Renal Disorders in Children
Comprehensive Nursing Notes on Nephrotic Syndrome, Acute Glomerulonephritis, and Renal Failure
Introduction to Pediatric Renal Disorders
Renal disorders in children present unique challenges for healthcare providers. This educational resource provides comprehensive information on three major pediatric renal conditions: nephrotic syndrome, acute glomerulonephritis, and renal failure. These notes integrate pathophysiology, clinical presentation, diagnostic approaches, and evidence-based management strategies essential for nursing care.
Key Points for Nursing Care:
- Children with renal disorders require close monitoring of fluid balance, electrolytes, and vital signs
- Growth and development assessment is crucial due to the impact of renal disease on pediatric growth
- Medication administration requires precise dosing based on renal function and weight
- Family education and emotional support are essential components of comprehensive care
- Nutrition management is critical for preventing complications and supporting recovery
Comparison of Pediatric Renal Disorders
| Feature | Nephrotic Syndrome | Acute Glomerulonephritis | Renal Failure |
|---|---|---|---|
| Definition | Group of symptoms including proteinuria, hypoalbuminemia, edema, and hyperlipidemia | Inflammation of the glomeruli causing hematuria, proteinuria, and azotemia | Temporary or permanent damage to kidneys with loss of normal function |
| Primary Pathophysiology | Altered glomerular permeability leading to massive protein loss | Immune-mediated damage to glomerular basement membrane | Acute: Sudden impairment of kidney function Chronic: Progressive loss of nephrons |
| Common Cause in Children | Minimal change disease (80-90% of cases) | Post-streptococcal infection | Acute: Dehydration, infection, obstruction Chronic: Congenital anomalies |
| Key Clinical Features | Periorbital edema, ascites, foamy urine | Hematuria, hypertension, oliguria | Acute: Oliguria, fluid overload Chronic: Growth failure, anemia |
| Diagnostic Findings | Proteinuria >40 mg/m²/hr Hypoalbuminemia Hyperlipidemia |
Hematuria RBC casts Low C3 complement |
Elevated BUN, creatinine Electrolyte imbalances Metabolic acidosis |
| Treatment Approach | Corticosteroids Sodium restriction Diuretics for edema |
Antibiotics if infection present Supportive care BP management |
Acute: Fluid management, dialysis if needed Chronic: Medication, dialysis, transplant |
| Prognosis | Good; most respond to steroids May have relapses |
Usually resolves without permanent damage | Acute: Often reversible Chronic: Progressive decline |
1. Nephrotic Syndrome in Children
Overview
Nephrotic syndrome is not a disease but a group of symptoms that indicate kidney dysfunction. It’s characterized by massive proteinuria, hypoalbuminemia, edema, and hyperlipidemia. In children, it most commonly affects those between 2-7 years of age, with a higher prevalence in boys.
Clinical Definition
- Proteinuria >40 mg/m²/hr or protein/creatinine ratio >2.0 mg/mg
- Hypoalbuminemia (serum albumin <2.5 g/dL)
- Edema (often periorbital, progressing to generalized)
- Hyperlipidemia (elevated cholesterol and triglycerides)
Epidemiology
- Annual incidence: 2-7 cases per 100,000 children
- Peak incidence: 2-7 years of age
- Male to female ratio: 2:1
- 90% of cases in children are due to minimal change disease
Pathophysiology

The fundamental pathophysiologic event in nephrotic syndrome is increased permeability of the glomerular filtration barrier, which consists of:
Capillary Endothelium
First barrier with fenestrations that normally allow passage of water and small solutes but not larger proteins
Basement Membrane
Middle layer composed of type IV collagen, laminin, and proteoglycans that provides size and charge selectivity
Podocytes
Epithelial cells with foot processes and slit diaphragms that are crucial for preventing protein loss
Sequence of Events:
- Podocyte injury → foot process effacement and loss of slit diaphragm integrity
- Increased glomerular permeability → massive protein loss in urine (primarily albumin)
- Hypoalbuminemia → decreased plasma oncotic pressure
- Fluid shift from intravascular to interstitial space → edema formation
- Compensatory hepatic protein synthesis → increased production of lipoproteins → hyperlipidemia
- Activation of renin-angiotensin-aldosterone system → sodium and water retention → worsening edema
Key Concept: Podocyte Injury
In minimal change disease (most common in children), the podocyte injury is believed to be caused by a circulating factor, possibly released by T cells, that disrupts the actin cytoskeleton of podocytes, leading to foot process effacement.
