Quick Facts
- ROP is a vasoproliferative disorder affecting the developing retina of premature infants
- It is a leading cause of preventable childhood blindness worldwide
- Primarily affects infants born before 31 weeks of gestation or with birth weight less than 1500g
- Oxygen therapy is a major contributing risk factor
- Early detection through screening and timely intervention can prevent vision loss
Pathophysiology of ROP
Normal Retinal Development
In a normal term infant, the retinal blood vessels begin developing at 16 weeks of gestation from the optic nerve and grow outward to reach the periphery of the retina by 36-40 weeks. This vascularization process is regulated by vascular endothelial growth factor (VEGF), which is produced in response to physiological hypoxia in the developing retina.
Two-Phase Disease Process
Phase 1: Vaso-obliteration
- Occurs from birth to 30-32 weeks postmenstrual age
- Exposure to high oxygen levels causes suppression of VEGF
- Leads to arrest of normal retinal vascular development
- Existing immature vessels constrict and regress
- Results in avascular areas in the peripheral retina
Phase 2: Vasoproliferation
- Begins around 32-34 weeks postmenstrual age
- Avascular retina becomes increasingly metabolically active
- Local hypoxia triggers overproduction of VEGF
- Abnormal blood vessel growth at junction of vascular and avascular retina
- Can lead to fibrovascular proliferation, hemorrhage, and retinal detachment
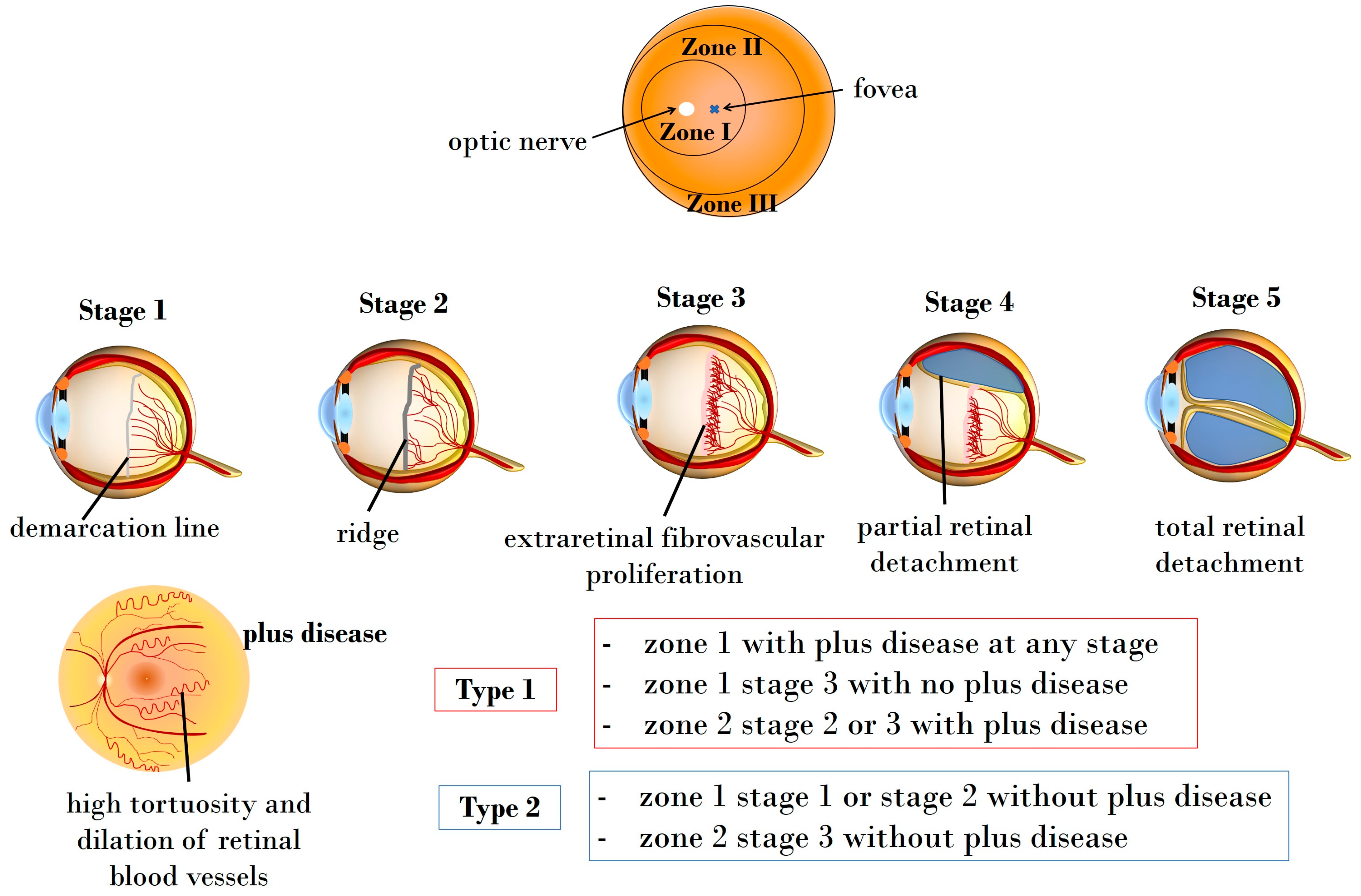
Figure 1: Pathophysiology of Retinopathy of Prematurity showing the two phases of the disease and the role of oxygen
Risk Factors for ROP
| Category | Risk Factors |
|---|---|
| Major Risk Factors |
|
| Secondary Risk Factors |
|
| Protective Factors |
|
Clinical Features & Classification
Location: Zones of the Retina

Figure 2: Zones of the retina in ROP classification
-
Zone I
Circle with radius of 2x the distance from optic disc to macula
This is the most posterior region of the retina. ROP in Zone I is the most severe form as it affects the central vision and has the worst prognosis.
-
Zone II
Extends from edge of Zone I to the nasal ora serrata
This is the middle zone. ROP in Zone II is less severe than Zone I but still requires close monitoring and often treatment.
-
Zone III
Remaining temporal crescent of retina
This is the most peripheral zone. ROP in Zone III generally has the best prognosis and often resolves spontaneously.
Severity: Stages of ROP

Figure 3: Schematic representation of ROP stages
-
Stage 1
Demarcation Line
Thin, flat white line at the junction of vascularized and avascular retina.
-
Stage 2
Ridge
The line has height and width, becoming an elevated ridge.
-
Stage 3
Ridge with Extraretinal Fibrovascular Proliferation
Abnormal blood vessels and fibrous tissue grow from the ridge into the vitreous.
-
Stage 4
Partial Retinal Detachment
4A: Not involving the macula (better prognosis)
4B: Involving the macula (worse prognosis) -
Stage 5
Total Retinal Detachment
Complete detachment of the retina, usually in a funnel shape. Poor visual prognosis.
