PROTEINS: Comprehensive Nursing Notes
Building Blocks of Life – Essential Knowledge for Nursing Practice
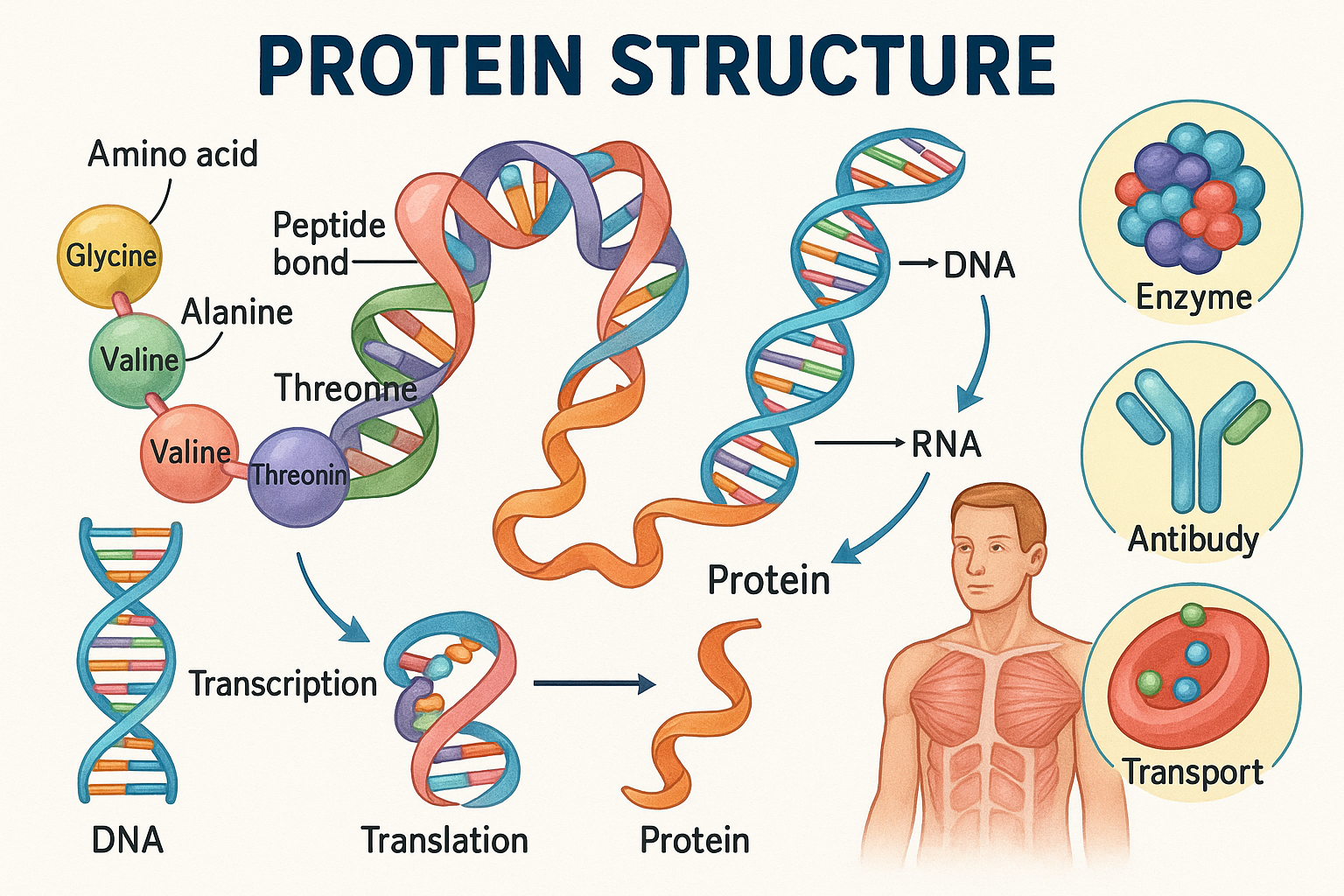
Figure 1: Protein structure showing amino acid composition, peptide bonds, and various cellular functions
Introduction to Proteins
Proteins are complex macromolecules that serve as the fundamental building blocks of life. As a nursing professional, understanding protein structure, function, and metabolism is crucial for providing optimal patient care, particularly in nutrition assessment, wound healing, immune function, and overall health maintenance. This comprehensive guide will equip you with essential knowledge about proteins and their clinical applications in nursing practice.
