators, pumps
- Alarms: Call bells, emergency alerts
- Human Activity: Conversations, footsteps
- Transportation: Gurneys, wheelchairs
- Construction: Maintenance, renovations
Health Impact of Noise
- Sleep Disruption: Fragmented sleep cycles
- Cardiovascular: Increased blood pressure, heart rate
- Cognitive: Impaired concentration, memory
- Psychological: Increased stress, anxiety
- Healing: Delayed recovery, prolonged hospitalization
Noise Control Mnemonic: “QUIET”
Quiet zones • Unit-wide protocols • Incident reporting • Equipment maintenance • Time-sensitive activities
Noise Reduction Strategy Flowchart
Practical Noise Reduction Strategies
Immediate Actions
- • Lower voice levels
- • Close doors gently
- • Use soft-soled shoes
- • Adjust alarm volumes
- • Cluster care activities
Team Collaboration
- • Communicate during shift changes
- • Coordinate with housekeeping
- • Work with maintenance
- • Educate family members
- • Establish quiet hours
System Changes
- • Sound-absorbing materials
- • Equipment modifications
- • Workflow optimization
- • Policy development
- • Staff training programs
Ventilation Systems
Ventilation Requirements
General Patient Areas
6-12 air changes per hour (ACH)
Operating Rooms
15-25 ACH with positive pressure
Isolation Rooms
12+ ACH with negative pressure
ICU
6-12 ACH with controlled pressure
Ventilation Functions
- Infection Control: Remove airborne pathogens
- Temperature Regulation: Maintain thermal comfort
- Humidity Control: Manage moisture levels
- Air Quality: Remove odors and contaminants
- Oxygen Supply: Ensure adequate fresh air
Ventilation Mnemonic: “FRESH”
Filtration • Recirculation • Exhaust • Supply air • Humidity control
Nursing Ventilation Management
Assessment Points
- Visual inspection of vents and filters
- Feel for adequate air movement
- Detect unusual odors or stuffiness
- Monitor patient comfort levels
- Check isolation room pressure indicators
Intervention Strategies
- Report ventilation issues immediately
- Manage door positions (isolation protocols)
- Ensure filters are clean and functional
- Implement temporary measures if needed
- Document all ventilation concerns
Critical Ventilation Alerts
Never ignore ventilation alarms or failures. Compromised ventilation can lead to rapid spread of airborne infections, compromised patient safety, and regulatory violations. Always prioritize immediate reporting and temporary protective measures.
Lighting Optimization
Lighting Requirements by Area
Patient Rooms
5-50 foot-candles (adjustable)
Nursing Stations
50-100 foot-candles
Operating Rooms
1000-2000 foot-candles
Hallways
10-20 foot-candles
Lighting Effects on Health
Positive Effects
- • Improved circadian rhythm regulation
- • Enhanced mood and mental health
- • Better visual acuity and safety
- • Increased vitamin D synthesis
Negative Effects
- • Eye strain and fatigue
- • Sleep disruption
- • Headaches and migraines
- • Seasonal affective disorder
Lighting Mnemonic: “BRIGHT”
Balanced intensity • Room-appropriate levels • Incandescent vs LED • Glare reduction • Healthy circadian patterns • Task-specific lighting
Nursing Lighting Management
Assessment
- • Evaluate lighting adequacy
- • Check for flickering or dim lights
- • Assess patient comfort
- • Identify glare sources
- • Monitor circadian disruption
Interventions
- • Adjust lighting levels appropriately
- • Use task-specific lighting
- • Implement day/night lighting cycles
- • Reduce glare with positioning
- • Provide reading lights
Coordination
- • Report lighting failures
- • Coordinate with facilities
- • Educate patients on lighting needs
- • Document lighting-related issues
- • Advocate for lighting improvements
Odor Management
Common Healthcare Odors
- Chemical: Disinfectants, medications, anesthetics
- Biological: Body fluids, waste, wound drainage
- Food-related: Meal preparation, dietary areas
- Environmental: Mold, mildew, poor ventilation
- Maintenance: Cleaning supplies, paint, construction
Impact on Patient Care
- Psychological: Anxiety, depression, stress
