Secondary Postpartum Hemorrhage
Comprehensive Clinical Guide for Nursing Students
Table of Contents
Introduction
Secondary postpartum hemorrhage (SPH) is an important obstetric complication that can occur days to weeks after delivery. Unlike primary postpartum hemorrhage, which occurs within the first 24 hours after delivery, SPH can manifest when the patient has already been discharged from the hospital, potentially leading to delayed diagnosis and treatment. As nursing professionals, understanding the pathophysiology, risk factors, clinical presentation, and management of SPH is crucial for providing timely and effective care to postpartum patients.
This comprehensive guide focuses on SPH from a nursing perspective, providing evidence-based information that will help nursing students develop the knowledge and skills needed to recognize, manage, and prevent this potentially life-threatening condition. The content includes detailed explanations, clinical pearls, mnemonics, and visual aids to facilitate learning and retention of key concepts.
Definition
Clinical Definition
Secondary postpartum hemorrhage (SPH) is defined as excessive vaginal bleeding occurring from 24 hours after delivery up to 12 weeks postpartum. It is also known as late postpartum hemorrhage or delayed postpartum hemorrhage.
The clinical significance of SPH lies in its potential to cause substantial maternal morbidity and, in severe cases, mortality. Unlike primary postpartum hemorrhage (PPH), which is typically managed in the hospital setting immediately after delivery, SPH often occurs after the patient has been discharged, necessitating readmission and sometimes causing delays in diagnosis and treatment.
Incidence
