Nursing Notes
Reproduction in Biology
Comprehensive Guide to Plant and Human Reproductive Health
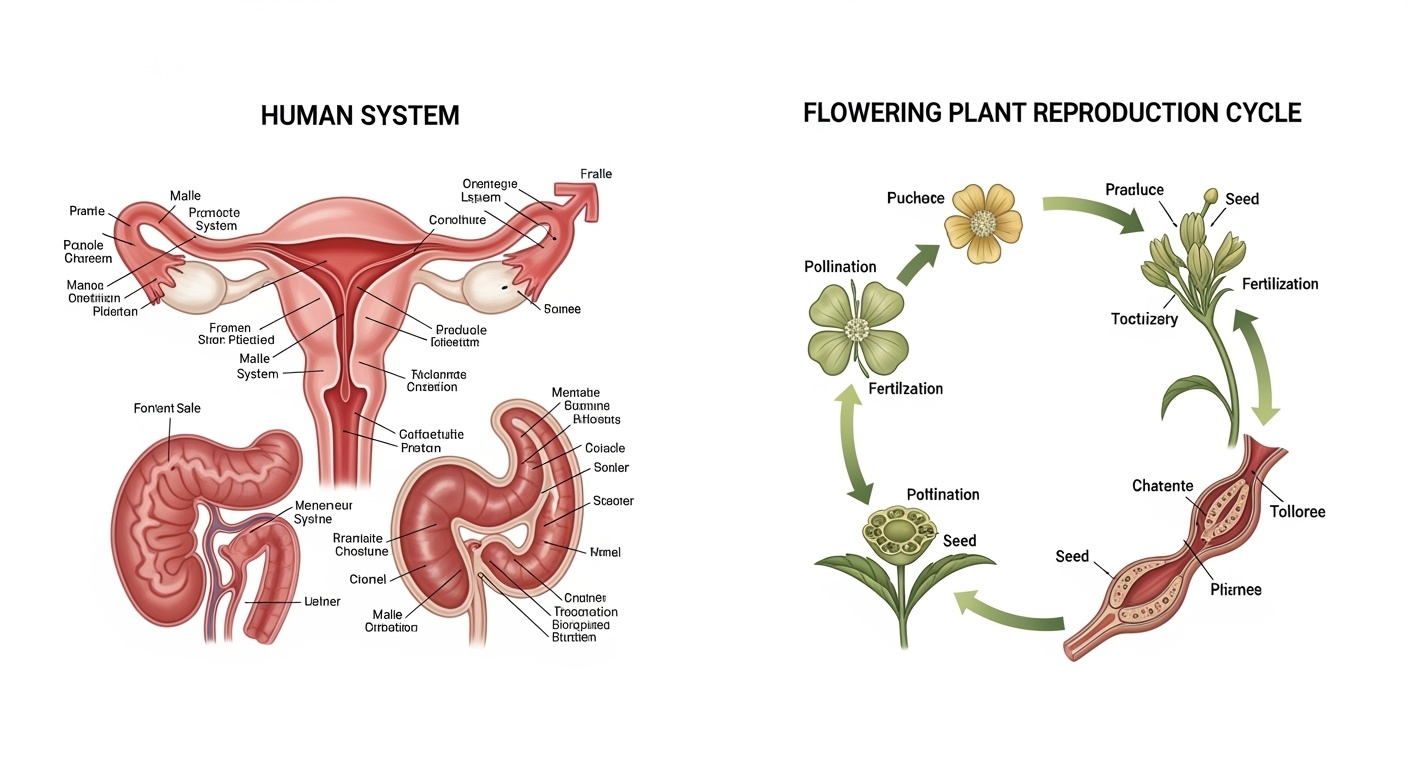
Table of Contents
Sexual Reproduction in Flowering Plants
Sexual reproduction in flowering plants represents a sophisticated biological process that ensures genetic diversity and species survival. Understanding plant reproduction provides nursing students with foundational knowledge applicable to human reproductive health concepts, particularly regarding gamete formation, fertilization processes, and hormonal regulation mechanisms.
Key Learning Objectives
- Understand the structural components of flowers and their reproductive functions
- Analyze pollination mechanisms and their efficiency in reproductive health
- Compare plant and human fertilization processes
- Apply knowledge of reproductive cycles to clinical nursing practice
Flower Structure and Function
Flowers serve as the reproductive organs of angiosperms, containing both male and female reproductive structures. The intricate design of floral components parallels the complexity found in human reproductive anatomy, making this knowledge relevant for understanding reproductive health principles.
| Floral Part | Function | Clinical Parallel |
|---|---|---|
| Stamen (Male) | Produces pollen grains containing male gametes | Similar to testes producing sperm |
| Pistil (Female) | Contains ovules with female gametes | Comparable to ovaries containing eggs |
| Petals | Attract pollinators through color and scent | Similar to secondary sexual characteristics |
| Sepals | Protect developing flower bud | Like protective tissues in reproductive organs |
Nursing Application: Understanding Reproductive Anatomy
When teaching patients about reproductive health, nurses can use the flower analogy to explain how reproductive organs have specialized functions. Just as flowers have protective outer layers (sepals) and inner reproductive structures, human reproductive systems have protective mechanisms and specialized organs for gamete production and fertilization.
