Revised National Tuberculosis Control Programme (RNTCP): A Community Health Nursing Perspective
- 1. Introduction
- 2. Evolution and History of RNTCP
- 3. Organizational Structure and Framework
- 4. Goals and Objectives
- 5. DOTS Strategy: The Core Approach
- 6. Case Finding and Diagnosis Strategies
- 7. Treatment Categories and Regimens
- 8. Role of Community Health Nurse in RNTCP
- 9. Prevention Strategies
- 10. Challenges and Future Directions
- 11. Useful Mnemonics for Nursing Students
- 12. Global Best Practices
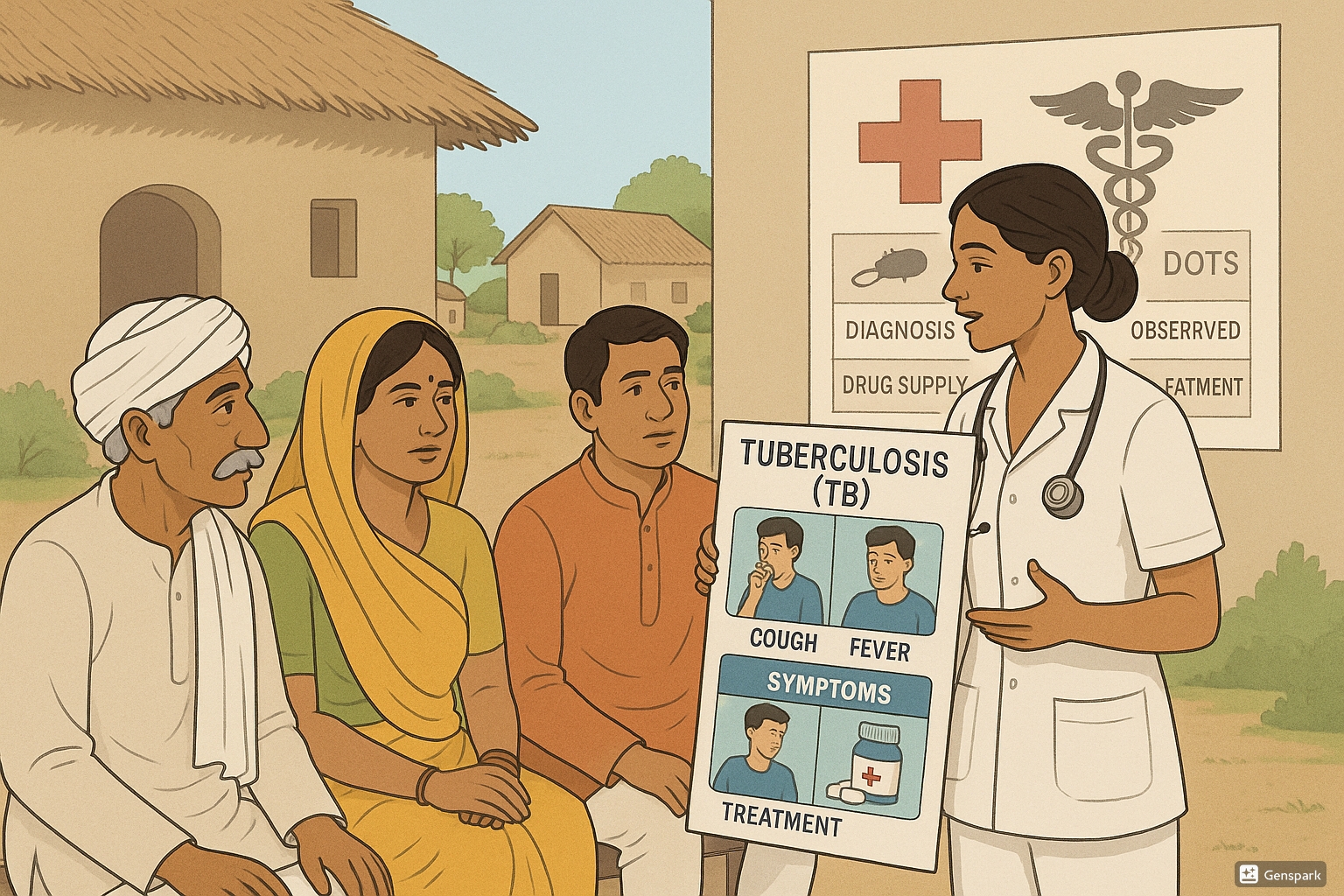
Community health nurse conducting tuberculosis screening and providing DOTS education in a rural Indian village
1. Introduction
Tuberculosis (TB) remains one of India’s most significant public health challenges, affecting millions of lives annually. India accounts for approximately one-fourth of the global tuberculosis burden. To combat this persistent threat, the Government of India launched the Revised National Tuberculosis Control Programme (RNTCP) in 1997, which has now evolved into the National Tuberculosis Elimination Program (NTEP).