Etiology and Classification
Primary (Idiopathic) Nephrotic Syndrome
Most common in children, with no identifiable cause. Histologic variants include:
| Type | Frequency in Children | Pathologic Features | Steroid Response |
|---|---|---|---|
| Minimal Change Disease (MCD) | 80-90% | Normal glomeruli on light microscopy; foot process effacement on electron microscopy | Usually responsive (90%) |
| Focal Segmental Glomerulosclerosis (FSGS) | 5-10% | Segmental sclerosis in some glomeruli; foot process effacement | Often resistant |
| Membranous Nephropathy | 1-5% | Thickened GBM with subepithelial immune deposits | Variable response |
| Membranoproliferative GN | Rare in children | Mesangial proliferation with thickening of GBM | Usually resistant |
Secondary Nephrotic Syndrome
Less common in children, caused by:
Infections
- Hepatitis B and C
- HIV
- Malaria
- Syphilis
Systemic Diseases
- Lupus nephritis
- Henoch-Schönlein purpura
- Diabetes mellitus
- Amyloidosis
Drugs/Toxins
- NSAIDs
- Penicillamine
- Gold
- Bismuth
Genetic Causes
- Congenital nephrotic syndrome (Finnish type)
- Alport syndrome
- NPHS1, NPHS2 mutations
Mnemonic: “NEPHROTIC”
To remember key features of nephrotic syndrome:
- N – Numerous proteins lost in urine
- E – Edema (periorbital, then generalized)
- P – Proteinuria (>40 mg/m²/hr)
- H – Hypoalbuminemia (<2.5 g/dL)
- R – Risk of infections and thrombosis
- O – Oncotic pressure decreased
- T – Triglycerides elevated
- I – Immune dysregulation (in MCD)
- C – Cholesterol increased
Clinical Presentation
Cardinal Signs and Symptoms
Edema (Most Common Presenting Feature)
- Periorbital edema (most noticeable in morning)
- Progresses to dependent areas (feet, ankles, genitalia)
- Can become generalized (anasarca) with ascites, pleural effusions
Urinary Findings
- Foamy urine (due to proteinuria)
- Normal or decreased urine output
General Symptoms
- Fatigue and malaise
- Poor appetite
- Irritability
Complications
Infections
- Increased susceptibility (loss of immunoglobulins)
- Peritonitis (particularly pneumococcal)
- Cellulitis, pneumonia, UTIs
Thromboembolism
- Loss of anticoagulant factors in urine
- Increased clotting factors (fibrinogen, factors V, VIII)
- Risk of renal vein thrombosis, pulmonary emboli
Acute Kidney Injury
- Due to hypovolemia
- Renal vein thrombosis
- Interstitial nephritis from medications
Clinical Pearls:
- Morning periorbital edema that improves throughout the day is a classic initial presentation
- Weight gain is often the first objective sign parents notice
- Hypertension is uncommon in pure minimal change disease – its presence suggests alternative diagnosis
- Gross hematuria is rare – if present, consider other diagnoses
Diagnostic Evaluation
Initial Laboratory Evaluation
Urinalysis
- Proteinuria (3+ to 4+ on dipstick)
- Hyaline casts
- Absent or minimal hematuria
Urine Studies
- 24-hour urine protein (>40 mg/m²/hr or >1g/m²/day)
- Spot urine protein/creatinine ratio (>2.0 mg/mg)
- Urine protein electrophoresis (predominant albumin)
Blood Tests
- Serum albumin (<2.5 g/dL)
- Total protein (decreased)
- Cholesterol and triglycerides (elevated)
- BUN and creatinine (usually normal)
- Electrolytes (may show hyponatremia)
Additional Investigations
Complement Studies
- C3, C4 (typically normal in MCD)
- Low complement suggests MPGN or lupus nephritis
Serologic Studies (for secondary causes)
- ANA, anti-dsDNA (for lupus)
- ANCA (for vasculitis)
- Hepatitis B, C, HIV serology
Imaging
- Renal ultrasound (normal size kidneys in MCD)
- Chest X-ray (if respiratory symptoms present)
Renal Biopsy
Not routinely indicated initially in children with typical presentation. Indications include:
- Age <1 year or >12 years
- Steroid resistance or dependence
- Atypical features (gross hematuria, hypertension)
- Low complement levels
- Persistent renal insufficiency
Diagnostic Criteria for Nephrotic Syndrome:
- Proteinuria >40 mg/m²/hr or spot urine protein/creatinine ratio >2.0 mg/mg
- Hypoalbuminemia (serum albumin <2.5 g/dL)
- Edema
- Hyperlipidemia (not required for diagnosis but typically present)
Management Approach
Pharmacological Management
Corticosteroids (First-line)
- Initial therapy: Prednisone 60 mg/m²/day or 2 mg/kg/day (max 60 mg) for 4-6 weeks
- Followed by: 40 mg/m²/day or 1.5 mg/kg/day on alternate days for 4-6 weeks, then taper
- 80-90% of children with MCD respond within 4 weeks
For Frequent Relapses or Steroid Dependence
- Cyclophosphamide: 2-3 mg/kg/day for 8-12 weeks
- Levamisole: 2.5 mg/kg on alternate days
- Mycophenolate mofetil: 600-1200 mg/m²/day in 2 divided doses
