Second Trimester Physiological Changes and Discomfort Management
Comprehensive Osmosis-style notes for nursing students
Table of Contents
Introduction to the Second Trimester
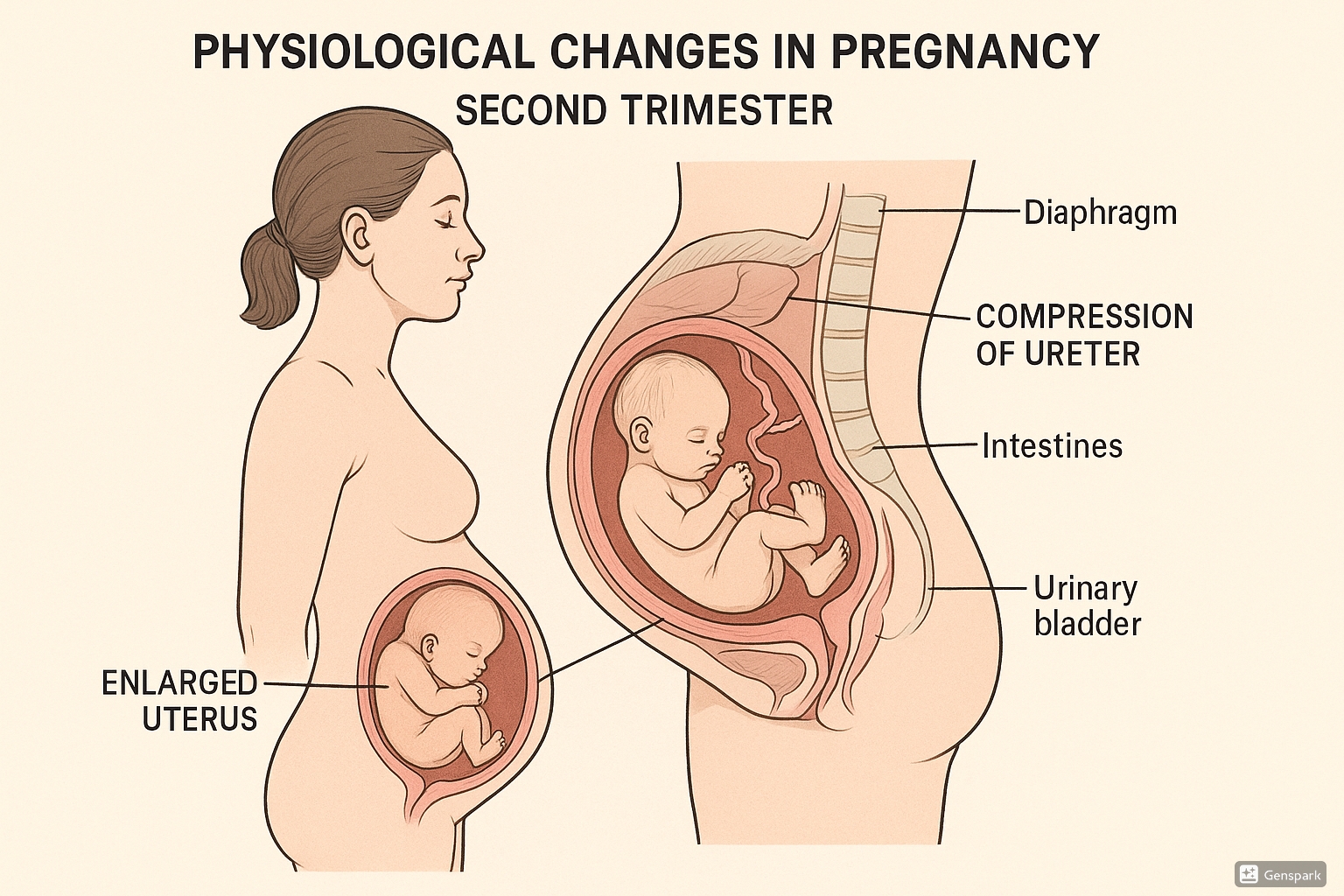
Educational illustration showing physiological changes during the second trimester of pregnancy
The second trimester of pregnancy spans from week 13 to week 27 (months 4-6) and is often referred to as the “golden period” of pregnancy. During this time, many women experience relief from the nausea and fatigue that characterized the first trimester. The second trimester is marked by significant fetal growth and noticeable physiological changes in the mother’s body.