Key Facts:
- Tuberculosis is caused by Mycobacterium tuberculosis, primarily affecting the lungs but can involve any organ system
- Approximately 2.8 million new cases of tuberculosis are reported in India annually
- Around 450,000 people die from tuberculosis each year in India
- RNTCP was renamed as National Tuberculosis Elimination Program (NTEP) in January 2020
- India aims to eliminate tuberculosis by 2025, five years ahead of global targets
2. Evolution and History of RNTCP
The journey of India’s fight against tuberculosis has seen several transformations over the decades:
| Time Period | Program Phase | Key Features |
|---|---|---|
| 1962 | National Tuberculosis Program (NTP) | First organized effort; district TB centers; BCG vaccination focus; domiciliary treatment |
| 1993 | RNTCP Pilot Phase | DOTS strategy pilot implementation in select districts |
| 1997 | RNTCP National Launch | Full-scale implementation of DOTS; standardized treatment protocols |
| 2006 | RNTCP Phase II | Nationwide coverage; MDR-TB management; public-private partnerships |
| 2017-2025 | National Strategic Plan | “Detect-Treat-Prevent-Build” strategy; focus on TB elimination |
| 2020 | NTEP Transition | RNTCP renamed as NTEP; elimination goal set for 2025 |
The evolution of the program reflects the growing understanding of tuberculosis control and the adaptation of international best practices to India’s unique healthcare context. The emphasis has gradually shifted from control to elimination, with increasingly ambitious targets and comprehensive strategies.
3. Organizational Structure and Framework
The RNTCP/NTEP is structured as a four-level hierarchy to ensure effective implementation across India’s diverse geographical and demographic settings:
National Level
- Central TB Division under Ministry of Health and Family Welfare
- National TB Institute (NTI) in Bangalore
- National Reference Laboratories
- Policy formulation and program monitoring
State Level
- State TB Cell (STC)
- State TB Training and Demonstration Center (STDC)
- Intermediate Reference Laboratories
- Program implementation and supervision
District Level
- District TB Center (DTC)
- District TB Officer (DTO)
- District Program Manager
- Supervision of TB Control activities
Sub-District (Tuberculosis Unit) Level
- TB Unit serving 250,000-500,000 population
- Medical Officer-TB Control (MO-TC)
- Senior Treatment Supervisor (STS)
- Senior TB Laboratory Supervisor (STLS)
- Direct implementation and monitoring
At the peripheral level, Designated Microscopy Centers (DMCs) and DOTS providers (including community health workers, community health nurses, and volunteers) form the backbone of service delivery. Community health facilities, Primary Health Centers (PHCs), Community Health Centers (CHCs), and district hospitals all play crucial roles in the implementation network.
4. Goals and Objectives
The NTEP’s goals have evolved from controlling tuberculosis to eliminating it as a public health problem in India.
