Community Health Nursing: Records Management and Maternal Care Essentials
A comprehensive guide for nursing students on maintenance of records, safe childbirth procedures, and labor room organization
Table of Contents
Introduction
Community health nursing plays a pivotal role in maternal and child health, particularly in ensuring safe childbirth and effective postpartum care. This comprehensive guide focuses on four essential components that every nursing professional should master: maintenance of records and reports, implementation of the WHO Safe Childbirth Checklist, understanding the Skilled Birth Attendant (SBA) module, and proper organization of labor rooms.
Effective maternal care requires meticulous attention to detail and adherence to established protocols. The expertise of community health nurses in these areas directly impacts maternal and newborn outcomes, particularly in resource-limited settings where access to specialized facilities may be limited.
Why This Matters: According to the World Health Organization, approximately 295,000 women died during and following pregnancy and childbirth in 2017. The majority of these deaths were preventable with proper care and adherence to established protocols, highlighting the critical importance of skilled nursing care in maternal health services.
1. Maintenance of Records and Reports
1.1 Importance of Record Keeping
Accurate and comprehensive record keeping is the foundation of quality healthcare delivery in community settings. Records serve as both legal documents and essential tools for continuity of care, particularly during maternal health services where multiple healthcare providers may be involved in a woman’s care during pregnancy, childbirth, and postpartum periods.
Key Functions of Health Records in Maternal Care
- Documentation of care provided and health status
- Communication tool between healthcare providers
- Quality assurance and improvement mechanism
- Legal protection for both patients and providers
- Resource for research and health planning
- Evaluation of healthcare services and outcomes
1.2 Types of Records in Community Health
Community health nurses are responsible for maintaining various types of records to ensure comprehensive maternal care throughout pregnancy, childbirth, and postpartum periods.
| Record Type | Description | Purpose |
|---|---|---|
| Antenatal Records | Documentation of pregnancy progression, risk assessments, and interventions | Monitor maternal and fetal health, identify risks early |
| Partograph | Graphical record of labor progress and maternal-fetal condition | Early detection of abnormal labor patterns and complications |
| Birth Records | Details of childbirth including mode of delivery, complications, and interventions | Legal documentation, quality monitoring |
| Postnatal Records | Documentation of maternal recovery and newborn condition | Ensure appropriate follow-up care |
| Referral Records | Documentation of patient transfers between facilities | Ensure continuity of care during referrals |
| Family Planning Records | Documentation of counseling and method provision | Track uptake and continuation of family planning services |
| Home Visit Records | Documentation of community-based care | Ensure continuity of care between facility and home |
| Immunization Records | Documentation of maternal and infant immunizations | Track immunization coverage and due dates |
1.3 Principles of Record Maintenance
The community health nurse should adhere to the following principles when maintaining maternal health records:
ACCURATE: Principles of Record Maintenance
A – Accurate and factual information only
C – Complete documentation of all care provided
C – Clear and concise entries with standard terminology
U – Up-to-date entries made promptly after care
R – Relevant information that impacts care decisions
A – Authenticated with name, date, and signature
T – Timely completion without delays
E – Error correction with proper procedure (single line through error, initial, date)
Storage and Maintenance Guidelines
- Store records in a clean, secure space protected from damage
- Develop a systematic filing method (alphabetical or numerical)
- Ensure confidentiality and limit access to authorized personnel
- Establish retention periods according to legal requirements
- Create backup systems for electronic records
- Regularly audit records for completeness and accuracy
1.4 Reporting Systems
Reports are essential communication tools in community health nursing that summarize data from individual records to inform program planning, resource allocation, and evaluation of maternal care services.
Common Types of Reports in Maternal Health
| Report Type | Frequency | Key Contents |
|---|---|---|
| Daily Delivery Report | Daily | Number of deliveries, complications, referrals |
| Maternal Death Review | As needed | Case analysis, contributing factors, preventive measures |
| Monthly Activity Report | Monthly | Summary of services provided, coverage indicators |
| Immunization Report | Monthly | Coverage rates, stock status, adverse events |
| Facility Utilization Report | Quarterly | Service statistics, bed occupancy, referral patterns |
| Birth Registration Report | Monthly | Birth statistics, gender distribution, birth weight categories |
Note: Timely reporting is crucial for early identification of trends and prompt intervention. Delayed reporting can lead to missed opportunities for corrective action, especially in cases of maternal complications or disease outbreaks.
