Breastfeeding Essentials: Proper Latching & Managing Uterine Cramps
Comprehensive guide for nursing students on breastfeeding techniques, proper latching, and management of postpartum uterine cramps
Introduction to Breastfeeding
Breastfeeding provides optimal nutrition for infants while fostering a unique bond between mother and child. It offers numerous benefits for both the infant and the mother, including improved immunity for the baby and reduced risk of certain diseases for the mother. As healthcare professionals, understanding the physiological and psychological aspects of breastfeeding is crucial for providing effective support to new mothers.
Key Benefits of Breastfeeding:
- Provides ideal nutrition for infants with the perfect mix of vitamins, protein, and fat
- Contains antibodies that help babies fight viruses and bacteria
- Reduces the risk of asthma, allergies, respiratory illnesses, and ear infections
- Lowers the risk of SIDS (Sudden Infant Death Syndrome)
- Promotes healthy weight gain and helps prevent obesity
- Aids in maternal postpartum recovery and reduces the risk of postpartum depression
- Decreases the mother’s risk of breast and ovarian cancer, type 2 diabetes, and heart disease
Breastfeeding Basics
Successful breastfeeding begins with understanding the fundamentals of milk production, let-down reflex, and proper positioning. These basics create the foundation for a positive breastfeeding experience for both mother and baby.
Milk Production and Let-Down Reflex
The breast contains alveoli (milk-producing cells) surrounded by myoepithelial cells that contract to eject milk. When the baby suckles, sensory nerves in the nipple send signals to the brain, stimulating the release of two key hormones:
- Prolactin: Stimulates milk production in the alveoli
- Oxytocin: Causes myoepithelial cells to contract, pushing milk through the ducts (let-down reflex)
The let-down reflex may be triggered by hearing the baby cry, thinking about the baby, or even just preparing to breastfeed. This reflex can be affected by stress, anxiety, pain, or embarrassment, which can inhibit oxytocin release.
Memory Aid: Supply and Demand Cycle
Remember that breastfeeding operates on a supply and demand principle:
- More frequent nursing → More prolactin release → Increased milk production
- Less frequent nursing → Less stimulation → Decreased milk production
The cycle maintains itself based on the infant’s feeding patterns!
Breastfeeding Positions
Various positions can be used for breastfeeding. The ideal position depends on the mother’s and baby’s comfort, the size of the mother’s breasts, and any specific circumstances (e.g., cesarean birth, twins).
| Position | Description | Best For |
|---|---|---|
| Cradle Hold | Baby’s head rests in the crook of the elbow on the same side as the breast being used, with baby’s body facing mother’s body | Most common position, good for term babies with good head control |