Current NTEP Goals
Primary Goal: To eliminate tuberculosis in India by 2025 (five years ahead of global target)
Key Targets (baseline 2015):
- 80% reduction in tuberculosis incidence
- 90% reduction in tuberculosis mortality
- Zero catastrophic expenses for affected families
Original RNTCP Objectives
- Achieve at least 85% treatment success among new smear-positive TB patients
- Detect at least 70% of estimated new smear-positive TB cases
- Ensure universal access to quality TB care for all patients
- Reduce transmission of infection in the community
- Prevent emergence of drug resistance
The strategic pillars of the current National Strategic Plan (2017-2025) are organized under the “Detect-Treat-Prevent-Build” (DTPB) framework:
Detect
- Early identification of presumptive TB cases
- Active case finding in high-risk populations
- Universal rapid molecular diagnostics
- Systematic screening of contacts
Treat
- Universal access to drug susceptibility testing
- Patient-friendly treatment services
- Nutritional and social support to patients
- Private sector engagement for comprehensive care
Prevent
- Airborne infection control
- Treatment of latent TB infection
- Address social determinants of TB
- BCG vaccination
Build
- Strengthening surveillance systems
- Community engagement and awareness
- Research capacity and implementation
- Human resource development
5. DOTS Strategy: The Core Approach
The Directly Observed Treatment, Short-course (DOTS) strategy remains the cornerstone of India’s tuberculosis control efforts. It is implemented as a comprehensive package with five key components:
- Support – Political and administrative commitment
- Proper diagnosis – Quality-assured sputum microscopy and other diagnostic tools
- Observed treatment – Standardized treatment with supervision and patient support
- Track supplies – Effective drug supply and management system
- Surveillance – Monitoring and evaluation system
Under DOTS, treatment is administered under direct observation of a trained health worker or community volunteer (DOTS provider) at least during the intensive phase of treatment. This approach ensures:
- Regular intake of all prescribed drugs
- Completion of the full course of treatment
- Early identification of side effects and complications
- Prevention of drug resistance development
- Better patient outcomes with higher cure rates
Role of DOTS Providers
DOTS providers can be healthcare workers, community volunteers, or family members who are trained to:
- Directly observe patients taking their medications
- Record medication consumption in treatment cards
- Provide motivational support to patients
- Follow up on missed doses
- Report adverse drug reactions
- Facilitate follow-up sputum examinations
Community health nurses often serve as DOTS providers and play a vital role in the success of the program through their patient-centered approach and community reach. This strategy has significantly improved treatment outcomes compared to the previous self-administered treatment approach.
6. Case Finding and Diagnosis Strategies
Early and accurate diagnosis is essential for effective tuberculosis control. The RNTCP/NTEP employs various case-finding strategies:
Passive Case Finding
Identifying TB cases among symptomatic individuals who present themselves to health facilities
- Symptom screening (cough >2 weeks, fever, weight loss, night sweats)
- Sputum examination of symptomatic individuals
- Requires patient awareness and healthcare access
Active Case Finding
Proactively searching for TB cases in communities, especially among high-risk groups
- House-to-house visits in high-prevalence areas
- Targeted screening of contacts of TB patients
- Screening in congregate settings (prisons, slums, factories)
- Mobile TB detection vans with X-ray facilities
Diagnostic Methods
The program employs a range of diagnostic tools, from conventional to advanced:
| Diagnostic Method | Description | Application |
|---|---|---|
| Sputum Smear Microscopy | Examination of sputum for acid-fast bacilli (AFB) | Primary diagnostic tool; two samples collected (spot and morning) |
| Cartridge Based Nucleic Acid Amplification Test (CBNAAT/GeneXpert) | Molecular test detecting TB DNA and rifampicin resistance | Priority groups: HIV-TB co-infection, children, suspected drug resistance |
| Line Probe Assay (LPA) | Molecular test for detecting resistance to first and second-line drugs | Drug resistance testing at reference laboratories |
| Chest X-ray | Radiological examination of lungs | Supplementary tool; especially for smear-negative TB |
| Culture and Drug Susceptibility Testing (DST) | Growing TB bacilli and testing drug sensitivity | Confirmation of diagnosis and comprehensive resistance profile |
| TrueNat | Portable molecular diagnostic system | Rapid point-of-care testing; useful in peripheral settings |
Case Definition in RNTCP/NTEP
Presumptive TB: Any person with signs and symptoms suggestive of TB, particularly:
- Persistent cough for two weeks or more
- Fever for two weeks or more
- Significant weight loss
- Night sweats
- Hemoptysis (blood in sputum)
Bacteriologically Confirmed TB: A case where a biological specimen is positive by smear microscopy, culture, or WRD (WHO-recommended rapid diagnostic test).