Plus Disease
An additional qualifier that can be added to any stage indicating increased disease activity and greater risk of progression:
- Vascular dilation and tortuosity of posterior retinal vessels
- Iris vascular engorgement
- Pupillary rigidity
- Vitreous haze
Pre-plus disease refers to vascular abnormalities of the posterior pole that are insufficient for the diagnosis of plus disease but demonstrate more arterial tortuosity and venous dilation than normal.
Classification Summary
| Classification | Description | Clinical Significance |
|---|---|---|
| Type 1 ROP (Requires Treatment) |
|
High risk for poor outcomes if untreated. Requires urgent treatment within 72 hours of diagnosis. |
| Type 2 ROP (Observation) |
|
Lower risk, but requires close monitoring twice weekly to detect progression to type 1 ROP. |
| Aggressive Posterior ROP (APROP) | Severe form with rapidly progressing vascular changes, typically in Zone I or posterior Zone II, with prominent plus disease. | Very aggressive and rapidly progressive form that requires immediate treatment. Poor prognosis if not treated promptly. |
Screening Guidelines
Who to Screen
Screening Criteria
- All infants with birth weight ≤1500 grams
- All infants born at ≤30 weeks gestational age
- Selected infants with birth weight 1500-2000 grams or gestational age >30 weeks with an unstable clinical course who are believed to be at high risk (as determined by the attending neonatologist)
Timing of Initial Screening
| Gestational Age at Birth | Age at Initial Examination |
|---|---|
| 22-26 weeks | 31 weeks postmenstrual age |
| 27-28 weeks | 4 weeks chronological age |
| 29-30 weeks | 4 weeks chronological age |
| 31-32 weeks | 4 weeks chronological age |
| ≥33 weeks | 4 weeks chronological age |
Follow-up Recommendations
- 1-week follow-up or less:
- Zone I, immature vascularization
- Zone I, stage 1 or 2 ROP
- Zone II, stage 3 ROP
- Any zone with plus or pre-plus disease
- 1-2 week follow-up:
- Zone II, immature vascularization
- Zone II, stage 1 or 2 ROP
- 2-week follow-up:
- Zone III, stage 1 or 2 ROP
- Regressing ROP in Zone I
- 2-3 week follow-up:
- Zone III, immature vascularization
- Regressing ROP in Zone II
Termination of Acute-Phase Screening
Screening examinations can be terminated when ANY of the following criteria are met:
- Full retinal vascularization in close proximity to the ora serrata for 360° (the normal adult pattern)
- Zone III retinal vascularization attained without previous Zone I or II ROP (if there is doubt about the zone or if the postmenstrual age is less than 35 weeks, confirmatory examinations may be warranted)
- Postmenstrual age of 50 weeks and no pre-threshold disease (defined as stage 3 ROP in zone II, any ROP in zone I) or worse ROP is present
- Regression of ROP (ensuring there is no abnormal vascular tissue that is capable of reactivation and progression)
Screening Procedure
Preparation
Dilate pupils with cycloplegic eye drops (e.g., tropicamide 0.5% and phenylephrine 2.5%) approximately 30-60 minutes before the examination.