- Calcineurin inhibitors:
- Cyclosporine: 3-5 mg/kg/day in 2 divided doses
- Tacrolimus: 0.05-0.1 mg/kg/day in 2 divided doses
- Rituximab: 375 mg/m² weekly for 1-4 doses (for difficult cases)
Symptomatic Management
- Diuretics: For severe edema (furosemide 1-2 mg/kg/dose)
- Albumin infusion: 25% albumin 0.5-1 g/kg followed by diuretic (for severe edema with hypovolemia)
- ACE inhibitors: To reduce proteinuria in steroid-resistant cases
- Statins: For persistent hyperlipidemia (rarely needed in children)
Supportive Management
Nutritional Management
- Normal protein diet (1-2 g/kg/day)
- Sodium restriction (1-2 g/day) during edematous phase
- No routine fluid restriction unless hyponatremia present
- Low cholesterol diet if hyperlipidemia persists
Infection Prevention
- Pneumococcal vaccination
- Prompt treatment of infections
- Avoid unnecessary exposure to sick contacts
Thrombosis Prevention
- Early mobilization when possible
- Consider prophylactic anticoagulation in high-risk cases
Activity and Lifestyle
- Return to school once edema resolves
- No restriction of physical activity once in remission
- Regular monitoring of urine protein at home
Response Definitions:
- Remission: Urine protein negative or trace for 3 consecutive days
- Relapse: Urine protein 3+ or 4+ for 3 consecutive days after having been in remission
- Frequent relapses: ≥2 relapses within 6 months of initial response or ≥4 relapses in any 12-month period
- Steroid dependence: Two consecutive relapses during steroid therapy or within 14 days of discontinuation
- Steroid resistance: Failure to achieve remission after 8 weeks of daily prednisone
Nursing Considerations
Assessment
Initial Assessment
- Comprehensive measurement of edema (location, pitting)
- Accurate weight and vital signs (baseline)
- Abdominal girth measurement (if ascites present)
- Fluid balance assessment
- Respiratory status (for pleural effusions)
Ongoing Monitoring
- Daily weight (same time, clothing, scale)
- Strict intake and output
- BP monitoring (at least twice daily)
- Daily urine dipstick for protein
- Signs of steroid side effects
- Signs of infection or thrombosis
Interventions
Medication Administration
- Administer steroids with food to minimize GI effects
- Give diuretics in morning to avoid nighttime diuresis
- Monitor for medication side effects
- Administer albumin infusions slowly (over 2-4 hours)
Edema Management
- Elevate edematous extremities
- Reposition frequently to prevent pressure areas
- Gentle skin care for edematous areas
- Monitor skin integrity, especially in skin folds
Family Education
- Home urine dipstick monitoring
- Recognition of relapse signs
- Medication administration and side effects
- Dietary sodium restriction
- When to seek medical attention
- Infection prevention strategies
Nursing Care Mind Map for Nephrotic Syndrome
NEPHROTIC SYNDROME NURSING CARE
├── ASSESSMENT
│ ├── Daily Weight
│ ├── Edema Evaluation
│ ├── Vital Signs
│ ├── Intake & Output
│ └── Urine Protein Monitoring
│
├── MANAGEMENT
│ ├── Medication Administration
│ │ ├── Corticosteroids
│ │ ├── Diuretics
│ │ └── Immunosuppressants
│ │
│ ├── Fluid & Electrolyte Balance
│ │ ├── Sodium Restriction
│ │ └── IV Albumin (if ordered)
│ │
│ └── Skin Care for Edematous Areas
│
├── MONITORING
│ ├── Complications
│ │ ├── Infection
│ │ ├── Thrombosis
│ │ └── Steroid Side Effects
│ │
│ └── Laboratory Values
│ ├── Urine Protein
│ ├── Serum Albumin
│ └── Electrolytes
│
└── EDUCATION
├── Disease Process
├── Medication Information
├── Home Monitoring
├── Dietary Guidance
├── Activity Recommendations
└── When to Seek Medical Care
2. Acute Glomerulonephritis
Overview
Acute glomerulonephritis (AGN) is inflammation of the glomeruli resulting in hematuria, proteinuria, decreased urine output, and often hypertension and edema. In children, it is most commonly post-infectious, particularly following group A beta-hemolytic streptococcal infection (post-streptococcal glomerulonephritis or PSGN).
Clinical Definition
- Abrupt onset of hematuria (microscopic or gross)
- Variable proteinuria (usually subnephrotic)
- Decreased glomerular filtration rate
- Edema and hypertension (nephritic syndrome)
Epidemiology
- Most common between ages 5-12 years
- Male:female ratio of 2:1
- More common in developing countries
- May occur sporadically or in epidemics
- Incidence decreasing in developed countries
Pathophysiology

Acute glomerulonephritis is primarily an immune-complex mediated disease where immune complexes deposit in the glomeruli, activating inflammatory pathways.