Clinically Diagnosed TB: A case that does not fulfill the criteria for bacteriological confirmation but diagnosed as TB by a clinician who has decided to give the patient a full course of TB treatment.
7. Treatment Categories and Regimens
The RNTCP/NTEP follows standardized treatment regimens based on the patient’s disease classification, previous treatment history, and drug sensitivity:
Treatment Classification
| Patient Type | Definition |
|---|---|
| New | Patient who has never been treated for TB or has taken anti-TB drugs for less than one month |
| Relapse | Patient previously treated for TB, declared cured or treatment completed, and now diagnosed with TB again |
| Treatment after failure | Patient previously treated for TB and whose treatment failed at the end of their most recent course |
| Treatment after loss to follow-up | Patient who received TB treatment for at least one month and was declared lost to follow-up |
| Others | Patients who do not fit into any of the above categories |
Current Treatment Regimens
Under NTEP, daily regimens have replaced the earlier thrice-weekly regimens. The key drug regimens include:
Drug-Sensitive TB
- New cases: 2HRZE/4HRE
- Intensive Phase: 2 months of Isoniazid (H), Rifampicin (R), Pyrazinamide (Z), and Ethambutol (E)
- Continuation Phase: 4 months of Isoniazid, Rifampicin, and Ethambutol
- Previously treated cases: 2HRZES/1HRZE/5HRE
- Intensive Phase: 2 months of HRZE + Streptomycin (S), followed by 1 month of HRZE
- Continuation Phase: 5 months of HRE
Drug-Resistant TB
Multi-Drug Resistant TB (MDR-TB): Standardized Treatment Regimen (STR) based on resistance pattern:
- Shorter MDR-TB Regimen: 4-6 Km-Mfx-Pto-Cfz-Z-E-Hh/5 Mfx-Cfz-Z-E (9-11 months total)
- Longer MDR-TB Regimen: 6-9 months intensive phase with 6 drugs (kanamycin, ofloxacin, ethionamide, pyrazinamide, ethambutol, cycloserine) followed by 18 months of 4 drugs (ofloxacin, ethionamide, ethambutol, cycloserine)
Extensively Drug-Resistant TB (XDR-TB): Individualized regimens based on Drug Susceptibility Testing (DST) results, including newer drugs like Bedaquiline and Delamanid
- Rifampicin – Bactericidal, inhibits RNA synthesis
- Isoniazid – Bactericidal, inhibits mycolic acid synthesis
- Pyrazinamide – Bactericidal in acidic environment
- Ethambutol – Bacteriostatic, inhibits cell wall synthesis
Treatment Monitoring
Regular monitoring is essential to track treatment progress and identify complications:
- Follow-up sputum examinations: At the end of intensive phase, 2 months into continuation phase, and at the end of treatment
- Clinical assessment: Weight monitoring, symptom assessment, and side effect monitoring
- Treatment outcome recording: Using standardized RNTCP/NTEP definitions (cured, treatment completed, treatment failed, died, lost to follow-up, not evaluated)
8. Role of Community Health Nurse in RNTCP
Community health nurses play a pivotal role in the success of the RNTCP/NTEP through their direct patient contact and community presence. Their responsibilities encompass various aspects of tuberculosis control:
Case Finding and Referral
- Identifying presumptive TB cases during home visits
- Screening contacts of TB patients for symptoms
- Organizing TB symptom screening camps
- Referring symptomatic individuals to diagnostic centers
- Collecting sputum samples and ensuring proper transportation
DOTS Implementation
- Serving as DOTS providers
- Ensuring directly observed medication intake
- Maintaining treatment cards and records
- Tracking and tracing treatment defaulters
- Coordinating with TB Unit for patient management
Patient Education and Counseling