| Cross-Cradle Hold | Similar to cradle hold, but baby is supported by the arm opposite to the breast being used | Provides more head control for smaller babies or those with latching difficulties |
| Football Hold (Clutch Hold) | Baby’s body is tucked under the mother’s arm (like a football) with legs extending behind her | Mothers who had cesarean births, large breasts, or when nursing twins |
| Side-Lying Position | Mother and baby lie on their sides facing each other | Nighttime feedings, mothers recovering from cesarean birth |
| Laid-Back Position (Biological Nurturing) | Mother reclines at a 45-degree angle with baby placed on her chest | Encourages natural reflexes, good for babies who have difficulty latching |
Proper Latching Techniques
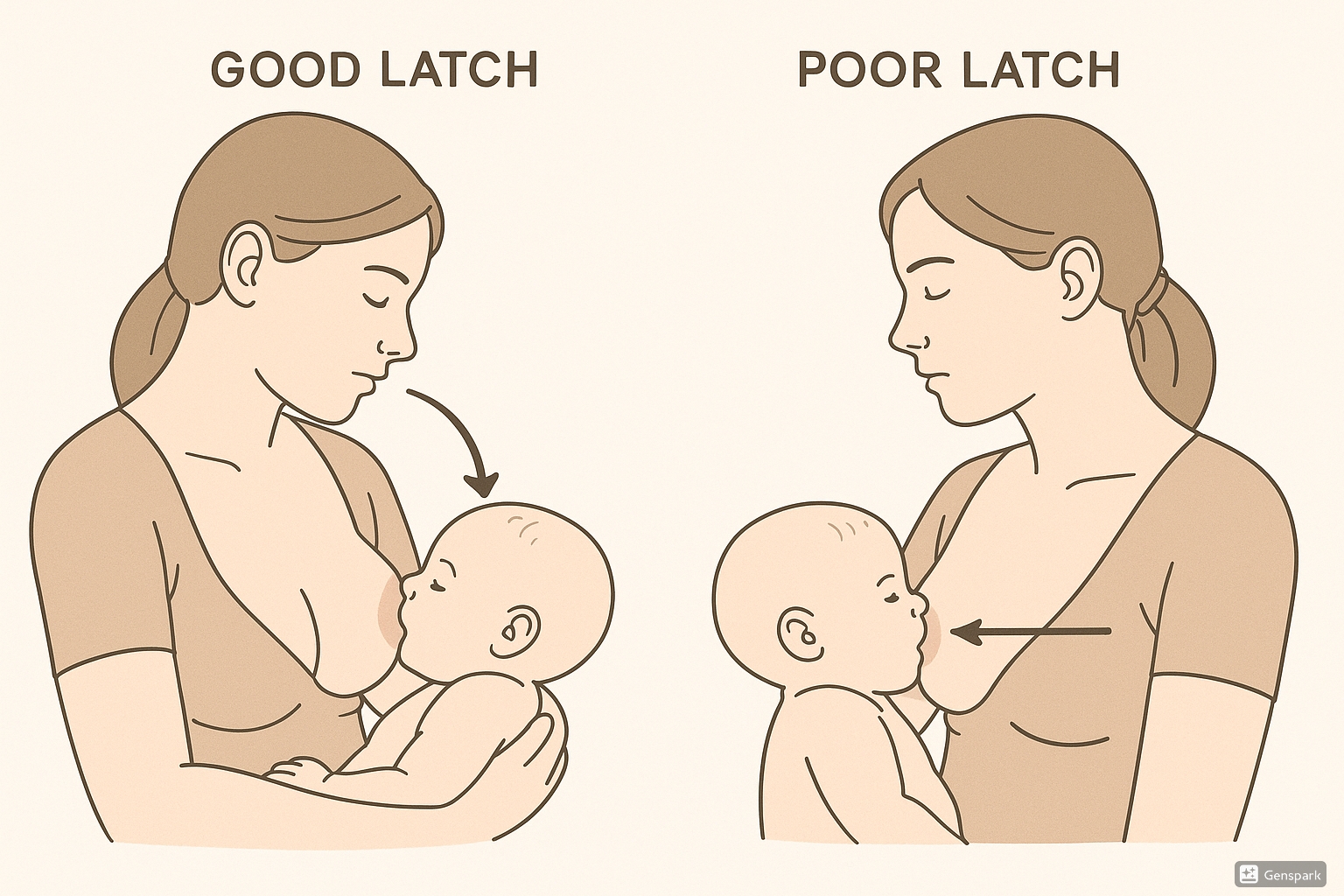
Proper breastfeeding latching techniques
A proper latch is crucial for effective breastfeeding as it allows the baby to extract milk efficiently while preventing nipple pain and damage. The latch involves the baby taking both the nipple and a significant portion of the areola into their mouth.
Steps for Achieving a Good Latch
- Position the baby with their nose aligned to the nipple
- Wait for the baby to open their mouth wide (like a yawn)
- Quickly move the baby onto the breast, ensuring they take a large portion of the areola, not just the nipple
- Ensure the baby’s chin touches the breast, with nose clear
- Check for asymmetric latch – more areola visible above the baby’s top lip than below their bottom lip
- Listen for swallowing sounds and observe rhythmic jaw movements
Memory Aid: CHIN
For proper latching, remember CHIN:
- C: Close – baby close to mother’s body
- H: Head free – baby’s head free to move, not restrained
- I: In line – baby’s ear, shoulder, and hip in straight line
- N: Nose to nipple – baby’s nose aligned with mother’s nipple
Memory Aid: CALM
For checking proper latch, remember CALM:
- C: Chin touches breast
- A: Areola (inferior half) covered
- L: Lips flanged outward
- M: Mother comfortable
Signs of a Good Latch
- Baby’s mouth covers a large portion of the areola, not just the nipple
- Baby’s lips are flanged outward (like fish lips)
- Baby’s chin indents the breast
- Baby’s cheeks are rounded, not dimpled
- Rhythmic sucking and swallowing is observed
- Mother feels pulling/tugging but not pinching or pain
- Baby remains latched without slipping off
Signs of a Poor Latch
- Clicking sounds during feeding
- Baby’s cheeks dimple or hollow inward
- Baby frequently slips off the breast
- Mother experiences pain throughout the feeding
- Nipples appear pinched, flattened, or damaged after feeding
- Baby seems unsatisfied after feeding
- Minimal swallowing is observed
Important: Persistent pain during breastfeeding is not normal and often indicates a problem with the latch. If a mother experiences continued pain despite attempts to improve the latch, refer her to a lactation consultant for specialized support.