- Physical: Nausea, vomiting, appetite loss
- Respiratory: Breathing difficulties, allergic reactions
- Cognitive: Concentration problems, memory issues
- Recovery: Delayed healing, prolonged stays
Odor Control Mnemonic: “FRESH”
Find the source • Remove or neutralize • Ensure ventilation • Sanitize effectively • Healthy environment maintenance
Odor Control Strategy
Identify
Locate source of odor
Remove
Eliminate source if possible
Neutralize
Use appropriate odor control
Prevent
Implement prevention measures
Nursing Odor Management Strategies
Immediate Actions
- Quickly identify odor source
- Remove soiled items immediately
- Improve air circulation
- Use appropriate odor neutralizers
- Isolate affected areas if needed
Prevention Measures
- Implement regular cleaning schedules
- Maintain proper hygiene protocols
- Ensure proper waste disposal
- Maintain adequate ventilation
- Monitor and document odor incidents
Pest Control Management
Common Healthcare Pests
- Insects: Ants, flies, cockroaches, mosquitoes
- Rodents: Mice, rats
- Birds: Pigeons, sparrows
- Microorganisms: Mold, bacteria, fungi
- Parasites: Bed bugs, fleas, lice
Health Risks
- Disease Transmission: Bacterial, viral, parasitic infections
- Allergic Reactions: Respiratory, skin reactions
- Physical Harm: Bites, stings, wounds
- Food Contamination: Foodborne illnesses
- Compromised Immunity: Increased infection risk
Pest Control Mnemonic: “CLEAN”
Clean environment • Limit food sources • Eliminate entry points • Assess regularly • Notify professionals
Integrated Pest Management (IPM) Approach
Prevention
Eliminate attractants
Monitoring
Regular inspections
Identification
Proper pest identification
Treatment
Targeted interventions
Nursing Pest Control Responsibilities
Daily Vigilance
- • Inspect patient areas
- • Check food storage areas
- • Monitor waste disposal
- • Observe for pest signs
- • Document findings
Prevention Actions
- • Maintain clean environment
- • Proper food storage
- • Seal entry points
- • Remove standing water
- • Educate patients/families
Response Protocol
- • Report immediately
- • Isolate affected areas
- • Contact facilities management
- • Implement temporary measures
- • Follow up on treatment
Critical Pest Control Alerts
Never use unauthorized pesticides in healthcare settings. Always coordinate with licensed pest control professionals and facilities management. Some pest control chemicals can be harmful to patients, especially those with respiratory conditions or compromised immune systems.
Comprehensive Implementation Framework
Daily Assessment Checklist
Quality Improvement Process
1. Data Collection
Systematically gather environmental data and patient feedback
2. Analysis
Identify patterns, trends, and areas for improvement
3. Intervention
Implement evidence-based solutions and modifications
4. Evaluation
Assess effectiveness and make necessary adjustments
Interdisciplinary Collaboration
Facilities Management
HVAC, lighting, maintenance
Environmental Services
Cleaning, waste management
Infection Control
Safety protocols, compliance
Quality Assurance
Performance monitoring
Key Takeaways for Nursing Practice
Core Principles
- Holistic Assessment: Environmental factors are interconnected and impact patient outcomes
- Proactive Monitoring: Regular assessment prevents problems before they impact care
- Patient-Centered Care: Environmental comfort directly affects healing and recovery
- Collaborative Approach: Effective environmental management requires teamwork
Professional Development
- Continuing Education: Stay current with environmental safety standards
- Certification: Pursue specialized training in environmental health
- Innovation: Contribute to environmental improvement initiatives
- Leadership: Advocate for environmental safety in healthcare settings
Final Master Mnemonic: “NURSES CARE”
Noise management
Understanding patient needs
Respiratory air quality
Sanitary environment
Environmental safety
Comfort optimization
Air circulation
Room temperature control
Everything for healing