Pollination Mechanisms
Pollination represents the transfer of pollen from male to female reproductive structures, a process requiring precise timing and environmental conditions. This mechanism demonstrates principles of reproductive health that nurses encounter when counseling patients about fertility and conception timing.
Self-Pollination
- Occurs within the same flower
- Ensures reproduction in isolated conditions
- Reduces genetic diversity
- Parallel: Reproductive health challenges in closed populations
Cross-Pollination
- Transfer between different flowers
- Promotes genetic diversity
- Requires external agents (wind, insects)
- Parallel: Genetic diversity in human populations
Nursing Application: Fertility Counseling
Understanding pollination timing helps nurses explain fertility windows to patients. Just as successful pollination requires optimal environmental conditions and timing, human conception depends on precise timing of ovulation, sperm viability, and favorable reproductive tract conditions. This knowledge supports evidence-based fertility counseling and reproductive health education.
Fertilization Process in Plants
Plant fertilization involves complex cellular mechanisms that share fundamental similarities with human reproductive processes. The double fertilization unique to flowering plants demonstrates sophisticated reproductive strategies relevant to understanding reproductive health complexity.
| Stage | Plant Process | Human Parallel |
|---|---|---|
| Pollen Tube Growth | Pollen tube extends through style to ovule | Sperm migration through reproductive tract |
| Gamete Fusion | Male and female nuclei combine | Sperm-egg fertilization |
| Embryo Development | Zygote develops into plant embryo | Embryonic development in humans |
| Seed Formation | Protective seed coat develops | Placental and amniotic protection |
Male Reproductive System
The male reproductive system produces, maintains, and delivers sperm cells while secreting hormones essential for reproductive health. Understanding male reproductive anatomy and physiology enables nurses to provide comprehensive reproductive health care, including assessment, education, and intervention strategies.
Primary Structures
Testes
Primary reproductive organs producing sperm and testosterone. Located in the scrotum for optimal temperature regulation essential for spermatogenesis.
Epididymis
Coiled tube where sperm mature and gain motility. Critical for sperm development and storage, affecting male fertility.
Vas Deferens
Muscular tube transporting sperm from epididymis to urethra during ejaculation.
Accessory Glands
Prostate Gland
Produces alkaline fluid neutralizing vaginal acidity, enhancing sperm survival and motility.
Seminal Vesicles
Secrete fructose-rich fluid providing energy for sperm motility and comprising majority of semen volume.
Bulbourethral Glands
Produce pre-ejaculatory fluid that neutralizes urethral acidity and lubricates urethra.
Nursing Assessment: Male Reproductive Health
Nurses conducting male reproductive health assessments should evaluate:
- Testicular size, consistency, and presence of masses through palpation
- Signs of infections, including urethral discharge or penile lesions
- Sexual health history including fertility concerns and contraceptive use
- Prostate health screening recommendations based on age and risk factors
- Hormonal symptoms such as decreased libido or erectile dysfunction
Female Reproductive System
The female reproductive system encompasses complex structures and processes supporting ovulation, fertilization, pregnancy, and childbirth. Comprehensive understanding of female reproductive anatomy and physiology is essential for nurses providing reproductive health care, gynecological services, and maternal health support.
| Structure | Function | Nursing Considerations |
|---|---|---|
| Ovaries | Produce eggs and hormones (estrogen, progesterone) | Monitor for cysts, assess hormonal symptoms |
| Fallopian Tubes | Transport eggs, site of fertilization | Screen for tubal patency, ectopic pregnancy risk |
| Uterus | Support fetal development, menstruation | Assess menstrual patterns, pregnancy readiness |
| Cervix | Produces mucus, pregnancy barrier | Perform cervical cancer screening, assess discharge |
| Vagina | Birth canal, receives penis during intercourse | Evaluate pH balance, assess for infections |
Hormonal Regulation in Female Reproductive Health
The female reproductive system operates under complex hormonal control involving:
Primary Hormones
- Follicle Stimulating Hormone (FSH)
- Luteinizing Hormone (LH)
- Estrogen
- Progesterone
Clinical Significance
- Menstrual cycle regulation
- Fertility optimization
- Pregnancy maintenance
- Menopausal transition
The Menstrual Cycle and Reproductive Health
The menstrual cycle represents a complex interplay of hormonal signals preparing the female reproductive system for potential pregnancy. Understanding cycle variations and abnormalities is crucial for nurses providing reproductive health services and identifying potential health concerns.