- Educating patients about TB and its treatment
- Addressing misconceptions and stigma
- Advocating for treatment adherence
- Providing emotional support to patients and families
- Counseling on nutrition, infection control, and healthy habits
Community Education and Mobilization
- Conducting awareness programs in communities
- Training community volunteers and ASHA workers
- Organizing Information, Education, and Communication (IEC) activities
- Engaging community leaders in TB control efforts
- Promoting early care-seeking behavior
Nursing Process in TB Management
Community health nurses apply the nursing process to provide comprehensive care to TB patients:
- Assessment:
- Conduct thorough history taking and symptom assessment
- Identify risk factors and complications
- Assess home environment for infection control
- Evaluate nutritional status and support systems
- Nursing Diagnosis:
- Ineffective breathing pattern related to pulmonary inflammation
- Risk for infection transmission related to airborne pathogens
- Imbalanced nutrition: less than body requirements
- Knowledge deficit regarding disease process and treatment
- Risk for non-adherence related to lengthy treatment
- Planning:
- Develop patient-centered care plans
- Set achievable goals for treatment adherence
- Plan for follow-up visits and sputum examinations
- Coordinate with other healthcare providers
- Implementation:
- Direct observation of treatment
- Health education and counseling
- Home visits for monitoring and support
- Infection control measures implementation
- Referrals for complications or social support
- Evaluation:
- Monitor treatment response and sputum conversion
- Assess improvement in clinical symptoms
- Evaluate adherence to treatment plan
- Document and report outcomes
9. Prevention Strategies
The RNTCP/NTEP incorporates various prevention strategies to reduce tuberculosis transmission and disease progression:
BCG Vaccination
- Administered to all newborns at birth under Universal Immunization Programme
- Provides protection against severe forms of TB in children (TB meningitis, miliary TB)
- Limited effectiveness against pulmonary TB in adults
- Single-dose strategy in India, no boosters recommended
Infection Control Measures
- Administrative controls (early diagnosis, separation of infectious cases)
- Environmental controls (proper ventilation, UV germicidal irradiation)
- Personal protective equipment (N95 respirators for healthcare workers)
- Cough hygiene education for patients
Contact Investigation
- Systematic screening of household contacts of TB patients
- Priority to children under 5 years and people living with HIV
- Symptom screening, tuberculin skin testing, and/or chest X-ray
- Provision of isoniazid preventive therapy (IPT) for eligible contacts
Preventive Treatment
- Isoniazid Preventive Therapy (IPT) for high-risk groups
- 6-9 months of isoniazid for HIV-positive individuals
- TPT (TB Preventive Treatment) for household contacts
- Newer shorter regimens (3HP, 3RH) being introduced
Social Determinants Approach
Addressing underlying social factors contributing to TB:
- Improved housing and reduced overcrowding
- Nutritional support for TB patients and vulnerable populations
- Reduction of indoor air pollution
- Addressing comorbidities like diabetes and HIV
- Tackling tobacco and alcohol use
- Socioeconomic support through Direct Benefit Transfer (DBT) and Nikshay Poshan Yojana
Community health nurses play a vital role in implementing these prevention strategies through their work in maternal and child health services, school health programs, and community outreach activities.