Electronic Health Records in Community Settings
Many facilities are transitioning from paper-based to electronic health record (EHR) systems. Community health nurses should be familiar with both systems and understand the transition process.
Benefits of Electronic Records for Maternal Care
- Improved access to patient information
- Enhanced data accuracy and completeness
- Better tracking of maternal care continuity
- Automated alerts for high-risk conditions
- Simplified reporting and data analysis
- Reduced storage space requirements
- Facilitated sharing of information between facilities
2. Safe Childbirth Checklist
2.1 Introduction to WHO Safe Childbirth Checklist
The World Health Organization (WHO) Safe Childbirth Checklist is a tool designed to improve the quality of care provided to women during labor, delivery, and the immediate postpartum period. It helps healthcare providers remember essential practices that prevent the major causes of maternal and neonatal mortality.
Purpose of the WHO Safe Childbirth Checklist: This tool aims to reduce maternal and neonatal mortality by ensuring healthcare providers follow evidence-based practices at critical points during childbirth. It provides a systematic approach to care that can be implemented in various resource settings.
2.2 Stages of Childbirth Checklist
The WHO Safe Childbirth Checklist is divided into four pause points, each corresponding to a critical moment in maternal care when checks and interventions can prevent complications.
Pause Point 1: On Admission
Pause Point 2: Just Before Pushing (or Before Caesarean)
Pause Point 3: Soon After Birth (Within 1 Hour)
Pause Point 4: Before Discharge
MOTHER: Danger Signs to Watch For
M – Massive bleeding or increased vaginal discharge
O – Overwhelming pain (severe abdominal pain, headache, visual disturbances)
T – Temperature elevated (fever or chills)
H – Hypertension symptoms (headache, blurred vision, epigastric pain)
E – Elimination problems (difficulty emptying bladder)
R – Respiratory difficulty (breathing problems)
NEWBORN: Danger Signs in Baby
N – Not feeding well
E – Excessive crying or irritability
W – Warm (fever) or too cold (hypothermia)
B – Breathing fast/difficulty
O – Overall activity reduced
R – Redness or discharge from umbilicus
N – Noticeable yellow skin (jaundice)
2.3 Implementation in Community Settings
Successfully implementing the WHO Safe Childbirth Checklist in community health settings requires a systematic approach and adaptation to local contexts.
Implementation Steps
- Engage stakeholders – Involve facility leadership, healthcare providers, and community representatives
- Assess current practices – Identify gaps in existing maternal care protocols
- Adapt the checklist – Modify to fit local context while maintaining essential elements
- Train healthcare providers – Ensure all staff understand the purpose and use of the checklist
- Introduce the checklist gradually – Begin with pilot implementation and expand
- Monitor implementation – Regularly assess adherence and address barriers
- Provide supportive supervision – Offer coaching and mentorship to staff
- Evaluate outcomes – Measure impact on maternal and newborn health outcomes
Common Implementation Challenges:
- Resistance to change among healthcare providers
- Time constraints in busy facilities
- Lack of essential supplies and medications
- Insufficient training and supportive supervision
- Poor integration with existing documentation systems
2.4 Benefits and Outcomes
The WHO Safe Childbirth Checklist, when properly implemented, offers numerous benefits for maternal and newborn care.
| Benefit | Description |
|---|---|
| Standardized Care | Ensures consistency in applying evidence-based practices during childbirth |
| Improved Communication | Enhances teamwork and information sharing among healthcare providers |
| Early Detection of Complications | Prompts systematic assessment for early identification of problems |
| Reduced Maternal Mortality | Addresses major causes of maternal death through preventive measures |
| Reduced Neonatal Mortality | Promotes essential newborn care practices that prevent complications |
| Quality Improvement | Provides data for monitoring and improving facility performance |
| Empowered Healthcare Providers | Builds confidence among staff in managing childbirth complications |
Research Evidence: Studies have shown that implementing the WHO Safe Childbirth Checklist can improve adherence to essential birth practices. For example, a study in India found significant improvements in practices such as partograph use, antibiotic administration, and postpartum hemorrhage prevention measures after implementing the checklist with proper coaching.
3. Skilled Birth Attendant (SBA) Module Review
3.1 Definition and Role of SBA
A Skilled Birth Attendant (SBA) is defined by the World Health Organization as “an accredited health professional—such as a midwife, doctor, or nurse—who has been educated and trained to proficiency in the skills needed to manage normal (uncomplicated) pregnancies, childbirth, and the immediate postnatal period, and in the identification, management, and referral of complications in women and newborns.”