Positioning and Comfort Measures
Position the infant securely, administer oral sucrose solution and provide non-nutritive sucking to reduce pain and discomfort. Consider swaddling the infant.
Examination
The ophthalmologist uses an indirect ophthalmoscope with a specialized lens and a lid speculum to visualize the retina. The examination typically takes 3-5 minutes.
Documentation
The ophthalmologist documents findings including zone, stage, extent (clock hours), presence of plus disease, and recommendations for follow-up or treatment.
Post-Examination Care
Monitor the infant for signs of distress, bradycardia, or apnea. Provide comfort measures and resume regular feeding when the infant is stable.
Nursing Management & Interventions
Prevention Strategies
The “PREEMIE” Mnemonic for ROP Prevention
Oxygen Management: The Nurse’s Critical Role
| Nursing Intervention | Rationale |
|---|---|
| Set and maintain oxygen saturation targets between 89-94% (or as per unit protocol) | Prevents hyperoxia that suppresses VEGF and contributes to vaso-obliteration in Phase 1 of ROP |
| Set pulse oximeter alarms appropriately (lower alarm at 88%, upper alarm at 95%) | Ensures prompt response to oxygen saturation outside target range |
| Respond quickly to alarms and adjust oxygen accordingly | Minimizes duration of hyperoxia or hypoxia, both of which can contribute to ROP development |
| Avoid fluctuations in oxygen levels | Fluctuations between hyperoxia and hypoxia can be more damaging than consistent hypoxia |
| Document oxygen adjustments and saturations regularly | Allows for trend identification and quality improvement |
| Ensure proper functioning of oxygen delivery equipment | Prevents unintended oxygen delivery issues |
| Coordinate care to minimize handling during procedures that may affect oxygenation | Reduces fluctuations in oxygen saturation related to stimulation or procedures |
Pain Management During ROP Screening
Pharmacological Interventions
- Topical anesthetic drops (e.g., proparacaine 0.5%) 2-3 minutes before examination
- Oral sucrose solution (24%) 2 minutes before and during examination
- Consider acetaminophen for post-procedure pain if needed
Non-Pharmacological Interventions
- Facilitated tucking (holding the infant’s arms and legs in a flexed, midline position)
- Swaddling
- Non-nutritive sucking (pacifier)
- Gentle containment
- Minimize light and noise in the environment
ROP Positioning Technique
Research has shown that a specialized positioning technique called “ROP position” can reduce pain during eye examinations:
- Wrap the infant securely with a blanket
- Support the head and neck in midline
- Place both hands on the infant’s sides, providing gentle but firm boundaries
- Maintain flexion of the extremities
- Provide verbal comfort with soft, soothing voice
This positioning helps maintain physiological flexion posture and reduces stress responses during the examination.