As nursing professionals, understanding these changes is essential for providing comprehensive care, education, and support to pregnant individuals. This knowledge enables nurses to differentiate between normal physiological adaptations and potential complications requiring intervention.
Key Point
The second trimester is characterized by rapid fetal growth, visible physical changes in the pregnant person, and usually a decrease in early pregnancy symptoms like nausea and fatigue.
Timeline and Overview
| Weeks | Key Maternal Changes | Key Fetal Development |
|---|---|---|
| 13-16 |
|
|
| 17-20 |
|
|
| 21-24 |
|
|
| 25-27 |
|
|
Physiological Changes by System
The second trimester is characterized by significant physiological adaptations across multiple body systems to accommodate the growing fetus and prepare for childbirth.
Reproductive System
Uterine Changes
- The uterus grows significantly, rising from the pelvis into the abdominal cavity
- Fundal height increases approximately 4 cm per month
- By week 20, the fundus is typically at the level of the umbilicus
- Uterine weight increases from 50g (pre-pregnancy) to approximately 700g by the end of the second trimester
- Blood flow to the uterus continues to increase
Cervical Changes
- Increased vascularity and softening continues (Goodell’s sign)
- Mucus glands enlarge, secreting thick mucus that forms the operculum (mucus plug)
- The operculum acts as a protective barrier against ascending infections
Vaginal Changes
- Increased vascularization creating a bluish-purple appearance (Chadwick’s sign)
- Vaginal walls thicken and elasticity increases in preparation for delivery
- Increased glycogen content leads to more acidic pH (3.5-6)
- Increased vaginal discharge (leukorrhea) is common
Clinical Relevance
The increased glycogen content in vaginal tissues creates an environment favorable for Candida growth, making pregnant women more susceptible to vaginal thrush during the second trimester.
Cardiovascular System
- Blood volume continues to increase, reaching 30-40% above pre-pregnancy levels by mid-second trimester
- Cardiac output increases by 30-50% above baseline
- Heart rate increases by 10-15 beats per minute
- Systolic and diastolic blood pressure typically remains stable or slightly decreases
- Total systemic vascular resistance decreases by about 20% due to progesterone’s vasodilatory effect
- Supine hypotension syndrome may develop due to vena cava compression by the enlarging uterus
Warning
Supine hypotension syndrome can occur when a pregnant woman lies flat on her back, causing the enlarged uterus to compress the inferior vena cava. This can lead to decreased venous return, reduced cardiac output, and symptoms including dizziness, nausea, and decreased fetal heart rate. Advise pregnant women to avoid prolonged periods in the supine position and to rest in a left lateral position.
Respiratory System
- Oxygen consumption increases by approximately 20%
- Diaphragm elevates by about 4 cm due to the enlarging uterus
- Chest circumference increases by 5-7 cm due to hormonal relaxation of ligaments connecting ribs to sternum
- Subcostal angle widens from approximately 68° to 103° by late pregnancy
- Respiratory rate increases by 1-2 breaths per minute
- Tidal volume increases by 30-50%
- Functional residual capacity decreases by 10-25%
- Nasal mucosa becomes more vascularized, leading to congestion and occasional epistaxis
Clinical Relevance
The increased respiratory effort, combined with a reduced oxygen reserve due to decreased functional residual capacity, makes pregnant women more susceptible to hypoxia during periods of hypoventilation or apnea.
Gastrointestinal System
- Reduced gastrointestinal motility due to progesterone’s smooth muscle relaxant effects
- Decreased lower esophageal sphincter tone, contributing to gastroesophageal reflux
- Displacement of stomach and intestines by the enlarging uterus
- Increased water absorption in the colon, contributing to constipation
- Increased appetite as nausea typically subsides
- Gums may become more vascular and prone to bleeding
Urinary System
- Kidney size increases by approximately 1-1.5 cm
- Renal blood flow increases by 35-50%
- Glomerular filtration rate increases by 40-65%
- Physiologic hydronephrosis and hydroureter develop due to mechanical compression and hormonal effects
- Bladder capacity decreases as the uterus grows
- Increased frequency of urination, particularly as the uterus begins to compress the bladder
- Increased risk of urinary tract infections due to urinary stasis
Clinical Relevance
The increased GFR results in lower serum creatinine and blood urea nitrogen (BUN) levels during pregnancy. Values considered normal in non-pregnant women may indicate renal dysfunction in pregnant women.