LATCH Scoring System
The LATCH scoring system is a standardized tool used to document and assess breastfeeding sessions. Each component is assigned a score of 0, 1, or 2, with a total score ranging from 0 to 10. Higher scores indicate more effective breastfeeding.
| Component | Score 0 | Score 1 | Score 2 |
|---|---|---|---|
| L – Latch | Too sleepy or reluctant; no latch achieved | Repeated attempts; holds nipple in mouth; stimulation needed to maintain | Grasps breast; tongue down; lips flanged; rhythmic sucking |
| A – Audible swallowing | None | A few with stimulation | Spontaneous and intermittent <24 hours old; Spontaneous and frequent >24 hours old |
| T – Type of nipple | Inverted | Flat | Everted (after stimulation) |
| C – Comfort (breast/nipple) | Engorged; Cracked; Bleeding; Large blisters or bruises; Severe discomfort | Filling; Reddened; Small blisters or bruises; Mild/moderate discomfort | Soft; Non-tender |
| H – Hold (positioning) | Full assist (staff holds infant at breast) | Minimal assist (i.e., elevate head of bed; place pillows for support) | No assist from staff; Mother able to position/hold infant |
Interpreting LATCH Scores:
- 0-3: Poor, requires significant intervention
- 4-7: Moderate, some assistance needed
- 8-10: Good, minimal assistance needed
Research indicates that a LATCH score of ≥7 at 16-24 hours postpartum is associated with ongoing breastfeeding at 6 weeks.
Memory Aid: LATCHES Mnemonic
The expanded LATCHES mnemonic focuses on the principles of attachment for effective breastfeeding:
- L: Latch – how well the infant latches onto the breast
- A: Audible swallowing – amount of swallowing heard
- T: Type of nipple – mother’s nipple type (inverted, flat, everted)
- C: Comfort – mother’s level of comfort
- H: Hold – positioning assistance required
- E: Engagement – baby’s engagement with the breast
- S: Support – level of support mother needs
Common Breastfeeding Challenges
Breastfeeding challenges are common, especially in the early postpartum period. As a nursing professional, being able to identify and address these challenges can help mothers continue breastfeeding successfully.
Nipple Pain and Damage
Often caused by improper latching, which compresses the nipple against the baby’s hard palate.
- Interventions:
- Check and correct latch positioning
- Break suction properly before removing baby from breast
- Start feeding on the less sore side first
- Apply expressed breast milk or lanolin to nipples after feeding
- Allow nipples to air dry
- Change breast pads frequently
Engorgement
Occurs when breasts become overly full, usually when milk first comes in or when feedings are missed.
- Interventions:
- Breastfeed frequently (8-12 times per 24 hours)
- Apply warm compress before feeding to promote let-down
- Gently massage breasts while feeding
- Apply cold packs after feeding to reduce swelling
- Hand express or pump just enough milk to soften the areola for latching
Low Milk Supply
May be perceived or actual, can be caused by infrequent feeding, poor latch, or certain medical conditions.
- Interventions:
- Increase breastfeeding frequency
- Ensure proper latch and positioning
- Use breast compression during feeding
- Consider “power pumping” (short, frequent pumping sessions)
- Stay hydrated and maintain good nutrition
- Assess for medical conditions that may affect supply
Plugged Ducts
Occurs when a milk duct becomes blocked, causing a small, painful lump in the breast.
- Interventions:
- Continue breastfeeding, starting on the affected side
- Position baby with chin pointing toward the plug
- Apply warm compress before feeding
- Gently massage from the blocked area toward the nipple
- Wear loose clothing and properly fitted bras
Warning Sign: If symptoms of plugged ducts worsen and are accompanied by fever, body aches, and flu-like symptoms, suspect mastitis (breast infection) and refer for prompt medical evaluation. Mastitis requires antibiotic treatment while continuing to breastfeed.
Managing Postpartum Uterine Cramps
Postpartum uterine cramps, also known as afterpains, are contractions of the uterus that help it return to its pre-pregnancy size. These cramps are typically more pronounced in multiparous women and during breastfeeding due to the release of oxytocin.
Physiology of Afterpains
After delivery, the uterus must contract to:
- Return to pre-pregnancy size (involution)
- Prevent excessive bleeding by compressing blood vessels
- Expel remaining placental fragments or blood clots
Oxytocin released during breastfeeding intensifies these contractions, which is why many women notice increased cramping during nursing sessions, especially in the first few days postpartum.