Key Point: Skilled attendance at birth requires two essential components: a skilled birth attendant and an enabling environment that includes drugs and equipment, a functional referral system, and supportive policies.
Essential Roles of Skilled Birth Attendants
- Provide care during normal labor and childbirth
- Identify and manage or refer complications during pregnancy, childbirth, and postpartum period
- Provide essential care to newborns
- Provide health education and counseling to women and families
- Maintain accurate records of maternal care
- Collaborate with other healthcare providers for optimal care
3.2 Essential Competencies
Skilled Birth Attendants must possess specific competencies to effectively manage childbirth and address potential complications. These competencies are categorized into signal functions of Emergency Obstetric Care (EOC).
| Signal Function | Description |
|---|---|
| Administration of Parenteral Antibiotics | Ability to administer injectable antibiotics for maternal infections |
| Administration of Uterotonic Drugs | Ability to administer drugs like oxytocin to prevent/treat postpartum hemorrhage |
| Administration of Anticonvulsants | Ability to administer magnesium sulfate for pre-eclampsia/eclampsia |
| Manual Removal of Placenta | Skill to manually extract a retained placenta |
| Removal of Retained Products | Ability to remove retained placental fragments |
| Assisted Vaginal Delivery | Skill to perform vacuum extraction or forceps delivery |
| Neonatal Resuscitation | Ability to resuscitate newborns using bag and mask |
Competency Gap: Research from South Asian countries shows that while most SBAs perform administration of parenteral antibiotics, oxytocics, and neonatal resuscitation, there are significant gaps in the provision of other signal functions. Many nursing cadres are not trained or authorized to perform manual removal of placenta, removal of retained products of conception, and assisted vaginal delivery, which are often provided only by medical doctors.
PRACTICE: Essential SBA Competencies
P – Prevent complications through early recognition
R – Respond quickly to obstetric emergencies
A – Administer appropriate medications correctly
C – Clean birth practices and infection prevention
T – Track labor progress using partograph
I – Identify warning signs promptly
C – Communicate effectively with women and team
E – Ensure comprehensive postpartum care
3.3 Training Modules and Approach
SBA training modules are designed to equip healthcare providers with the knowledge and skills needed to provide safe childbirth services. The training follows a structured approach to ensure competency in all required areas.
Key Components of SBA Training Modules
- Theoretical Knowledge – Comprehensive understanding of normal and complicated pregnancy, childbirth, and postpartum care
- Practical Skills – Hands-on practice of essential procedures using models and simulations
- Clinical Practice – Supervised experience in actual care settings
- Communication Skills – Effective interaction with women, families, and other healthcare providers
- Record Keeping – Proper documentation of care provided
- Continuing Education – Regular updates on new evidence and best practices
Training Duration by Provider Type (South Asia Example)
| Provider Cadre | Base Education | Additional SBA Training |
|---|---|---|
| Obstetrician-Gynecologist | 5 years MBBS + 3-4 years specialization | None (already qualified) |
| Medical Officer with O&G training | 5 years MBBS | 6 months-1 year EOC training |
| Staff Nurse | 3-4 years nursing | Additional SBA modules |
| Auxiliary Nurse Midwife | 18 months-2 years | Additional SBA modules |
| Community SBA | Varies | 6-18 months |
3.4 Challenges and Solutions
Despite the importance of skilled birth attendance, several challenges affect the effectiveness of SBAs in community settings.
Key Challenges in SBA Implementation
| Challenge | Potential Solutions |
|---|---|
| Inadequate training in emergency obstetric functions | Enhanced “skills and drills” practical training, regular refresher courses |
| Legal and regulatory barriers | Review and revise scope of practice regulations, formalize task-shifting |
| Lack of supportive environment | Ensure adequate equipment, supplies, and functional referral systems |
| Low retention in rural areas | Provide incentives, improve living/working conditions, career advancement |
| Inadequate supervision | Establish mentorship programs, regular supportive supervision |
| Poor coordination between different cadres | Team-based training, clear referral protocols, joint case reviews |
Task Shifting: In areas with shortages of medical doctors, task shifting is an effective strategy to expand the number of healthcare providers able to perform essential childbirth services. This involves training nurses, midwives, and other non-physician providers to perform functions traditionally done by physicians. Evidence shows that with proper training and supervision, this approach can improve maternal and newborn outcomes.
