Serological Tests and Immunization
Comprehensive Nursing Study Notes
Comprehensive overview of immune system components, serological testing, and vaccination protocols
Table of Contents
1. Introduction to Serological Tests
Key Concept: Serology
Serology is the scientific study of serum and other bodily fluids, focusing on the detection and measurement of antibodies, antigens, and other immune components. In clinical practice, serological tests are essential diagnostic tools that help identify infections, immune status, and autoimmune conditions.
Memory Aid: SERUM
- Specific antibody detection
- Evaluation of immune response
- Rapid diagnostic results
- Understanding disease progression
- Monitoring treatment effectiveness
Clinical Applications
Diagnostic Uses:
- Infectious disease identification
- Autoimmune disorder detection
- Allergy testing
- Blood typing and cross-matching
- Pregnancy testing
Monitoring Uses:
- Vaccine effectiveness
- Disease progression
- Treatment response
- Immune system function
- Organ transplant rejection
Historical Context: Serological testing has been a cornerstone of medical diagnosis since the early 1900s. The development of enzyme-linked immunosorbent assay (ELISA) in the 1970s revolutionized the field, making serological tests more sensitive, specific, and widely accessible.
2. Immunoglobulins: Structure, Types & Properties
Immunoglobulin Structure
Basic Y-Shaped Antibody Structure
Fab (Antigen-binding)
/ \
Light Chain Heavy Chain
\ /
\ /
\ /
\ /
\/
Fc (Crystallizable)
(Effector Function)
Structural Components
Heavy Chains:
- Determine antibody class (isotype)
- Constant and variable regions
- Molecular weight: ~50-70 kDa
- Types: γ, α, μ, δ, ε
Light Chains:
- Two types: Kappa (κ) and Lambda (λ)
- Molecular weight: ~25 kDa
- Constant and variable regions
- Ratio κ:λ = 2:1 in humans
Memory Aid: GAMES (Immunoglobulin Classes)
- Gammaglobulin (IgG) – Most abundant, crosses placenta
- Antigens at mucosal surfaces (IgA) – Secretory antibody
- Macroglobulin (IgM) – First responder, largest antibody
- Eosinophils and allergies (IgE) – Allergic reactions
- Surface bound (IgD) – B-cell receptor
| Immunoglobulin | Molecular Weight | Concentration | Half-life | Primary Function |
|---|---|---|---|---|
| IgG | 150 kDa | 8-16 mg/mL | 21 days | Secondary immune response, placental transfer |
| IgA | 160-380 kDa | 1-4 mg/mL | 6 days | Mucosal immunity, secretory antibody |
| IgM | 900 kDa | 0.5-2 mg/mL | 5 days | Primary immune response, complement activation |
| IgE | 190 kDa | 0.05-0.3 mg/mL | 2 days | Allergic reactions, parasite immunity |
| IgD | 180 kDa | 0.03-0.4 mg/mL | 3 days | B-cell receptor, antigen recognition |
Functional Properties
Binding Properties:
- Antigen specificity
- Binding affinity
- Avidity (overall binding strength)
- Cross-reactivity potential
Effector Functions:
- Complement activation
- Opsonization
- Antibody-dependent cell cytotoxicity
- Neutralization
Distribution:
- Tissue distribution
- Serum concentration
- Secretory presence
- Cellular binding
3. Principles of Serological Testing
Antigen-Antibody Interactions
Serological tests are based on the specific binding between antigens and antibodies. This interaction is governed by molecular recognition, where the antibody’s binding site (paratope) recognizes and binds to the antigen’s epitope with high specificity and affinity.
Serological Test Workflow
Test Interpretation Principles
Qualitative Results:
- Positive: Presence of target analyte
- Negative: Absence of target analyte
- Indeterminate: Unclear results
- Invalid: Test failure
Quantitative Results:
- Titers: Highest dilution showing positivity
- Concentration: Absolute amount present
- Index values: Ratio to reference standard
- Units: Standardized measurement units
Memory Aid: ELISA Steps (WASH)
- Well coating with antigen or antibody
- Add sample and incubate
- Secondary antibody addition
- Horseradish peroxidase detection
Clinical Significance: Understanding serological principles helps nurses interpret test results accurately, recognize limitations, and provide appropriate patient education. False positives and negatives can occur, requiring clinical correlation.