Key Facts about Afterpains:
- More common and intense in multiparous women (those who’ve had previous pregnancies)
- Typically more intense during breastfeeding due to oxytocin release
- Usually most severe in the first 2-3 days postpartum
- Generally diminish in intensity by 5-7 days postpartum
- Serve an important physiological function in preventing postpartum hemorrhage
Nursing Interventions for Afterpains
| Intervention | Technique | Rationale |
|---|---|---|
| Medication Management | Administer NSAIDs (ibuprofen) or acetaminophen as ordered | NSAIDs are particularly effective as they reduce both pain and inflammation; ibuprofen is compatible with breastfeeding |
| Heat Application | Apply heating pad to lower abdomen for 15-20 minutes | Heat improves blood flow and relaxes muscles, reducing pain perception |
| Positioning | Encourage prone position when resting | Lying on stomach applies gentle pressure that helps keep the uterus contracted |
| Empty Bladder | Encourage frequent urination | Full bladder can displace uterus and interfere with contraction |
| Relaxation Techniques | Deep breathing, visualization, progressive muscle relaxation | Reduces tension and anxiety, which can exacerbate pain perception |
| Uterine Massage | Gentle massage of fundus of uterus in circular motion | Stimulates and maintains uterine tone; helps expel clots |
Memory Aid: CRAMPED
Remember these interventions for afterpain relief with CRAMPED:
- C: Comfort measures (heat, positioning)
- R: Relaxation techniques
- A: Analgesics (NSAIDs preferred)
- M: Massage uterine fundus gently
- P: Position prone when resting
- E: Empty bladder frequently
- D: Discuss normal physiological process
Patient Education Points
When teaching new mothers about afterpains, include the following information:
- Afterpains are a normal part of the healing process
- They are temporary and typically resolve within a week
- Taking pain medication 30 minutes before breastfeeding can help manage pain
- Emptying the bladder before breastfeeding may reduce discomfort
- Using a pillow to support the abdomen during breastfeeding can provide relief
- When to seek medical attention (severe pain unrelieved by medication, large clots, foul odor)
Clinical Tip: Severe afterpains that worsen or persist beyond a week may indicate retained placental fragments or infection. If a woman reports increasing pain, fever, or unusual discharge, prompt evaluation is needed.
Best Practices & Recent Updates
Stay current with the latest recommendations and guidelines for breastfeeding support and management of postpartum issues.
1. Extended Duration of Breastfeeding Recommendation
The American Academy of Pediatrics updated their breastfeeding policy in 2022, recommending:
- Exclusive breastfeeding for approximately 6 months
- Continued breastfeeding for at least 2 years (extended from previous 1-year recommendation)
- Introduction of nutritious complementary foods around 6 months
This aligns with World Health Organization recommendations and emphasizes the continued benefits of human milk beyond the first year of life.
2. Trauma-Informed Breastfeeding Support
Recent guidelines emphasize the importance of trauma-informed care in breastfeeding support:
- Recognize that past trauma may impact breastfeeding experience
- Create safe environments where mothers feel in control
- Ask permission before touching the mother or baby
- Offer multiple options and respect mother’s choices
- Use sensitive language and avoid judgment
- Provide referrals to mental health support when needed
This approach acknowledges that up to 30% of women report birth trauma, and many more have experienced other forms of trauma that may affect their breastfeeding journey.
3. Technology Integration in Breastfeeding Support
Recent advances in telehealth and digital tools have expanded breastfeeding support options:
- Virtual lactation consultations provide access to expert support regardless of location
- Mobile apps help track feeding patterns, growth, and milestones
- Online support groups connect mothers with peers and professionals
- Digital education resources provide on-demand information in multiple languages
- Wearable breast pumps and smart devices offer more flexibility for expressing milk
Evidence shows that technology-based interventions can be effective in extending breastfeeding duration and exclusivity when combined with traditional support methods.
Current Guidelines At-a-Glance (2024)
| Organization | Recommendation |
|---|---|
| World Health Organization (WHO) | Initiate breastfeeding within first hour of birth; exclusive breastfeeding for 6 months; continue breastfeeding with complementary foods for up to 2 years or beyond |
| American Academy of Pediatrics (AAP) | Exclusive breastfeeding for about 6 months; continued breastfeeding as complementary foods are introduced for 2 years or longer |
| American College of Obstetricians and Gynecologists (ACOG) | Supports continued breastfeeding while complementary foods are introduced, as long as mutually desired by mother and infant |
| Centers for Disease Control and Prevention (CDC) | Exclusive breastfeeding for about the first 6 months with continued breastfeeding while introducing appropriate complementary foods until children are 12 months or older |
Additional Resources
For continued learning and support, the following resources are recommended:
Professional Organizations
- International Lactation Consultant Association (ILCA): www.ilca.org
- Academy of Breastfeeding Medicine: www.bfmed.org
- La Leche League International: www.llli.org
- United States Breastfeeding Committee: www.usbreastfeeding.org
Clinical Tools and Guidelines
- CDC Breastfeeding Guidelines: www.cdc.gov/breastfeeding/recommendations
- WHO Breastfeeding Resources: www.who.int/health-topics/breastfeeding
- AAP Policy Statement on Breastfeeding: www.aap.org/breastfeeding
Patient Education Materials
- Office on Women’s Health: www.womenshealth.gov/breastfeeding
- HealthyChildren.org (AAP): www.healthychildren.org/breastfeeding
- WIC Breastfeeding Support: wicbreastfeeding.fns.usda.gov