Pathogenesis of Post-Streptococcal Glomerulonephritis:
- Streptococcal infection (typically pharyngitis or impetigo from “nephritogenic” strains)
- Latent period (1-2 weeks after pharyngitis, 3-6 weeks after impetigo)
- Formation of immune complexes (either in circulation or in situ within glomeruli)
- Glomerular immune complex deposition (primarily in subepithelial location)
- Complement activation (primarily via alternative pathway)
- Inflammatory response with neutrophil and monocyte infiltration
- Endothelial injury causing decreased glomerular filtration rate
- Proliferation of mesangial and endothelial cells (giving “lumpy-bumpy” appearance)
Glomerular Changes
Enlarged, hypercellular glomeruli due to proliferation of endothelial and mesangial cells and infiltration of neutrophils
Immune Deposits
Granular deposits of IgG and C3 along the capillary walls and mesangium appearing as “lumpy-bumpy” pattern on immunofluorescence
Electron Microscopy
Subepithelial electron-dense deposits (“humps”) with effacement of podocyte foot processes
Functional Consequences:
- Decreased glomerular filtration rate due to:
- Inflammatory narrowing of capillary lumina
- Structural damage to glomerular basement membrane
- Mesangial and endothelial cell proliferation
- Hematuria from damage to glomerular filtration barrier
- Proteinuria from altered capillary permeability
- Sodium and water retention leading to edema and hypertension
- Azotemia from reduced GFR and impaired waste elimination
Key Concept: Streptococcal Antigens in PSGN
Several streptococcal antigens have been implicated in PSGN pathogenesis, including:
- Nephritis-associated plasmin receptor (NAPlr)
- Streptococcal pyrogenic exotoxin B (SpeB)
- Streptococcal M proteins (particularly M types 1, 4, 12, 49, 55, 57, 60)
These antigens may directly deposit in the glomeruli or form immune complexes that trigger inflammation.
Etiology and Classification
Post-Infectious Causes
The most common causes of AGN in children:
| Pathogen | Specific Agents | Clinical Features |
|---|---|---|
| Bacterial |
|
Latent period between infection and nephritis; hypocomplementemia |
| Viral |
|
Often concurrent infection and nephritis; variable complement levels |
| Parasitic |
|
More common in endemic regions; may have other system involvement |
Non-Infectious Causes
Primary Glomerular Diseases
- IgA nephropathy (Berger’s disease)
- Membranoproliferative glomerulonephritis
- Anti-glomerular basement membrane disease
- C3 glomerulopathy
Systemic Diseases
- Henoch-Schönlein purpura
- Systemic lupus erythematosus
- ANCA-associated vasculitis
- Goodpasture syndrome
Classification by Histopathology
Diffuse Proliferative GN
Affects most/all glomeruli; characterized by endocapillary hypercellularity. Most common pattern in PSGN.
Focal Proliferative GN
Affects some but not all glomeruli; common in IgA nephropathy and Henoch-Schönlein purpura.
Crescentic GN
Characterized by crescent formation; indicates severe injury; associated with rapidly progressive GN.
Mnemonic: “NEPHRITIS”
To remember causes of acute glomerulonephritis in children:
- N – Nephritogenic strep (Group A β-hemolytic streptococcus)
- E – Endocarditis (infective)
- P – Post-infectious causes (viral, bacterial)
- H – Henoch-Schönlein purpura
- R – Renal diseases (IgA nephropathy)
- I – Immune complex diseases (lupus nephritis)
- T – Toxin-mediated (heavy metals)
- I – Infectious diseases (HBV, HCV, HIV)
- S – Systemic diseases (vasculitis)
Clinical Presentation
Cardinal Signs and Symptoms
Urinary Findings
- Hematuria (microscopic or gross “tea-colored” or “cola-colored” urine)
- Proteinuria (usually non-nephrotic range)
- RBC casts in urine sediment
- Oliguria (reduced urine output)
Fluid Retention
- Periorbital edema (typically most prominent in morning)
- Peripheral edema (less prominent than in nephrotic syndrome)
- Facial puffiness
- Weight gain
Hypertension
- Present in 60-80% of cases
- Usually mild to moderate
- Due to fluid retention and activation of renin-angiotensin system
Associated Symptoms
General Symptoms
- Fatigue and malaise
- Low-grade fever
- Flank or abdominal pain