Secondary postpartum hemorrhage occurs in approximately 0.2% to 2% of all deliveries, making it less common than primary postpartum hemorrhage but still a significant clinical concern. SPH is one of the most common causes of readmission during the postpartum period. The wide range in reported incidence reflects variations in definition, diagnostic criteria, and reporting practices across different healthcare settings.
Pathophysiology
Understanding the pathophysiology of secondary postpartum hemorrhage requires knowledge of normal postpartum changes and how they can be disrupted. During the postpartum period, the placental site undergoes a process called involution, where the uterus returns to its pre-pregnant state. This process involves:
- Contraction of the myometrium to reduce the size of the uterus
- Compression of blood vessels at the placental site
- Formation of thrombi in the vessels of the placental bed
- Sloughing of the decidua and endometrial regeneration
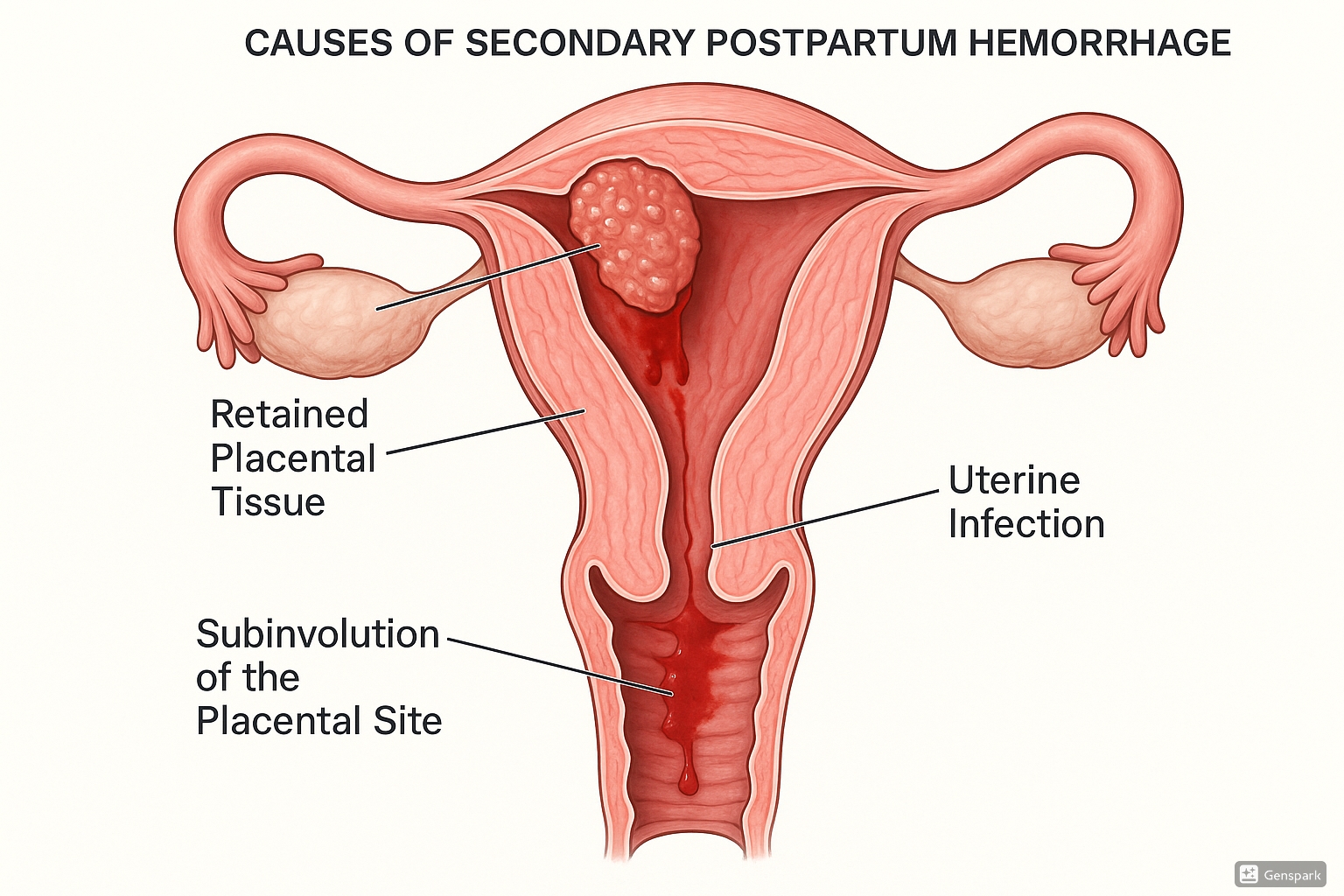
Secondary postpartum hemorrhage occurs when this normal process is disrupted. The bleeding occurs due to various mechanisms depending on the underlying cause:
Pathophysiological Mechanisms of SPH
- Subinvolution of the Placental Site: Failure of the uterus to return to its normal size and function, often due to impaired contraction of the myometrium at the placental site.
- Retained Placental Tissue: Fragments of placenta or membranes that remain in the uterus can prevent proper contraction and healing of the placental bed, leading to bleeding.
- Endometritis: Infection of the endometrium can disrupt the normal healing process and cause inflammation and bleeding.
- Pseudoaneurysm: Damage to a blood vessel during delivery can lead to the formation of a false aneurysm that may rupture days to weeks later.
- Coagulopathy: Disorders of blood clotting can predispose to delayed postpartum bleeding.