Musculoskeletal System
- Relaxin, estrogen, and progesterone cause increased ligamentous laxity, particularly in the pelvic joints
- The symphysis pubis gap widens by approximately 3-8 mm
- Sacroiliac joint mobility increases
- Center of gravity shifts anteriorly as the uterus grows
- Lumbar lordosis often increases to compensate for the anterior shift in weight
- Abdominal muscles stretch to accommodate the enlarging uterus
- Separation of the rectus abdominis muscles (diastasis recti) may begin
Warning
Increased joint laxity and altered biomechanics predispose pregnant women to musculoskeletal discomfort, particularly in the lower back and pelvic girdle. Pelvic girdle pain affects approximately 20% of pregnant women and should be differentiated from other causes of back pain.
Integumentary System
- Increased melanocyte-stimulating hormone leads to hyperpigmentation of the skin
- Linea nigra develops – a dark vertical line extending from the pubic bone to the umbilicus
- Melasma (chloasma) may develop – brownish patches on the face, particularly on the forehead and cheeks
- Stretch marks (striae gravidarum) begin to appear on the abdomen, breasts, and thighs
- Increased sebaceous gland activity may lead to acne in some women
- Spider nevi and palmar erythema may develop due to increased estrogen
- Increased vascularity leads to skin warmth and occasional flushing
Endocrine System
- Placenta becomes the primary source of pregnancy hormones
- Estrogen levels continue to rise, promoting uterine growth and development
- Progesterone maintains the pregnancy and promotes smooth muscle relaxation
- Human chorionic gonadotropin (hCG) levels plateau and begin to decrease
- Human placental lactogen increases, promoting fetal growth and maternal metabolism
- Relaxin increases, promoting ligamentous laxity
- Mild insulin resistance develops, requiring increased insulin production
Clinical Relevance
The insulin resistance of pregnancy typically peaks in the late second to early third trimester. Women with risk factors for diabetes should be screened for gestational diabetes between weeks 24-28.
Neurological System
- Fluid retention and hormonal changes may lead to nerve compression syndromes
- Carpal tunnel syndrome may develop or worsen due to fluid retention
- Mood stabilization is common as first-trimester hormonal fluctuations decrease
- Altered sleep patterns due to physical discomforts and hormonal influences
- Heightened senses, particularly smell and taste
Common Discomforts and Management
The second trimester brings a unique set of discomforts related to the physiological changes occurring in the body. Nurses play a crucial role in educating pregnant individuals about these discomforts and providing evidence-based management strategies.
Back Pain
| Contributing Factors | Management Strategies |
|---|---|
|
|
Nursing Education Point
Differentiate between normal pregnancy-related back pain and pain that may indicate complications such as preterm labor or kidney infection. Red flags include pain associated with vaginal bleeding, fever, dysuria, or regular cramping.
Leg Cramps
| Contributing Factors | Management Strategies |
|---|---|
|
|
Heartburn and Indigestion
| Contributing Factors | Management Strategies |
|---|---|
|
|
Constipation
| Contributing Factors | Management Strategies |
|---|---|
|
|
Nasal Congestion and Nosebleeds
| Contributing Factors | Management Strategies |
|---|---|
|
|
Skin Changes
| Contributing Factors | Management Strategies |
|---|---|
|
|
Nursing Education Point
Educate patients that while there are many products marketed for preventing stretch marks, there is limited scientific evidence supporting their effectiveness. Genetic factors play a significant role in determining who will develop stretch marks.
Round Ligament Pain
| Contributing Factors | Management Strategies |
|---|---|
|
|
Warning
While round ligament pain is typically harmless, severe abdominal pain that is persistent or associated with fever, vaginal bleeding, or changes in vaginal discharge requires immediate medical evaluation to rule out complications such as placental abruption, preterm labor, or infection.