- Anorexia
In Severe Cases
- Acute kidney injury (elevated BUN and creatinine)
- Pulmonary edema (dyspnea, crackles)
- Hypertensive encephalopathy (headache, altered mental status, seizures)
- Heart failure
Post-Streptococcal Specific
- History of recent pharyngitis or impetigo
- Latent period between infection and nephritis
- May have persistent sore throat or skin lesions
Clinical Course of PSGN:
- Onset typically 1-2 weeks after pharyngitis, 3-6 weeks after skin infection
- Most children recover completely within 6-8 weeks
- Urinary abnormalities may persist for several months
- Microscopic hematuria may take up to 1-2 years to resolve
- Less than 1% of children develop chronic kidney disease
- Recurrence is rare in post-streptococcal glomerulonephritis
Diagnostic Evaluation
Initial Laboratory Evaluation
Urinalysis
- Hematuria (RBCs >5/HPF)
- RBC casts (pathognomonic of glomerular disease)
- Proteinuria (1+ to 2+)
- Dysmorphic RBCs (indicating glomerular origin)
Blood Tests
- BUN and creatinine (may be elevated)
- Electrolytes (may show hyponatremia)
- Complete blood count (may show anemia)
- Albumin (usually normal or slightly decreased)
Complement Studies
- C3 levels (decreased in PSGN)
- C4 levels (usually normal in PSGN)
- CH50 (total complement, usually decreased)
Specific Tests for PSGN
Streptococcal Infection Markers
- Anti-streptolysin O (ASO) titer (elevated in pharyngeal infections)
- Anti-DNase B (elevated in both skin and pharyngeal infections)
- Streptozyme test (combination of streptococcal antibodies)
- Throat or skin culture (may be negative by time of nephritis)
Additional Investigations
- Antinuclear antibodies (if suspecting lupus)
- ANCA (if suspecting vasculitis)
- Anti-GBM antibodies (if suspecting Goodpasture syndrome)
- Viral studies (for hepatitis B, C, HIV if suspected)
Imaging
- Renal ultrasound (normal or enlarged kidneys with increased echogenicity)
- Chest X-ray (if pulmonary symptoms present)
Renal Biopsy
Not routinely indicated in typical post-streptococcal glomerulonephritis. Consider if:
- Atypical presentation or course
- Persistent low complement beyond 8 weeks
- Rapidly progressive renal failure
- Nephrotic range proteinuria
- No evidence of streptococcal infection
Diagnostic Strategy for Acute Glomerulonephritis:
- Establish the presence of glomerulonephritis (hematuria, proteinuria, RBC casts)
- Assess renal function (BUN, creatinine, GFR)
- Evaluate complement levels (low C3 suggests post-infectious or lupus)
- Look for evidence of streptococcal infection (ASO, anti-DNase B)
- Consider other etiologies if PSGN is unlikely based on history, exam, and labs
- Reserve renal biopsy for atypical presentations or failure to improve
Management Approach
General Management Principles
Treatment of Underlying Cause
- For PSGN: Antibiotic therapy if active streptococcal infection is present
- Penicillin V: 250-500 mg PO QID for 10 days
- Amoxicillin: 50 mg/kg/day in divided doses
- For penicillin allergy: Erythromycin or azithromycin
- Note: Antibiotics don’t alter the course of nephritis once established but prevent spread of infection
Supportive Care
- Fluid management:
- Monitor fluid balance closely
- Restrict fluids if edema or hypertension present
- Replacement based on urine output and insensible losses
- Diet:
- Sodium restriction (1-2 g/day)
- Potassium restriction if hyperkalemic
- Moderate protein intake
Management of Complications
Hypertension Management
- Mild to moderate hypertension:
- Sodium and fluid restriction
- Calcium channel blockers (e.g., amlodipine 0.1-0.6 mg/kg/day)
- Beta-blockers (e.g., metoprolol 1-2 mg/kg/day)
- Severe hypertension:
- IV labetalol (0.2-1 mg/kg/dose)
- Nicardipine infusion (1-3 mcg/kg/min)
- Sodium nitroprusside (0.5-10 mcg/kg/min) for hypertensive emergency
Volume Overload/Edema
- Loop diuretics (furosemide 1-2 mg/kg/dose)
- Consider dialysis if severe/refractory
Acute Kidney Injury
- Maintain fluid and electrolyte balance
- Avoid nephrotoxic drugs
- Dialysis indications:
- Severe hyperkalemia (K+ >6.5 mEq/L)
- Severe acidosis (pH <7.2)
- Uremic symptoms
- Refractory fluid overload