Causes and Risk Factors
Primary Causes
Mnemonic: “RETAINS”
Retained placental tissue
Endometritis
Trauma (unhealed)
Abnormal involution
Infection
Neovascularization issues
Subinvolution of placental site
The most common causes of secondary postpartum hemorrhage include:
| Cause | Frequency | Mechanism |
|---|---|---|
| Endometritis (Uterine Infection) | 40-60% | Infection of the endometrium causing inflammation and disruption of normal healing |
| Retained Placental Tissue | 20-40% | Fragments of placenta or membranes that prevent proper uterine contraction |
| Subinvolution of Placental Site | 10-20% | Failure of the placental site to heal properly with persistent vascularity |
| Vascular Abnormalities | 5-10% | Pseudoaneurysm, arteriovenous malformation, or other vascular anomalies |
| Wound Complications | 2-5% | Hematoma, infection, or dehiscence at cesarean or vaginal repair sites |
| Coagulation Disorders | 1-2% | Acquired or inherited disorders affecting blood clotting |
Risk Factors
Several factors increase the risk of developing secondary postpartum hemorrhage:
- Pre-delivery Factors:
- History of previous postpartum hemorrhage
- Multiparity (especially grand multiparity)
- Maternal age >35 years
- Pre-existing maternal anemia
- Placental abnormalities (placenta previa, placenta accreta)
- Intrapartum Factors:
- Cesarean delivery
- Prolonged labor
- Premature rupture of membranes
- Manual removal of the placenta
- Difficult or traumatic delivery
- Postpartum Factors:
- Primary postpartum hemorrhage
- Failure to receive prophylactic oxytocics
- Postpartum infection
- Lactation failure or suppression
Clinical Pearl
Always consider the possibility of retained placental tissue in patients who had a primary postpartum hemorrhage, as they are at higher risk for secondary hemorrhage. Similarly, patients who had manual removal of placenta are at increased risk for both infection and retention of placental fragments.
Signs and Symptoms
Patients with secondary postpartum hemorrhage typically present with the following clinical manifestations:
Primary Presentations
- Excessive Vaginal Bleeding: More than expected lochia, which may be sudden or gradual in onset
- Passing Blood Clots: Especially large clots or persistent passage of clots
- Foul-smelling Lochia: Suggesting infection (endometritis)
- Lower Abdominal Pain or Cramping: Often described as more severe than normal afterpains
Associated Symptoms
- Fever: Temperature >38°C (100.4°F), especially with endometritis
- Tachycardia: Heart rate >100 beats per minute
- Hypotension: In cases of significant blood loss
- Uterine Tenderness: On abdominal examination
- General Malaise: Fatigue, weakness, or feeling unwell
- Symptoms of Anemia: Dizziness, lightheadedness, fatigue, pallor
Warning Signs Requiring Immediate Attention
The following symptoms require immediate medical evaluation:
- Sudden heavy bleeding that soaks through a pad in less than an hour
- Passing clots larger than a golf ball
- Severe abdominal pain not relieved by analgesics
- Fever >38°C (100.4°F) with chills
- Dizziness, fainting, or confusion
- Tachycardia or hypotension
Diagnosis
The diagnosis of secondary postpartum hemorrhage involves a comprehensive approach including clinical history, physical examination, laboratory tests, and imaging studies.
Clinical History
A detailed history should include:
- Onset, duration, and quantity of bleeding
- Associated symptoms (pain, fever, malaise)
- Details of delivery (mode of delivery, complications)
- Past obstetric history
- Medical history and current medications
- Risk factors for postpartum hemorrhage
Physical Examination
Physical examination should focus on:
- Vital Signs: Blood pressure, heart rate, temperature, respiratory rate
- General Appearance: Assessment for signs of hypovolemia or shock
- Abdominal Examination: Uterine size, tenderness, presence of masses
- Pelvic Examination: Speculum examination to assess the amount and character of bleeding, examination of the cervix for lacerations or hematomas, and bimanual examination to assess uterine size and tenderness
Laboratory Studies
Essential laboratory tests include:
- Complete Blood Count (CBC): To assess hemoglobin, hematocrit, and white blood cell count
- Coagulation Profile: Including prothrombin time (PT), partial thromboplastin time (PTT), and fibrinogen level
- Blood Type and Screen: In preparation for possible blood transfusion
- Inflammatory Markers: C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) in suspected infection
- Microbiology: Blood cultures and endometrial cultures in cases of suspected endometritis
Imaging Studies
Imaging studies can help identify the cause of secondary postpartum hemorrhage:
| Imaging Modality | Findings | Advantages | Limitations |
|---|---|---|---|
| Transvaginal Ultrasound | Retained products of conception appear as heterogeneous echogenic mass within the endometrial cavity | Non-invasive, readily available, no radiation exposure | Operator-dependent, may not detect small fragments |
| Color Doppler Ultrasound | Enhanced vascularity at the placental site in subinvolution; pseudoaneurysm appears as pulsatile anechoic area with turbulent flow | Can identify vascular causes of bleeding | Requires experienced sonographer |
| CT Angiography | Identifies vascular anomalies, arteriovenous malformations, or pseudoaneurysms | Detailed vascular imaging | Radiation exposure, contrast risks |
| MRI | Superior soft tissue detail, can differentiate between retained products and blood clots | No radiation, excellent tissue characterization | Limited availability, time-consuming |
Clinical Pearl
Transvaginal ultrasound is the first-line imaging modality for suspected secondary postpartum hemorrhage. The sensitivity of ultrasound for detecting retained placental tissue ranges from 80-90%, but its specificity is lower (around 60-70%) as it may be difficult to differentiate between retained tissue and blood clots.