Varicose Veins
| Contributing Factors | Management Strategies |
|---|---|
|
|
Urinary Frequency
| Contributing Factors | Management Strategies |
|---|---|
|
|
Nursing Education Point
Educate pregnant individuals about the symptoms of urinary tract infections (painful urination, cloudy urine, fever) versus normal pregnancy-related urinary frequency. UTIs during pregnancy require prompt treatment to prevent complications.
Best Practices and Recent Updates in Second Trimester Care
Best Practice #1: Addressing Black Maternal Health Disparities
Recent studies continue to show that Black women are approximately three times more likely to die from pregnancy-related complications. In 2024, nursing organizations including the American Nurses Association (ANA) have called for passage of the Black Maternal Health Momnibus Act, which would fund community-based organizations working to advance maternal health equity and increase culturally congruent care.
Nursing Implications:
- Implement standardized screening tools to identify risk factors in all pregnant patients, with attention to social determinants of health
- Provide culturally sensitive care and education tailored to individual needs and backgrounds
- Connect patients with community resources that address specific barriers to care
- Monitor for signs of pregnancy complications with heightened vigilance in high-risk populations
- Advocate for diverse representation in maternal healthcare providers
Best Practice #2: Expanded Telehealth for Prenatal Care
The integration of telehealth services into prenatal care has accelerated, with studies showing effectiveness for certain aspects of second-trimester monitoring. Hybrid models combining virtual and in-person visits have demonstrated good outcomes while improving access to care, particularly in underserved areas.
Nursing Implications:
- Develop protocols for conducting effective virtual assessments during second trimester
- Train patients in home measurement of fundal height, blood pressure, and weight
- Identify clear criteria for when in-person evaluation is necessary
- Ensure proper documentation of telehealth encounters
- Provide technical support resources for patients with limited digital literacy
- Create contingency plans for technology failures during virtual visits
Best Practice #3: Mental Health Integration in Prenatal Care
Updated guidelines emphasize the importance of mental health screening and support throughout pregnancy, not just in the postpartum period. The second trimester is now recognized as an important time to address maternal mental health, as the physical stabilization during this period allows focus on psychological well-being.
Nursing Implications:
- Implement routine depression and anxiety screening at each second-trimester prenatal visit
- Develop clear referral pathways for patients requiring mental health support
- Provide education about normal emotional changes versus concerning symptoms during pregnancy
- Include partners/support persons in discussions about maternal mental health
- Normalize discussions about stress management and emotional well-being during pregnancy
- Connect patients with peer support groups specific to pregnancy
References
- American College of Obstetricians and Gynecologists. (2024). First and Second Stage Labor Management. Clinical Practice Guideline, Number 8. Retrieved from https://www.acog.org/clinical/clinical-guidance/clinical-practice-guideline
- Cleveland Clinic. (2024). Second Trimester of Pregnancy: What To Expect. Retrieved from https://my.clevelandclinic.org/health/articles/16092-pregnancy-second-trimester
- Mayo Clinic. (2025, February 7). 2nd trimester pregnancy: What to expect. Retrieved from https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy/art-20047732
- National Association of Nurse Practitioners in Women’s Health. (2024, August 26). Nursing Groups Unite to Address the Black Maternal Health Crisis. Retrieved from https://www.nursingworld.org/news/news-releases/2024/nursing-groups-unite-to-address-the-black-maternal-health-crisis-call-for-real-action-to-address-persistent-barriers-and-challenges-at-the-2024-black-maternal-health-summit/
- Physiopedia. (2022). Physiological Changes in Pregnancy. Retrieved from https://www.physio-pedia.com/Physiological_Changes_in_Pregnancy
- Tan, E.K., & Tan, E.L. (2013). Alterations in physiology and anatomy during pregnancy. Best Practice & Research, Clinical Obstetrics & Gynaecology, 27(6), 791-802.
- UNICEF. (2024). Your second trimester guide. Retrieved from https://www.unicef.org/parenting/pregnancy-milestones/second-trimester
- UCSF Health. (2024). Coping With Common Discomforts of Pregnancy. Retrieved from https://www.ucsfhealth.org/education/coping-with-common-discomforts-of-pregnancy
- OpenStax. (2024, June 26). Care in the Second Trimester of Pregnancy. Maternal-Newborn Nursing. Retrieved from https://openstax.org/books/maternal-newborn-nursing/pages/11-3-care-in-the-second-trimester-of-pregnancy