Why Proteins Matter in Nursing
- Essential for tissue repair and wound healing
- Critical component of immune system function
- Vital for medication transport and enzyme activity
- Key factor in fluid balance and acid-base regulation
- Important for muscle strength and patient mobility
Protein Composition
Basic Structure
- Carbon (C): 50-55%
- Oxygen (O): 20-25%
- Nitrogen (N): 15-17%
- Hydrogen (H): 6-8%
- Sulfur (S): 1-3%
Molecular Structure
Proteins are polymers composed of amino acids linked by peptide bonds. The unique sequence and arrangement of amino acids determine the protein’s structure and function.
Protein Structure Hierarchy
Primary
Amino acid sequence
Secondary
α-helices, β-sheets
Tertiary
3D folding
Quaternary
Multi-subunit
Clinical Significance
Understanding protein structure is essential for nurses because structural changes can affect protein function. Factors like pH, temperature, and medications can cause protein denaturation, impacting patient care outcomes. For example, albumin’s structural integrity affects its ability to maintain oncotic pressure and transport medications.
Eight Essential Amino Acids
Memory Aid – “PVT TIM HALL”
Phenylalanine, Valine, Threonine, Tryptophan, Isoleucine, Methionine, Histidine, Arginine, Lysine, Leucine
Note: Originally 8 essential amino acids, but Histidine and Arginine are now considered essential for infants and during illness/stress.
Phenylalanine
Function: Precursor to tyrosine, dopamine, norepinephrine
Sources: Meat, fish, eggs, dairy, nuts
Nursing Note: Monitor in PKU patients
Valine
Function: Muscle metabolism, energy production
Sources: Dairy, meat, grains, mushrooms
Nursing Note: Important for wound healing
Threonine
Function: Collagen formation, immune function
Sources: Turkey, fish, lentils, sesame seeds
Nursing Note: Critical for skin integrity
Tryptophan
Function: Serotonin synthesis, sleep regulation
Sources: Turkey, chicken, cheese, fish
Nursing Note: Affects mood and sleep patterns
Isoleucine
Function: Muscle energy, hemoglobin formation
Sources: Meat, fish, eggs, almonds
Nursing Note: Important for blood sugar regulation
Methionine
Function: Methylation reactions, detoxification
Sources: Fish, meat, dairy, Brazil nuts
Nursing Note: Essential for liver function
Leucine
Function: Protein synthesis, muscle maintenance
Sources: Meat, dairy, eggs, soybeans
Nursing Note: Prevents muscle wasting
Lysine
Function: Collagen synthesis, calcium absorption
Sources: Meat, fish, dairy, legumes
Nursing Note: Important for bone health
Clinical Considerations
Essential amino acids cannot be synthesized by the body and must be obtained from dietary sources. Deficiencies can lead to impaired wound healing, compromised immune function, and muscle wasting. As a nurse, assess patients for adequate protein intake, especially in vulnerable populations such as elderly patients, those with chronic illnesses, or patients with increased metabolic demands.