Nursing Roles During ROP Screening and Treatment
Before Screening
- Ensure informed consent has been obtained from parents
- Administer mydriatic eye drops as ordered (usually 30-60 minutes before examination)
- Document pupil dilation
- Prepare the environment (dim lighting, minimize noise)
- Ensure the infant has been fed 30-60 minutes before the exam to reduce hunger during the procedure
- Prepare pain management interventions (sucrose solution, pacifier)
- Position infant appropriately
During Screening
- Assist the ophthalmologist as needed
- Monitor vital signs, especially heart rate and oxygen saturation
- Provide containment and comfort measures
- Administer sucrose if crying or distress occurs
- Be prepared to pause the examination if the infant shows signs of severe distress or physiological instability
After Screening
- Continue comfort measures and containment
- Monitor for adverse effects (apnea, bradycardia, desaturation)
- Resume regular care when the infant is stable
- Document findings and next screening date prominently
- Schedule follow-up appointment as recommended
- Educate parents about findings and importance of follow-up
During Treatment (if needed)
- Prepare infant for laser therapy or anti-VEGF injection
- Assist with anesthesia if required
- Monitor vital signs throughout procedure
- Assist with positioning and stabilization
- Prepare post-procedure medications (antibiotics, steroids) as ordered
Treatment Options for ROP
Laser Photocoagulation
Procedure Overview
Laser photocoagulation is the gold standard treatment for Type 1 ROP. The procedure involves:
- Ablation of the avascular peripheral retina
- Usually performed under sedation or general anesthesia
- Typically takes 30-60 minutes to complete both eyes
- May be performed in the NICU or operating room
Nursing Considerations
- Ensure NPO status as directed for sedation
- Assist with sedation or anesthesia as needed
- Monitor vital signs before, during, and after procedure
- Administer post-procedure medications as ordered
- Monitor for complications (inflammation, increased IOP)
- Educate parents about post-procedure care and follow-up
Anti-VEGF Therapy
Procedure Overview
Anti-VEGF injections (e.g., bevacizumab, ranibizumab) are increasingly used, especially for Zone I ROP or APROP:
- Intravitreal injection of anti-VEGF medication
- Quick procedure (usually less than 5 minutes per eye)
- May be performed under topical anesthesia or sedation
- Often performed in the NICU
Nursing Considerations
- Prepare sterile field for injection
- Administer topical antibiotics as ordered
- Monitor for infection signs (redness, discharge)
- Be aware that anti-VEGF agents can enter systemic circulation
- Extended follow-up is crucial as late recurrences can occur
- Monitor for systemic complications
Surgical Interventions for Advanced ROP
| Procedure | Indication | Nursing Considerations |
|---|---|---|
| Scleral Buckling | Stage 4 ROP with partial retinal detachment |
|
| Vitrectomy | Stage 4B or 5 ROP with subtotal or total retinal detachment |
|
| Lens-Sparing Vitrectomy | Stage 4 ROP, preserves the lens for better visual rehabilitation |
|
Treatment Comparison
| Treatment Modality | Advantages | Disadvantages | Success Rate |
|---|---|---|---|
| Laser Photocoagulation |
|
|
~90% for Type 1 ROP |
| Anti-VEGF Therapy |
|
|
~80-95% (varies by agent) |
| Surgical Interventions |
|
|
~20-60% anatomical success, but limited functional vision |
Parent Education & Follow-up Care
Key Education Points for Parents
Understanding ROP
- Basic explanation of ROP and how it affects the eyes
- Risk factors and why their baby is at risk
- Potential outcomes and importance of early detection
- Different stages of the disease and what they mean
- Natural course and possible regression
Screening Process
- Why screening is necessary
- What happens during the examination
- How often screenings will occur
- How parents can help prepare and comfort their baby
- What to expect after the screening
Follow-up Care
- Importance of keeping all appointments
- Potential consequences of missed follow-ups
- What to bring to appointments
- How to find an ophthalmologist after discharge
- Long-term follow-up needs
Warning Signs
- Abnormal eye appearance (white pupil, crossed eyes)
- Lack of visual tracking or fixation
- Abnormal eye movements (nystagmus)
- Signs of eye infection (redness, discharge)
- When to seek immediate medical attention
Follow-up Care Schedule
| Time Period | Recommended Follow-up | Focus of Assessment |
|---|---|---|
| NICU Discharge to 6 months | According to ROP screening schedule, typically every 1-2 weeks until retina fully vascularized or ROP resolved | ROP progression or regression, retinal vascularization |
| 6-12 months | Every 2-3 months | Refractive errors, amblyopia, strabismus, late ROP sequelae |
| 1-2 years | Every 4-6 months | Visual function, refractive errors, amblyopia, strabismus |
| 2-5 years | Every 6-12 months | Visual acuity, refractive errors, amblyopia, strabismus |