4. Organization of Labor Room
4.1 Layout and Design
The labor room is a critical facility where childbirth takes place and requires careful organization to ensure safe maternal and newborn care. Proper layout and design considerations are essential for optimal functioning.
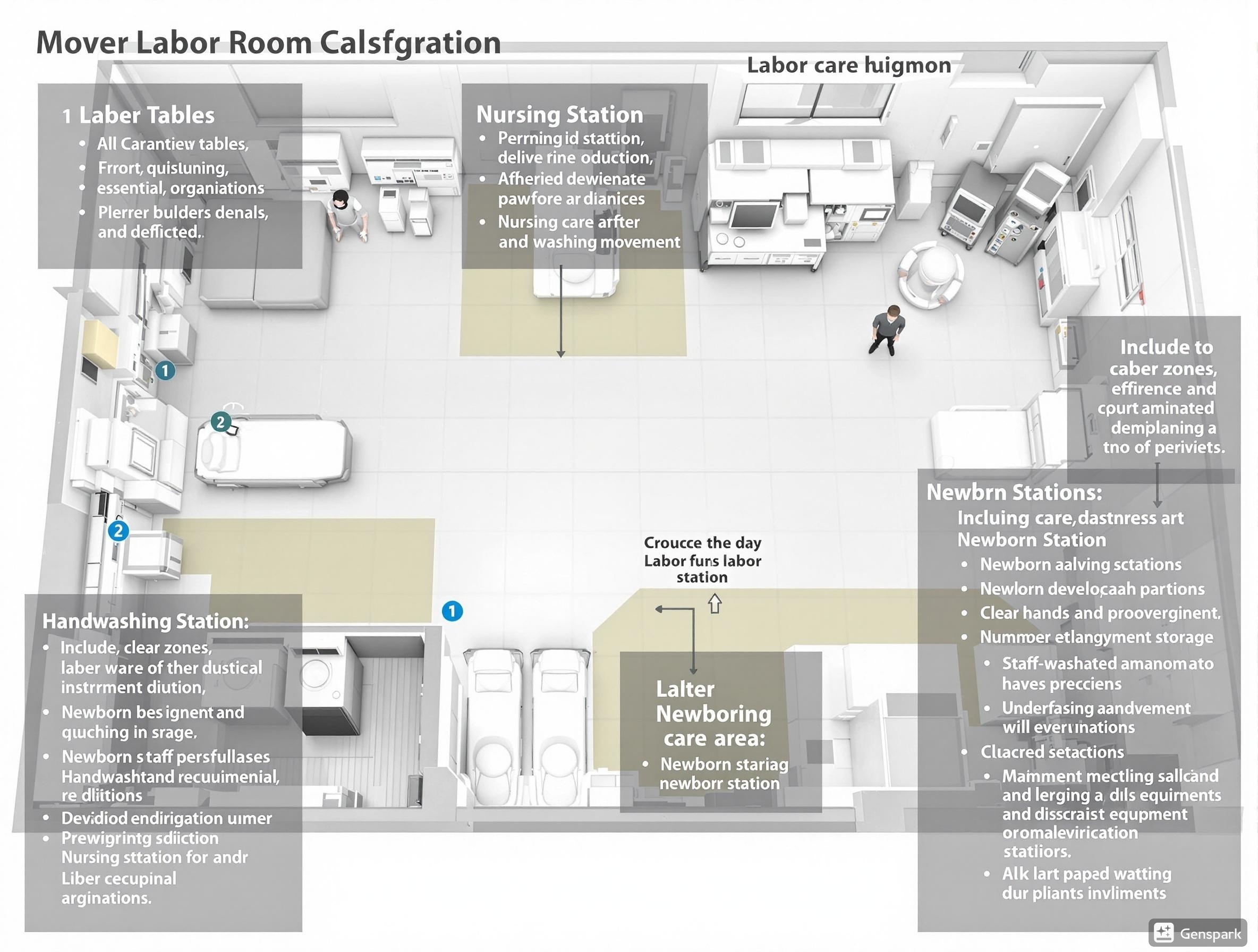
Figure 1: Detailed layout of a modern labor room showing essential zones and equipment placement
Labor Room Models
There are two primary models for labor room organization:
Labor Room Models
- Labor-Delivery-Recovery (LDR) Room: A comprehensive space where a woman remains throughout labor, delivery, and the immediate postpartum period (typically 4 hours). This client-centered approach provides continuity of care and enhanced privacy.
- Conventional Labor Room: A woman is admitted to this room at or near full cervical dilation and is moved to a postpartum ward approximately 2 hours after delivery.