Management
The management of secondary postpartum hemorrhage follows a systematic approach based on the patient’s clinical status and the underlying cause.
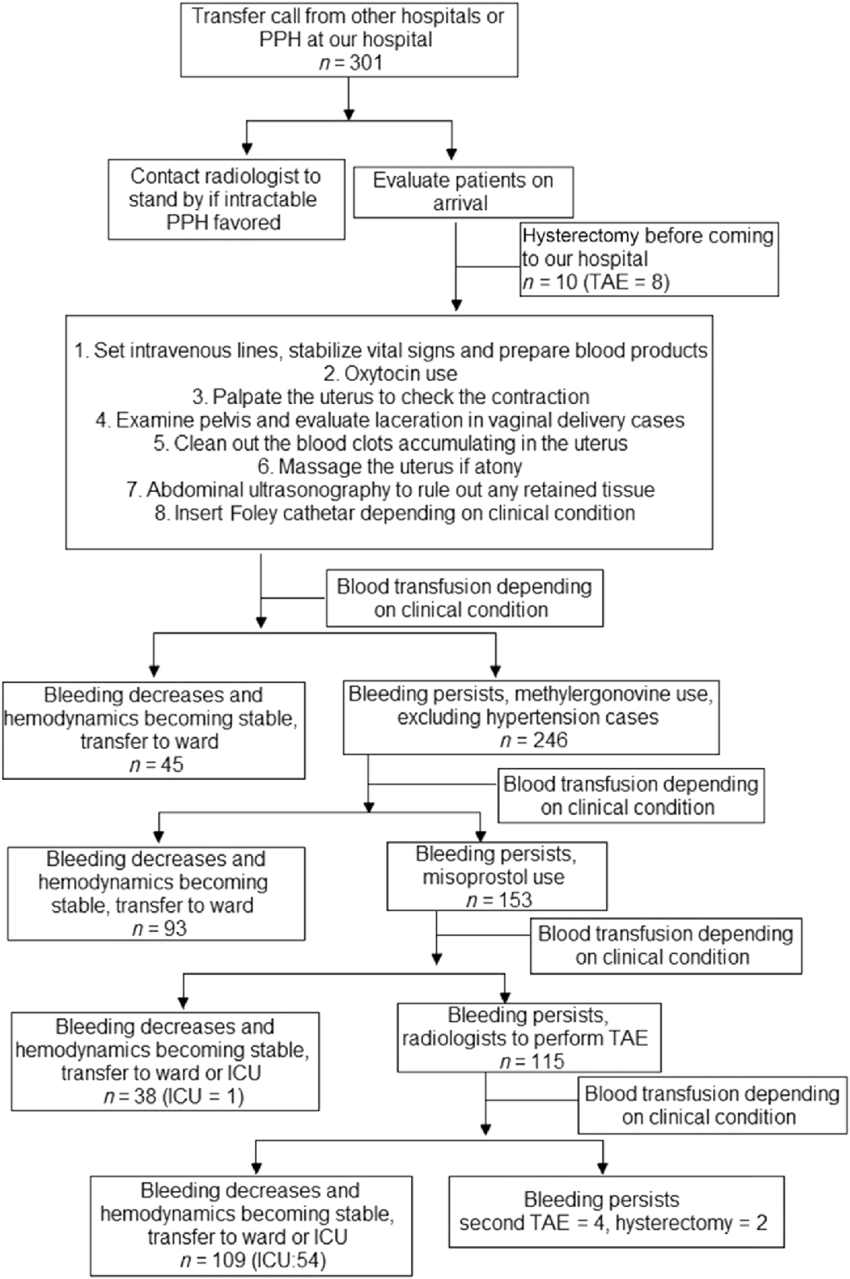
Initial Management
The initial approach to secondary postpartum hemorrhage focuses on resuscitation and stabilization:
Mnemonic: “ABCDE-H” for Initial Management
Airway – Ensure patent airway
Breathing – Provide oxygen if needed
Circulation – Establish IV access, fluid resuscitation
Drugs – Administer uterotonics, antibiotics if indicated
Examine – Complete physical examination
Hemoglobin – Monitor blood loss and replace as needed
- Resuscitation: Following standard ABCDE approach
- Establish large-bore IV access (at least two 16-18G cannulas)
- Fluid resuscitation with crystalloids
- Oxygen therapy if needed
- Blood product transfusion based on clinical status and laboratory parameters
- Assessment: Evaluate the severity of bleeding and hemodynamic stability
- Monitoring: Continuous vital signs, urine output, and blood loss
- Laboratory Testing: As outlined in the diagnostic section
- Identification of Cause: Clinical assessment and appropriate imaging
Medical Management
Medical therapy is often the first-line treatment for secondary postpartum hemorrhage:
| Medication | Dosage and Route | Mechanism of Action | Contraindications/Side Effects |
|---|---|---|---|
| Oxytocin (Pitocin) | 10-40 units in 1 L of IV fluid at 125 mL/hr | Stimulates uterine contractions | Hypotension, water intoxication with prolonged use |
| Methylergonovine (Methergine) | 0.2 mg IM every 2-4 hours (max 5 doses) | Causes sustained uterine contractions | Contraindicated in hypertension, preeclampsia; side effects: hypertension, nausea |