| 5+ years | Annually | Visual acuity, refractive errors, late complications (glaucoma, retinal detachment, myopia) |
Discharge Planning Checklist
- Confirm first follow-up appointment with ophthalmologist is scheduled
- Ensure parents have written documentation of ROP status and follow-up plan
- Provide contact information for ophthalmologist
- Discuss transportation needs for appointments
- Provide educational materials about ROP
- Connect parents with support resources
- Ensure primary care provider is aware of ROP status and follow-up plan
Long-term Visual Outcomes & Complications
Potential Long-term Complications
- Refractive Errors: High myopia (nearsightedness) is common in ROP-treated eyes
- Strabismus: Misalignment of the eyes
- Amblyopia: “Lazy eye” or reduced vision due to abnormal development
- Glaucoma: Increased pressure in the eye
- Cataract: Clouding of the lens
- Late Retinal Detachment: Can occur years after initial ROP
- Visual Field Defects: Especially after laser treatment
- Nystagmus: Involuntary eye movements
Visual Support and Interventions
- Glasses or Contact Lenses: For refractive errors
- Patching: For amblyopia treatment
- Vision Therapy: To improve visual function
- Early Intervention Programs: For developmental support
- Low Vision Aids: For those with permanent visual impairment
- Educational Support: Including Individualized Education Plans (IEPs)
- Mobility Training: For those with significant visual impairment
- Assistive Technology: To support learning and independence
Resources for Parents and Families
Organizations and Websites
- National Eye Institute: www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/retinopathy-prematurity
- American Association for Pediatric Ophthalmology and Strabismus: aapos.org/patients/patient-resources/retinopathy-of-prematurity
- March of Dimes: www.marchofdimes.org
- Prevent Blindness: preventblindness.org
- Graham’s Foundation (for parents of preemies): grahamsfoundation.org
Support Services
- Early Intervention Services: Available in all states for children with developmental delays or disabilities
- Family Support Groups: Connect with other families dealing with ROP
- Social Work Services: For assistance with medical costs, transportation, and other needs
- Respite Care: For parents who need temporary relief from caregiving
- State Services for Children with Visual Impairments: Educational and developmental support
Summary & Key Points
ROP Management Mind Map

Figure 4: Comprehensive approach to ROP management including screening, prevention, and treatment
The “NURSE” Mnemonic for ROP Management
Final Thoughts
Retinopathy of prematurity is a complex condition that requires a multidisciplinary approach involving neonatologists, ophthalmologists, nurses, and parents. As a neonatal nurse, you play a pivotal role in prevention, early detection, and management of ROP.
Your careful attention to oxygen management, facilitation of screening examinations, pain management during procedures, and parent education can significantly impact outcomes for premature infants at risk for ROP.
Remember that many cases of ROP resolve spontaneously without treatment, but diligent monitoring is essential to identify those cases that require intervention. With appropriate screening, timely treatment, and comprehensive follow-up care, most infants with ROP can have favorable visual outcomes.
References & Further Reading
- American Academy of Pediatrics Section on Ophthalmology. (2018). Screening examination of premature infants for retinopathy of prematurity. Pediatrics, 142(6), e20183061.
- Hellström, A., Smith, L. E., & Dammann, O. (2013). Retinopathy of prematurity. The Lancet, 382(9902), 1445-1457.
- Fierson, W. M. (2018). Screening examination of premature infants for retinopathy of prematurity. Pediatrics, 142(6), e20183061.
- Quinn, G. E. (2016). Retinopathy of prematurity blindness worldwide: phenotypes in the third epidemic. Eye and brain, 8, 31-36.
- Hartnett, M. E., & Penn, J. S. (2012). Mechanisms and management of retinopathy of prematurity. New England Journal of Medicine, 367(26), 2515-2526.
- Gilbert, C. (2008). Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early human development, 84(2), 77-82.
- Blencowe, H., Lawn, J. E., Vazquez, T., Fielder, A., & Gilbert, C. (2013). Preterm-associated visual impairment and estimates of retinopathy of prematurity at regional and global levels for 2010. Pediatric research, 74(S1), 35-49.
- Sun, H., Kang, W., Cheng, X., Chen, C., Xiong, H., Guo, J., … & Zhou, C. (2019). The use of the WINROP screening algorithm for the prediction of retinopathy of prematurity in a Chinese population. Neonatology, 116(1), 24-29.
- Chen, J., Stahl, A., Hellstrom, A., & Smith, L. E. (2011). Current update on retinopathy of prematurity: screening and treatment. Current opinion in pediatrics, 23(2), 173-178.
- Mintz-Hittner, H. A., Kennedy, K. A., & Chuang, A. Z. (2011). Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. New England Journal of Medicine, 364(7), 603-615.