Essential Zones in a Labor Room
A well-organized labor room should include the following zones:
| Zone | Description and Requirements |
|---|---|
| Labor Area | Minimum 10’×10′ per labor table with privacy provisions (curtains/partitions), adequate lighting and ventilation |
| Nursing Station | Centrally located with visibility of labor areas, equipped with documentation space and communication facilities |
| Newborn Care Area (NBCA) | Dedicated space for immediate newborn care and resuscitation if needed, equipped with radiant warmer, resuscitation equipment |
| Handwashing Area | Steel sink with elbow-operated taps, soap dispensers, and posted handwashing protocols |
| Utility Areas | Clean utility area for sterile supplies and dirty utility area for used items |
| Toilet Facilities | Western-style toilet, wash basin, and external window for ventilation |
General Design Specifications
- Walls: White wall tiles (1’×1.3′) with seamless joints extending to ceiling
- Floors: Anti-skid vitrified tiles or natural stone (2’×2′) with seamless joints
- Doors: 4’×7′ wooden doors with two frames
- Windows: 3’×2.5′ with sliding panels (part fixed with mesh, part movable with frosted glass)
- Lighting: 500 Lx for labor areas, additional focus lights for procedures
- Ventilation: Air handling unit ensuring 6 air changes per hour
- Power supply: Reliable backup system (preferably solar-powered)
4.2 Essential Equipment
A well-equipped labor room is essential for providing safe childbirth services. The equipment can be categorized based on different aspects of care.
EQUIPPED: Labor Room Essentials
E – Emergency drugs and supplies readily accessible
Q – Quality equipment in good working condition
U – Universal precautions supplies (gloves, masks, aprons)
I – Instruments for delivery and episiotomy properly sterilized
P – Partograph forms and documentation materials
P – Protective gear for staff safety
E – Equipment for newborn resuscitation
D – Delivery table with appropriate features
Labor Table Specifications
Each labor bed should meet these specifications:
- Adjustable side rails
- Facilities for Trendelenburg/reverse positions
- Height adjustment (preferably hydraulic pump)
- Stainless steel IV rod
- Mobility: swiveling castor wheels & brakes
- Three-part mattress that is waterproof and washable
- Steel basin attachments
- Calf support, hand grip, leg support
Essential Equipment by Category
| Category | Essential Items |
|---|---|
| Maternal Care | BP apparatus, stethoscope, fetoscope/Doppler, thermometer, IV stands, autoclaved delivery sets |
| Newborn Care | Radiant warmer, resuscitation kit with bag and mask, mucus extractor, pre-warmed receiving towels, shoulder roll, pediatric stethoscope |
| Emergency Equipment | Crash trolley with emergency drug trays, oxygen cylinder/concentrator, suction apparatus, adult resuscitation equipment |
| Infection Control | Hand washing station, autoclave/sterilizer, puncture-proof containers, color-coded waste bins, cleaning supplies |
| Documentation | Partograph charts, case sheets, registers, referral forms, birth certificates |
Essential Trays in Labor Room
Each labor room should have crash trolleys loaded with at least five trays:
- Delivery Tray: Sterile gloves, cord clamp, episiotomy scissors, artery forceps, dissecting forceps, sponge holding forceps, cord cutting scissors
- Episiotomy Tray: Sterile gloves, sponge holding forceps, dissecting forceps, needle holder, suture materials, gauze pieces
- Baby Tray: Baby receiving towel, cord clamp, mucus extractor, baby identification tag
- Normal Drug Tray: Syringes, needles, oxytocin, IV fluids, antiseptic solutions
- Emergency Drug Tray: Magnesium sulfate, calcium gluconate, antihypertensives, antibiotics, anticonvulsants
4.3 Staffing Requirements
Adequate staffing is crucial for providing quality care during childbirth. The number and type of staff required depend on the facility level and delivery load.
Recommended Staffing Pattern
| Facility Level | Delivery Load | Medical Officer | Staff Nurse/ANM | Support Staff |
|---|---|---|---|---|
| Primary Health Center | <20 deliveries/month | 1 (on call) | 1 per shift | 1 |
| Community Health Center | 20-100 deliveries/month | 1 (on site) | 2 per shift | 1-2 |
| First Referral Unit | 100-200 deliveries/month | 1 MO + 1 Specialist (on call) | 3 per shift | 2 |
| District Hospital | >200 deliveries/month | 1 MO + 1 Specialist (on site) | 4-6 per shift | 3-4 |
Skill Mix: Ensuring the right mix of skills is as important as having adequate numbers of staff. In each shift, there should be at least one staff member trained in newborn resuscitation and one trained in management of obstetric complications.