4. Common Serological Tests
Infectious Disease Serology
| Test | Pathogen | Markers | Clinical Significance | Nursing Considerations |
|---|---|---|---|---|
| Hepatitis B | HBV | HBsAg, HBsAb, HBcAb | Acute/chronic infection, immunity | Occupational exposure protocol |
| HIV | HIV-1/2 | HIV Ab, HIV Ag/Ab | HIV infection status | Counseling, confidentiality |
| Syphilis | T. pallidum | RPR, VDRL, FTA-ABS | Syphilis screening/confirmation | Partner notification, treatment |
| COVID-19 | SARS-CoV-2 | IgM, IgG antibodies | Past infection, immunity | Vaccination status correlation |
| Rubella | Rubella virus | IgM, IgG antibodies | Immunity status, recent infection | Pregnancy screening importance |
Autoimmune Disease Serology
Rheumatoid Arthritis:
- Rheumatoid Factor (RF)
- Anti-CCP antibodies
- Diagnostic and prognostic value
- Monitor disease activity
Systemic Lupus Erythematosus:
- Antinuclear Antibodies (ANA)
- Anti-dsDNA antibodies
- Complement levels (C3, C4)
- Disease activity correlation
Nursing Procedure: Serum Collection
- Verify patient identity and test orders
- Explain procedure to patient
- Collect 5-10 mL venous blood in appropriate tube
- Allow clotting at room temperature (30-60 minutes)
- Centrifuge to separate serum
- Label specimen with patient information
- Store/transport according to test requirements
- Document collection time and conditions
Critical Alert: Hemolysis Effects
Hemolyzed samples can significantly affect serological test results. Ensure proper collection technique, avoid excessive agitation, and use appropriate needle size to prevent hemolysis.
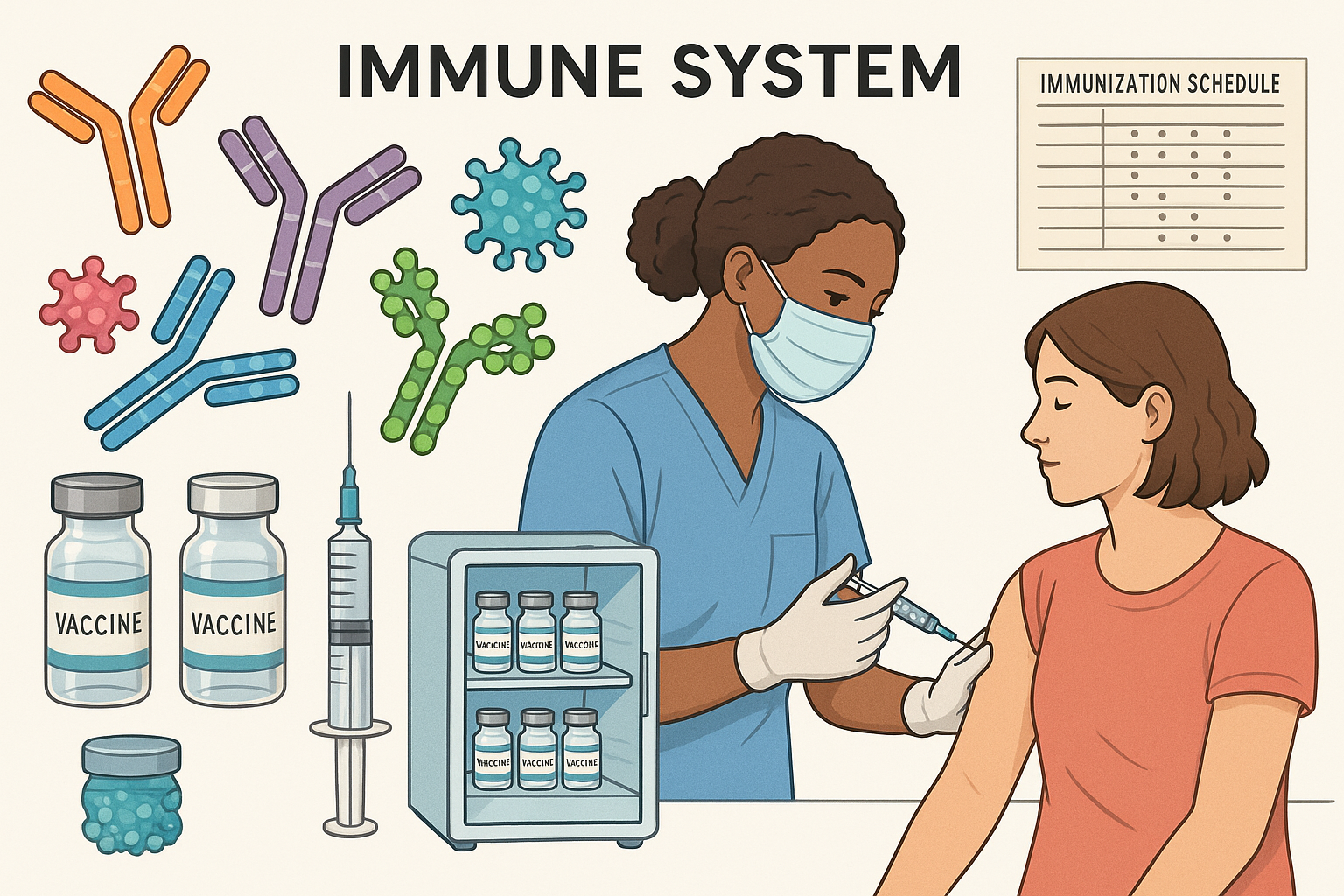
5. Vaccines: Types & Classification
Vaccine Fundamentals
Vaccines are biological preparations that provide active acquired immunity against specific diseases. They contain antigens that stimulate the immune system to recognize and remember pathogens, providing protection against future infections.
Memory Aid: LIVE (Vaccine Types)
- Live attenuated vaccines
- Inactivated vaccines
- Viral vector vaccines
- Engineered vaccines (subunit, toxoid)
Vaccine Classification