Monitoring and Follow-up:
- Daily weight and vital signs during acute phase
- Regular monitoring of urinalysis, BUN, creatinine, electrolytes
- Follow complement levels until normalization
- Monitor blood pressure until normalized
- Follow-up visits:
- Weekly initially
- Then monthly until urine findings resolve
- Long-term follow-up for 1-2 years with periodic urinalysis
Nursing Considerations
Assessment
Initial Nursing Assessment
- Comprehensive vital signs with accurate BP measurement
- Careful assessment of volume status and edema
- Urine appearance, output, and frequency
- Neurological assessment (for hypertensive encephalopathy)
- Respiratory assessment (for pulmonary edema)
Ongoing Monitoring
- Strict intake and output monitoring
- Daily weight measurements
- Monitor BP every 4-6 hours or more frequently if elevated
- Check urine for color, clarity, and presence of blood
- Monitor for signs of worsening kidney function
Interventions
Fluid and Electrolyte Management
- Implement prescribed fluid restrictions
- Administer diuretics as ordered, monitor response
- Educate on low-sodium diet adherence
- Monitor for signs of electrolyte disturbances
Blood Pressure Management
- Administer antihypertensive medications as prescribed
- Ensure proper BP cuff size for accurate measurements
- Monitor for signs of hypertensive emergency
- Position patient with head elevated if hypertensive
Education and Support
- Explain disease process and expected course
- Teach importance of medication adherence
- Instruct on home BP monitoring techniques
- Provide guidance on dietary sodium restriction
- Educate on when to seek medical attention
Nursing Care Mind Map for AGN
ACUTE GLOMERULONEPHRITIS NURSING CARE
├── ASSESSMENT
│ ├── Vital Signs (Especially BP)
│ ├── Fluid Status
│ │ ├── Edema
│ │ ├── Daily Weight
│ │ └── Intake & Output
│ │
│ ├── Urine Characteristics
│ │ ├── Hematuria
│ │ └── Proteinuria
│ │
│ └── Symptoms of Complications
│ ├── Encephalopathy
│ └── Pulmonary Edema
│
├── INTERVENTIONS
│ ├── Fluid Management
│ │ ├── Fluid Restriction
│ │ └── Diuretic Administration
│ │
│ ├── Hypertension Management
│ │ ├── Medication Administration
│ │ └── Position & Activity Adjustments
│ │
│ ├── Infection Prevention
│ │ ├── Antibiotic Administration
│ │ └── Hand Hygiene
│ │
│ └── Rest & Comfort Measures
│
└── EDUCATION
├── Disease Process
├── Medication Information
├── Dietary Restrictions
├── Activity Guidelines
└── Follow-up Schedule
3. Renal Failure in Children
Overview
Renal failure in children refers to the inability of kidneys to adequately filter waste products, concentrate urine, and maintain fluid and electrolyte balance. It is classified into acute kidney injury (AKI) and chronic kidney disease (CKD), each with distinct causes, presentations, and management approaches.
Acute Kidney Injury (AKI)
- Sudden, potentially reversible decline in kidney function
- Develops over hours to days
- Results in accumulation of nitrogenous wastes and fluid imbalance
- May be reversible with prompt intervention
Chronic Kidney Disease (CKD)
- Progressive, irreversible loss of kidney function
- Develops over months to years
- Results in permanent kidney damage
- Eventually leads to end-stage renal disease (ESRD) requiring dialysis or transplantation
Pathophysiology
Acute Kidney Injury Pathophysiology
Mechanisms of Injury:
- Prerenal: Decreased renal perfusion
- Hypovolemia (dehydration, hemorrhage)
- Decreased cardiac output
- Renal vasoconstriction
- Intrinsic renal: Direct kidney damage
- Acute tubular necrosis (ischemic or toxic)
- Acute interstitial nephritis
- Glomerulonephritis
- Vascular disease
- Postrenal: Urinary tract obstruction
- Congenital anomalies
- Stones
- Tumors
- Posterior urethral valves
Tubular Injury Process:
- Reduced renal blood flow → decreased oxygen delivery
- Tubular epithelial cell injury and death
- Tubular obstruction from cellular debris
- Backleak of filtrate through damaged tubules
- Vasoconstriction from tubuloglomerular feedback
- Reduced glomerular filtration rate (GFR)
Chronic Kidney Disease Pathophysiology
Progressive Nephron Loss:
- Initial kidney injury (congenital or acquired)
- Loss of functioning nephrons
- Hyperfiltration of remaining nephrons
- Compensatory hypertrophy
- Secondary glomerulosclerosis
- Further nephron loss in self-perpetuating cycle
- Eventually, critical mass of nephrons lost
Systemic Complications:
- Fluid and electrolyte imbalances: Inability to regulate sodium, potassium, acid-base balance
- Metabolic bone disease: Abnormal vitamin D metabolism, phosphate retention, secondary hyperparathyroidism
- Anemia: Reduced erythropoietin production
- Growth retardation: Metabolic acidosis, malnutrition, resistance to growth hormone
- Cardiovascular changes: Hypertension, left ventricular hypertrophy, vascular calcification
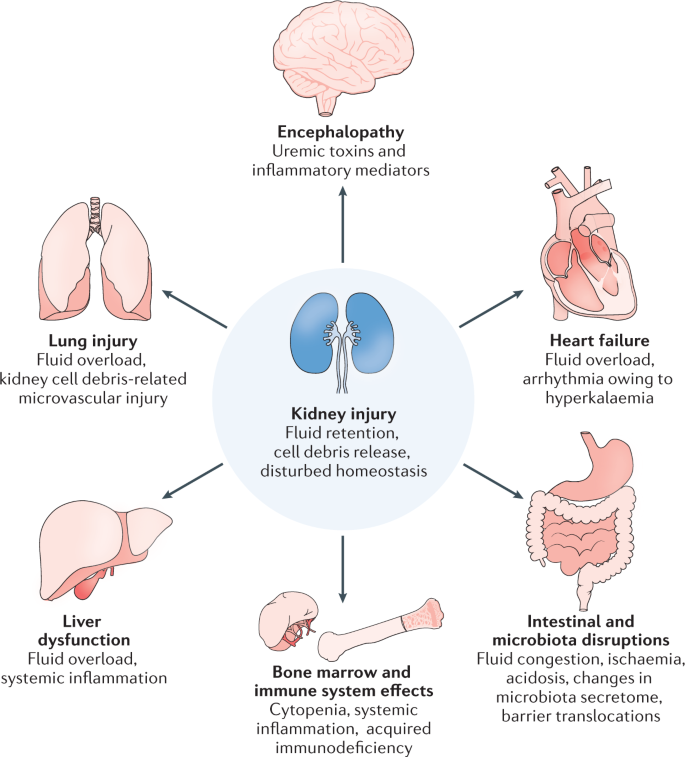
Uremic Toxins
Accumulation of nitrogenous waste products (urea, creatinine) and other uremic toxins leads to systemic manifestations and end-organ damage
Hormonal Dysregulation
Disruption of renin-angiotensin-aldosterone system, erythropoietin, vitamin D activation, and FGF-23/klotho axis
Growth Impact
Unique to pediatric patients: decreased linear growth, delayed puberty, and impaired cognitive development due to uremia and metabolic disturbances
Key Concept: Kidney Reserve
Children, like adults, have substantial renal reserve. Serum creatinine does not typically rise until 50% of nephrons are damaged. This results in “silent” progression of CKD until significant damage has occurred.
Etiology and Classification
Acute Kidney Injury Causes
| Category | Common Causes | Pathophysiology |
|---|---|---|
| Prerenal (55%) |
|
Decreased renal perfusion leading to reduced GFR; kidney function remains intact |
| Intrinsic Renal (40%) |
|
Direct damage to kidney parenchyma affecting glomeruli, tubules, interstitium, or blood vessels |
| Postrenal (5%) |
|
Obstruction to urine flow leading to increased backward pressure and decreased GFR |
Chronic Kidney Disease Causes
Causes vary by age group:
| Age Group | Common Causes |
|---|---|
| Infants (0-1 years) |
|
| Young Children (1-5 years) |
|
| Older Children (6-12 years) |
|
| Adolescents (13-18 years) |
|
Classification of Acute Kidney Injury (KDIGO)
| Stage | Serum Creatinine | Urine Output |
|---|---|---|
| 1 | 1.5-1.9 times baseline OR ≥0.3 mg/dL increase | <0.5 mL/kg/hr for 6-12 hrs |
| 2 | 2.0-2.9 times baseline | <0.5 mL/kg/hr for ≥12 hrs |
| 3 | 3.0 times baseline OR Increase to ≥4.0 mg/dL OR Initiation of renal replacement OR GFR <35 mL/min/1.73m² | <0.3 mL/kg/hr for ≥24 hrs OR Anuria for ≥12 hrs |
Classification of Chronic Kidney Disease
| Stage | GFR (mL/min/1.73m²) | Description |
|---|---|---|
| 1 | ≥90 | Normal or high GFR with kidney damage* |
| 2 | 60-89 | Mildly decreased GFR with kidney damage* |
| 3a | 45-59 | Mildly to moderately decreased GFR |
| 3b | 30-44 | Moderately to severely decreased GFR |
| 4 | 15-29 | Severely decreased GFR |
| 5 | <15 | Kidney failure (ESRD) |
*Kidney damage defined as pathological abnormalities or markers of damage, including abnormalities in blood or urine tests or imaging studies
Mnemonic: “RENAL FAILURE”
To remember common causes of renal failure in children:
- R – Renal dysplasia/hypoplasia
- E – Endocrine disorders (diabetes)
- N – Nephrotic syndrome
- A – Acute tubular necrosis
- L – Lupus nephritis
- F – Focal segmental glomerulosclerosis
- A – Alport syndrome
- I – Interstitial nephritis
- L – Lower urinary tract obstruction
- U – Urologic abnormalities (CAKUT)
- R – Reflux nephropathy
- E – Ehrlichia (Hemolytic uremic syndrome)
Clinical Presentation
Acute Kidney Injury Presentation
Urinary Findings
- Oliguria (<0.5 mL/kg/hr) or anuria
- May have polyuria in some cases
- Hematuria (variable)
- Proteinuria (variable)
Volume Status
- Prerenal: Signs of dehydration (decreased skin turgor, dry mucous membranes)
- Intrinsic: Variable, may have edema
- Postrenal: May have bladder distention, flank tenderness
Systemic Features
- Hypertension
- Fluid overload (edema, pulmonary crackles)
- Lethargy, confusion (from uremia or electrolyte disturbances)
- Anorexia, nausea, vomiting
- Features of underlying cause (rash, joint pain, etc.)