| Misoprostol (Cytotec) | 800-1000 mcg rectally once | Prostaglandin E1 analog causing uterine contractions | Fever, shivering, diarrhea |
| Carboprost (Hemabate) | 250 mcg IM every 15-90 min (max 8 doses) | Prostaglandin F2α causing uterine contractions | Contraindicated in asthma; side effects: nausea, vomiting, diarrhea, bronchospasm |
| Tranexamic Acid | 1 g IV over 10 minutes, repeat after 30 min if needed | Antifibrinolytic that inhibits clot breakdown | Contraindicated in active thromboembolic disorder; side effects: nausea, vomiting, hypotension |
| Antibiotics | Broad-spectrum coverage (e.g., ampicillin + gentamicin + metronidazole or clindamycin + gentamicin) | Treats underlying endometritis | Allergic reactions, antibiotic-associated diarrhea |
Clinical Pearl
The combination of uterotonics and antibiotics is often recommended as first-line treatment for secondary PPH, especially when endometritis is suspected. The commonly used antibiotic regimen includes ampicillin (or clindamycin if penicillin-allergic) plus metronidazole, with gentamicin added for cases of endomyometritis or sepsis.
Surgical Management
Surgical intervention may be necessary when medical management fails or specific conditions are identified:
- Dilation and Curettage (D&C): For removal of retained placental tissue
- May be performed under ultrasound guidance to improve safety and efficacy
- Risk of perforation, especially with infection or delayed postpartum status
- Hysteroscopy: For direct visualization and removal of retained tissue
- Allows targeted removal with reduced trauma to the endometrium
- May be combined with ultrasound guidance