Role Delineation
Clear role delineation among staff members is essential for efficient functioning of a labor room:
- Medical Officer/Obstetrician: Overall supervision, management of complications, performing interventions like assisted delivery
- Staff Nurse/ANM: Monitoring labor progress, conducting normal deliveries, initial newborn care, documentation
- Pediatrician/Trained Staff: Newborn resuscitation and management of newborn complications
- Support Staff: Maintaining cleanliness, assisting with patient transport, managing supplies
4.4 Protocols and Procedures
Standard protocols and procedures are essential for ensuring quality care during childbirth. These should be prominently displayed in the labor room and regularly updated.
Essential Protocols for Labor Room
- Admission Protocol: Criteria for admission, initial assessment, documentation
- Labor Monitoring Protocol: Use of partograph, frequency of monitoring
- Infection Prevention Protocol: Hand hygiene, use of personal protective equipment, waste management
- Normal Delivery Protocol: Steps for conducting normal delivery, active management of third stage of labor
- Newborn Care Protocol: Essential newborn care, resuscitation steps
- Emergency Management Protocols: PPH, eclampsia, obstructed labor, newborn asphyxia
- Referral Protocol: Indications for referral, documentation, communication
CLEAN: Infection Prevention in Labor Room
C – Clean hands before and after procedures
L – Linen should be changed immediately after each delivery
E – Equipment must be properly sterilized
A – Aseptic techniques for all invasive procedures
N – Needle safety and proper waste disposal
Documentation Requirements: Proper documentation is a critical aspect of labor room management. All labor room procedures and interventions must be documented in:
- Case sheets/patient records
- Partograph for labor monitoring
- Birth register
- Referral forms when applicable
- Birth certificates
5. Best Practices and Global Initiatives
Several global initiatives and best practices have emerged to improve maternal and newborn care during childbirth. These approaches can be adapted to local contexts to enhance the quality of care.
Innovative Approaches in Different Regions
| Region/Country | Initiative | Key Features |
|---|---|---|
| Rwanda | Mentorship Model | Experienced providers mentor less experienced SBAs in rural facilities to improve skills in emergency obstetric care |
| Bangladesh | Community SBA Program | Training community-based providers for safe home deliveries with strong referral linkages |
| India | LaQshya Initiative | Quality improvement approach for labor rooms and maternity operation theaters with certification system |
| Kenya | Beyond Zero Campaign | Mobile clinics bringing maternal care services to remote communities |
| Nepal | Aama Program | Combines free delivery care with cash incentives for facility births |
Technology Innovations
Technology is increasingly being integrated into maternal care to improve outcomes:
- Mobile Health Applications: Digital partographs, decision support tools, and referral coordination
- Telemedicine: Remote consultation for complicated cases in rural settings
- Low-Cost Devices: Non-pneumatic anti-shock garments, portable ultrasound devices, and solar-powered equipment
- Electronic Health Records: Improved tracking of maternal care continuity
Respectful Maternity Care: Beyond clinical care, there is growing recognition of the importance of respectful maternity care during childbirth. This approach emphasizes women’s dignity, privacy, and autonomy during labor and delivery. Evidence shows that respectful care improves women’s satisfaction, increases facility-based deliveries, and contributes to better maternal and newborn outcomes.
6. Conclusion
Quality maternal and newborn care during childbirth requires a comprehensive approach that integrates proper record maintenance, adherence to safety protocols like the WHO Safe Childbirth Checklist, competent skilled birth attendants, and well-organized labor rooms.
Community health nurses play a pivotal role in ensuring safe childbirth experiences, particularly in settings where access to specialized care may be limited. By mastering these four essential components—records and reports maintenance, implementation of the safe childbirth checklist, application of SBA competencies, and proper labor room organization—nurses contribute significantly to reducing maternal and newborn mortality and morbidity.
Continuous professional development, adherence to evidence-based practices, and adaptation of global best practices to local contexts are key strategies for improving maternal care. As healthcare systems evolve, community health nurses must remain flexible and committed to incorporating new approaches and technologies that enhance the quality and safety of childbirth services.
Remember: Every woman has the right to a safe childbirth experience, and every newborn deserves a healthy start in life. Community health nurses are at the frontline of making this a reality for families in their communities.