Chronic Kidney Disease Presentation
Early CKD (Often Asymptomatic)
- Growth retardation (often first sign in children)
- Mild hypertension
- Polyuria/nocturia (concentrating defect)
- Mild anemia
- Subtle neurocognitive issues
Advanced CKD
- Poor growth and delayed puberty
- Moderate to severe hypertension
- Bone deformities and pain
- Pallor (anemia)
- Uremic symptoms (fatigue, poor appetite, nausea)
- Pruritus
- Neurological symptoms (reduced concentration, poor school performance)
End-Stage Renal Disease
- Severe growth failure
- Uremic frost
- Pericarditis
- Encephalopathy
- Peripheral neuropathy
- Bleeding diathesis
- Severe anemia
Special Considerations in Children:
- Growth parameters: Linear growth impairment is often the earliest and most sensitive marker of CKD in children
- Developmental milestones: May be delayed with significant renal dysfunction
- Pubertal development: Often delayed in CKD stages 3-5
- School performance: May decline due to anemia, subtle uremia, and frequent medical appointments
- Psychosocial impact: Self-image concerns, depression, anxiety more common with visible signs of kidney disease
Diagnostic Evaluation
Laboratory Studies
Blood Tests
- BUN and creatinine (elevated)
- Electrolytes
- Potassium (often elevated)
- Sodium (variable)
- Calcium (decreased in CKD)
- Phosphorus (elevated in CKD)
- Acid-base status (usually metabolic acidosis)
- Complete blood count (anemia common in CKD)
- Albumin (may be decreased)
Urine Studies
- Urinalysis (for blood, protein, specific gravity)
- Urine electrolytes (helps distinguish prerenal from intrinsic causes)
- Fractional excretion of sodium (FENa)
- Urine sodium
- Protein/creatinine ratio
- Urine output measurement
Additional Studies for CKD
- Parathyroid hormone (elevated in CKD)
- 25-OH and 1,25-OH vitamin D levels
- Alkaline phosphatase (bone metabolism)
- Lipid profile
- Iron studies
- Glomerular filtration rate (GFR) estimation
- Schwartz formula for children
- Nuclear medicine studies (gold standard)
Imaging and Additional Tests
Imaging Studies
- Renal ultrasound
- Kidney size and echogenicity
- Evidence of obstruction
- Congenital anomalies
- Voiding cystourethrogram (for suspected reflux or obstruction)
- CT scan (rarely needed)
- MRI (for detailed anatomy or vascular issues)
- Nuclear scans (for function assessment)
Specialized Testing
- Kidney biopsy (for definitive diagnosis of intrinsic disease)
- Genetic testing (for suspected hereditary conditions)
- Complement studies (for glomerulonephritis)
- Autoantibody studies (for autoimmune causes)
Monitoring in CKD
- Growth parameters (height, weight, BMI)
- Blood pressure monitoring
- Bone age X-rays
- Renal osteodystrophy evaluation
- Developmental assessment
- Cardiovascular risk assessment
Diagnostic Approach:
- Confirm the presence of kidney dysfunction (elevated creatinine, abnormal GFR)
- Determine acuity (acute vs. chronic) – history, previous labs, imaging, anemia, growth
- In AKI, identify the mechanism (prerenal, intrinsic, postrenal)
- In CKD, stage the disease based on GFR and identify underlying cause
- Assess for complications of kidney failure
- Evaluate growth and development in pediatric patients
Management Approach
Acute Kidney Injury Management
Initial Stabilization
- Treat life-threatening complications
- Hyperkalemia
- Pulmonary edema
- Severe acidosis
- Uremic encephalopathy
- Correct underlying cause
- Fluid resuscitation (for prerenal causes)
- Relief of obstruction (for postrenal causes)
- Discontinue nephrotoxic drugs
- Treat infections
Fluid and Electrolyte Management
- Careful fluid management
- Replace ongoing losses
- Restrict fluids if oliguric
- Adjust maintenance based on output
- Hyperkalemia management
- Calcium gluconate (for cardiac stabilization)
- Insulin and glucose
- Sodium bicarbonate
- Potassium-binding resins
- Acidosis correction (sodium bicarbonate for severe acidosis)
Renal Replacement Therapy (RRT) Indications
- Refractory hyperkalemia
- Severe acidosis unresponsive to medical therapy
- Volume overload causing respiratory compromise
- Uremic symptoms (encephalopathy, pericarditis)
- Certain toxin ingestions
RRT Modalities
- Peritoneal dialysis (often first choice in small children)
- Continuous renal replacement therapy (CRRT)
- Intermittent hemodialysis
Chronic Kidney Disease Management
Slow Progression
- Blood pressure control
- ACE inhibitors or ARBs preferred
- Target BP <90th percentile for age, height, and sex
- Proteinuria reduction
- Glycemic control (if diabetic)
- Avoid nephrotoxins
Metabolic Complications Management
- Anemia
- Erythropoiesis-stimulating agents
- Iron supplementation
- Mineral bone disorder
- Phosphate binders