10. Challenges and Future Directions
Despite significant progress, several challenges remain in India’s journey toward tuberculosis elimination:
Current Challenges
- Large number of unreported/”missing” cases
- Rising drug resistance (MDR-TB and XDR-TB)
- TB-HIV co-infection management
- Private sector engagement and regulation
- Stigma and discrimination
- Treatment adherence issues
- Urban slums and difficult-to-reach populations
- Inadequate human resources and infrastructure
- Impact of COVID-19 pandemic on TB services
Future Directions
- Digital initiatives (Nikshay portal, 99DOTS, e-vouchers)
- Artificial Intelligence for chest X-ray interpretation
- Shorter treatment regimens for drug-sensitive and DR-TB
- Novel diagnostic tools with higher sensitivity
- Mobile health applications for patient support
- Community engagement and empowerment
- Integration with Ayushman Bharat and Health & Wellness Centers
- Research on new vaccines and drugs
- Stronger cross-sectoral collaboration
Role of Community Health Nursing in Future TB Control
As India moves toward TB elimination, community health nurses will need to evolve their practice in several ways:
- Greater use of digital tools for patient tracking and support
- Enhanced skills in managing drug-resistant TB
- Integrated care approach addressing TB and comorbidities
- Evidence-based nursing interventions for hard-to-reach populations
- Research participation and evidence generation
- Policy advocacy and community mobilization
- Collaboration with private sector providers
11. Useful Mnemonics for Nursing Students
Memory aids to help nursing students remember key aspects of tuberculosis control:
- Tiredness and fatigue
- Blood in sputum (hemoptysis)
- Fever, especially in evening
- Anorexia (loss of appetite)
- Cough for more than two weeks
- Thoracic pain (chest pain)
- Sweats at night
- Notify all TB cases to authorities
- Understand and educate about treatment regimens
- Refer symptomatic individuals for diagnosis
- Support patients through treatment journey
- Ensure infection control at home and community
- Screen contacts for TB symptoms
- Trust-building with patients
- Regular follow-up and monitoring
- Education about disease and treatment
- Addressing side effects promptly
- Timing medications appropriately
- Treatment observation (DOTS)
- Behavioral support and motivation
- Hygiene education (especially respiratory hygiene)
- Open windows for ventilation
- Mask use for infectious patients
- Early diagnosis and treatment
- Separation of high-risk contacts when possible
12. Global Best Practices
Several innovative approaches from around the world can inform India’s tuberculosis control efforts:
South Africa: Integration of TB-HIV Services
South Africa has successfully implemented integrated TB-HIV services, offering testing, treatment, and prevention for both conditions at the same facility. This approach has improved case detection and treatment outcomes for co-infected patients.
Relevance for India: Similar integration can be implemented at Health & Wellness Centers under Ayushman Bharat.
Philippines: Nurse-Led TB Care Model
The Philippines has developed a successful model where nurses lead community-based TB care teams, coordinating diagnosis, treatment, and prevention activities at the local level.
Relevance for India: Expanding the leadership role of nurses in TB control at PHCs and urban health centers.
Vietnam: Community-Based TB Prevention
Vietnam’s community-based TB programs engage local volunteers and women’s groups to conduct active case finding and treatment support, significantly increasing case detection rates.
Relevance for India: Engaging self-help groups and community-based organizations in TB control activities.
Peru: Patient-Centered Approach
Peru implemented a comprehensive patient support system including nutritional support, transportation vouchers, and psychosocial counseling, leading to improved treatment adherence.
Relevance for India: Expanding beyond Nikshay Poshan Yojana to include comprehensive patient support services.
WHO’s End TB Strategy: Global Best Practices
The World Health Organization’s End TB Strategy (2016-2035) provides a framework for global TB elimination efforts with three pillars:
- Integrated, patient-centered care and prevention
- Bold policies and supportive systems
- Intensified research and innovation
India’s NTEP aligns with these global pillars while adapting strategies to the local context and setting more ambitious elimination targets.
Conclusion
The Revised National Tuberculosis Control Programme, now known as the National Tuberculosis Elimination Program, represents India’s comprehensive strategy to combat tuberculosis and move toward elimination by 2025. Community health nurses serve as the backbone of this program, providing direct patient care, community education, and serving as the vital link between the healthcare system and the community.
As nursing students and professionals, understanding the structure, strategies, and implementation aspects of this program is essential for effective participation in India’s TB control efforts. The journey toward TB elimination will require sustained commitment, innovation, and community engagement, with nurses playing a pivotal role in this public health mission.