| Phase | Days | Hormonal Changes | Physical Changes |
|---|---|---|---|
| Menstrual Phase | 1-5 | Low estrogen and progesterone | Endometrial shedding, menstrual flow |
| Follicular Phase | 1-13 | Rising FSH and estrogen | Follicle development, endometrial proliferation |
| Ovulatory Phase | 14 | LH surge, peak estrogen | Ovulation, fertile cervical mucus |
| Luteal Phase | 15-28 | High progesterone, declining estrogen | Endometrial secretion, potential implantation |
Nursing Application: Menstrual Health Assessment
Nurses should assess menstrual patterns to identify reproductive health concerns:
Normal Parameters
- Cycle length: 21-35 days
- Flow duration: 3-7 days
- Volume: 5-40ml total
- Minimal pain or cramping
Red Flags
- Cycles shorter than 21 or longer than 35 days
- Excessive bleeding requiring frequent pad changes
- Severe pain interfering with daily activities
- Absent periods in reproductive-age women
Reproductive Health: A Comprehensive Approach
Reproductive health encompasses physical, mental, and social well-being related to reproductive processes, functions, and systems. This holistic approach recognizes that reproductive health extends beyond the absence of disease to include the capability to reproduce, regulate fertility, and maintain sexual health throughout the lifespan.
Physical Health
- Regular reproductive health screenings
- Sexually transmitted infection prevention
- Preconception health optimization
- Fertility preservation strategies
- Menopause and andropause management
Mental Health
- Body image and self-esteem support
- Sexual identity and orientation acceptance
- Pregnancy and parenting stress management
- Infertility counseling and support
- Postpartum mental health screening
Social Health
- Access to reproductive health services
- Education about reproductive rights
- Partner communication skills
- Cultural competency in care delivery
- Community support systems
World Health Organization Definition
“Reproductive health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity, in all matters relating to the reproductive system and to its functions and processes.”
This definition emphasizes that reproductive health care must address the whole person, considering biological, psychological, and social factors that influence reproductive outcomes and experiences.
| Life Stage | Reproductive Health Focus | Nursing Interventions |
|---|---|---|
| Adolescence | Sexual education, puberty guidance | Age-appropriate education, confidential counseling |
| Reproductive Years | Contraception, fertility, pregnancy care | Comprehensive family planning, prenatal care |
| Perimenopause | Hormonal changes, symptom management | Hormone therapy counseling, lifestyle modifications |
| Post-reproductive | Sexual health maintenance, disease prevention | Continued screening, sexual health support |
Nursing Implications and Clinical Practice
Nurses play a pivotal role in reproductive health care, serving as educators, advocates, and care providers across diverse settings. Understanding reproductive biology and health principles enables nurses to deliver evidence-based care that promotes optimal reproductive outcomes and supports individuals throughout their reproductive lifespan.
Evidence-Based Nursing Practice in Reproductive Health
Nurses integrate knowledge of reproductive biology with clinical expertise to:
Assessment Skills
- Comprehensive reproductive health histories
- Physical examination techniques
- Risk factor identification
- Symptom pattern recognition
Intervention Strategies
- Patient education and counseling
- Preventive care coordination
- Treatment plan implementation
- Ongoing monitoring and evaluation
Patient Education Topics
- Anatomy and physiology of reproductive systems
- Normal menstrual cycle variations
- Contraceptive options and effectiveness
- Sexually transmitted infection prevention
- Preconception health optimization
- Fertility awareness methods
- Signs and symptoms requiring medical attention
Cultural Competency Considerations
- Respect for diverse cultural beliefs about reproduction
- Language-appropriate education materials
- Gender-sensitive care delivery approaches
- Religious and spiritual considerations
- Socioeconomic factors affecting access to care
- LGBTQ+ inclusive reproductive health services
- Trauma-informed care principles
Quality Indicators for Reproductive Health Nursing
Effective reproductive health nursing demonstrates:
Clinical Outcomes
- Improved contraceptive adherence
- Reduced STI transmission rates
- Enhanced fertility outcomes
- Decreased pregnancy complications
Patient Satisfaction
- Increased knowledge confidence
- Positive care experiences
- Improved communication with providers
- Enhanced self-advocacy skills
System Performance
- Efficient care coordination
- Reduced emergency visits
- Improved screening rates
- Enhanced population health metrics
Conclusion: Integrating Knowledge for Optimal Reproductive Health
Understanding reproduction from both biological and clinical perspectives provides nursing students with a comprehensive foundation for delivering excellent reproductive health care. The parallels between plant and human reproduction demonstrate universal biological principles, while the complexity of human reproductive health requires sophisticated nursing knowledge and skills.
Effective reproductive health nursing integrates anatomical knowledge, physiological understanding, cultural competency, and evidence-based practice principles. By recognizing reproductive health as encompassing physical, mental, and social well-being, nurses can provide holistic care that supports individuals and families throughout their reproductive journey.
Key Takeaways for Nursing Practice
- Reproductive health extends beyond disease prevention to encompass overall well-being
- Understanding biological processes enhances clinical assessment and patient education capabilities
- Cultural competency and patient-centered care are essential for effective reproductive health services
- Evidence-based practice principles guide optimal reproductive health interventions
- Ongoing education and professional development support high-quality reproductive health nursing
Recommended Resources for Further Learning
Professional Organizations
- • Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN)
- • National Association of Nurse Practitioners in Women’s Health (NPWH)
- • International Childbirth Education Association (ICEA)
Key Clinical Guidelines
- • CDC Reproductive Health Guidelines
- • ACOG Practice Bulletins
- • WHO Reproductive Health Publications