Protein Functions
Structural
Collagen in connective tissues, keratin in skin and hair, elastin in blood vessels
Enzymatic
Catalyze biochemical reactions, including digestion, metabolism, and cellular processes
Transport
Hemoglobin carries oxygen, albumin transports medications and nutrients
Defense
Antibodies, complement proteins, and antimicrobial peptides
Regulation
Hormones like insulin, growth hormone, and thyroid hormones
Fluid Balance
Maintain oncotic pressure and acid-base balance
Protein Synthesis Pathway
DNA
Genetic Code
Transcription
mRNA Formation
Translation
Ribosome Assembly
Protein
Functional Product
Nursing Applications of Protein Functions
Assessment Focus:
- Albumin levels for nutritional status
- Hemoglobin for oxygen transport
- Immunoglobulin levels for immune function
- Prealbumin for acute nutritional changes
Intervention Considerations:
- Wound healing requires adequate protein
- Medication binding affected by albumin levels
- Fluid balance depends on protein concentration
- Enzyme function affects medication metabolism
Dietary Sources of Proteins
Complete Proteins
Contain all essential amino acids in adequate proportions
- Animal Sources:
- • Meat (beef, pork, lamb): 20-25g per 100g
- • Poultry (chicken, turkey): 18-25g per 100g
- • Fish and seafood: 18-22g per 100g
- • Eggs: 12g per 100g
- • Dairy products: 3-35g per 100g
Incomplete Proteins
Lack one or more essential amino acids
- Plant Sources:
- • Legumes (beans, lentils): 8-25g per 100g
- • Nuts and seeds: 5-21g per 100g
- • Grains: 2-14g per 100g
- • Vegetables: 1-4g per 100g
- • Soy products: 10-16g per 100g
Protein Complementation
Combining incomplete proteins to create complete amino acid profiles
Rice + Beans
Rice provides methionine, beans provide lysine
Peanut Butter + Bread
Complementary amino acid profiles
Hummus + Pita
Chickpeas + wheat combination
High Biological Value
Proteins easily absorbed and utilized
- • Eggs (100)
- • Milk (85)
- • Fish (75)
- • Beef (70)
Medium Biological Value
Moderately efficient utilization
- • Soy (65)
- • Rice (60)
- • Wheat (55)
- • Corn (50)
Special Considerations
Factors affecting protein quality
- • Processing methods
- • Digestibility
- • Anti-nutritional factors
- • Individual variations
Nursing Implementation: Dietary Assessment
Assessment Strategies:
- 24-hour dietary recall
- Food frequency questionnaires
- Anthropometric measurements
- Laboratory protein markers
- Clinical signs of deficiency
Patient Education Focus:
- Importance of complete proteins
- Protein complementation techniques
- Portion size guidelines
- Special dietary needs
- Budget-friendly protein sources
Protein Requirements – RDA (Recommended Daily Allowance)
Standard RDA Formula
0.8 g protein per kg body weight per day
For healthy adults (age 19 and older)
| Population Group | Age Range | Protein Requirement (g/kg/day) | Additional Notes |
|---|---|---|---|
| Infants | 0-6 months | 1.52 | Based on breast milk composition |
| Infants | 7-12 months | 1.5 | Transitioning to solid foods |
| Children | 1-3 years | 1.1 | Rapid growth phase |
| Children | 4-8 years | 0.95 | Continued growth |
| Children | 9-13 years | 0.95 | Pre-adolescent development |
| Adolescents | 14-18 years | 0.85 | Growth spurts and development |
| Adults | 19+ years | 0.8 | Maintenance of body tissues |
| Pregnancy | All trimesters | 1.1 | Fetal development and maternal changes |
| Lactation | 0-12 months | 1.3 | Milk production requirements |
| Elderly | 65+ years | 1.0-1.2 | Prevent sarcopenia |
Increased Protein Needs
Trauma, burns, sepsis
Surgical patients, pressure ulcers
Pre-dialysis patients
Hemodialysis patients
Clinical Considerations
Risk of hepatic encephalopathy
Prevent refeeding syndrome
Endurance and strength training
Lower protein digestibility
Memory Aid for Protein Assessment – “MEALS”
Protein Calculation Examples
Example 1: Healthy Adult
Patient: 70 kg adult
Calculation: 70 kg × 0.8 g/kg = 56 g/day
Distribution: ~19 g per meal
Example 2: Critically Ill
Patient: 70 kg burn patient
Calculation: 70 kg × 1.5 g/kg = 105 g/day
Distribution: ~35 g per meal
Nursing Implementation and Clinical Applications
Assessment Parameters
- Weight changes
- Mid-arm circumference
- Triceps skinfold thickness
- Body mass index (BMI)
- Albumin (3.5-5.0 g/dL)
- Prealbumin (15-35 mg/dL)
- Transferrin (200-400 mg/dL)
- Total protein (6.0-8.0 g/dL)
Physical Assessment
- Muscle wasting
- Delayed wound healing
- Edema (hypoproteinemia)
- Brittle hair and nails
- Immune dysfunction
- Fatigue and weakness
- Poor appetite
- Slow recovery from illness
- Increased infection risk
Nursing Process for Protein Management
Assessment
Nutritional status, lab values, intake
Diagnosis
Identify protein-related issues
Planning
Set protein goals, interventions
Implementation
Execute interventions, monitor
Evaluation
Assess outcomes, adjust plan
High-Risk Populations
- • Elderly patients
- • Chronic disease patients
- • Post-operative patients
- • Burn victims
- • Cancer patients
- • Patients with malabsorption
- • Vegetarians/vegans
Interventions
- • Dietary counseling
- • Protein supplementation
- • Enteral nutrition
- • Parenteral nutrition
- • Meal planning assistance
- • Appetite stimulation
- • Coordination with dietitian
Monitoring Parameters
- • Daily weight changes
- • Food intake records
- • Wound healing progress
- • Infection rates
- • Functional capacity
- • Laboratory trends
- • Patient satisfaction
Nursing Diagnoses Related to Protein
Primary Diagnoses:
- Imbalanced nutrition: less than body requirements
- Risk for impaired skin integrity
- Delayed surgical recovery
- Risk for infection
- Fatigue related to inadequate protein intake
Expected Outcomes:
- Patient maintains adequate protein intake
- Wound healing progresses as expected
- Laboratory values remain within normal limits
- Patient demonstrates understanding of protein needs
- No signs of protein deficiency develop
Key Nursing Considerations
Patient Education:
- Importance of protein in healing and recovery
- Identification of high-quality protein sources
- Proper portion sizes and meal timing
- Signs and symptoms of protein deficiency
- Strategies for increasing protein intake
Interdisciplinary Collaboration:
- Registered dietitian consultation
- Physician communication about protein needs
- Pharmacist consultation for supplements
- Social worker for economic barriers
- Family involvement in meal planning
Key Takeaways for Nursing Practice
Essential Knowledge
- • Proteins are essential for tissue repair and immune function
- • Eight essential amino acids must be obtained from diet
- • Complete proteins contain all essential amino acids
- • RDA is 0.8 g/kg/day for healthy adults
- • Increased needs in illness, pregnancy, and growth
- • Monitor albumin, prealbumin, and clinical signs
Clinical Applications
- • Assess protein status in all patients
- • Identify high-risk populations early
- • Collaborate with dietitians for optimal care
- • Educate patients about protein importance
- • Monitor response to interventions closely
- • Document protein intake and outcomes
Final Memory Aid – “PROTEIN”
References and Further Reading
1. Institute of Medicine. Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein, and Amino Acids. Washington, DC: National Academy Press; 2005.
2. American Dietetic Association. Position Paper: Vegetarian Diets. J Am Diet Assoc. 2016;116:1970-1980.
3. Wolfe RR. The role of dietary protein in optimizing muscle mass, function and health outcomes in older individuals. Br J Nutr. 2012;108:S88-S93.
4. Bauer J, Biolo G, Cederholm T, et al. Evidence-based recommendations for optimal dietary protein intake in older people. J Am Med Dir Assoc. 2013;14:542-559.
5. McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient. J Parenter Enteral Nutr. 2016;40:159-211.