Live Attenuated Vaccines
Contain weakened but living pathogens that replicate in the host.
Examples:
- MMR (Measles, Mumps, Rubella)
- Varicella (Chickenpox)
- Oral Polio Vaccine (OPV)
- Yellow Fever
Advantages:
- Strong, long-lasting immunity
- Cellular and humoral response
- Often single dose sufficient
- Cost-effective production
Disadvantages:
- Risk of reversion to virulence
- Contraindicated in immunocompromised
- Storage requirements
- Potential for adverse reactions
Inactivated Vaccines
Contain killed pathogens that cannot replicate.
Examples:
- Influenza vaccine
- Hepatitis A
- Inactivated Polio Vaccine (IPV)
- Rabies vaccine
Advantages:
- Cannot cause disease
- Safe for immunocompromised
- Stable storage
- No risk of reversion
Disadvantages:
- Weaker immune response
- Multiple doses required
- Boosters needed
- Primarily humoral immunity
Subunit Vaccines
Contain purified antigens or antigen fragments.
Examples:
- Hepatitis B (HBsAg)
- Pertussis (acellular)
- Pneumococcal polysaccharide
- HPV vaccine
Characteristics:
- Highly purified antigens
- Reduced side effects
- Adjuvants often needed
- Specific immune targeting
Toxoid Vaccines
Contain inactivated toxins that cause disease symptoms.
Examples:
- Diphtheria toxoid
- Tetanus toxoid
- Combined DT, Td, Tdap
Characteristics:
- Prevent toxin-mediated disease
- High safety profile
- Require boosters
- Aluminum adjuvants used
Vaccine Administration Considerations
Timing:
- Age-appropriate scheduling
- Interval between doses
- Catch-up schedules
- Simultaneous administration
Route & Site:
- Intramuscular (most common)
- Subcutaneous
- Oral (specific vaccines)
- Intranasal (FluMist)
Documentation:
- Vaccine name and manufacturer
- Lot number and expiration
- Date and site of administration
- Adverse events
Contraindications & Precautions
Absolute Contraindications:
- Severe immunodeficiency (live vaccines)
- Severe allergic reaction to vaccine component
- Pregnancy (live vaccines)
- Severe illness with fever
Precautions:
- Moderate illness
- Recent blood product administration
- Thrombocytopenia
- Altered immunocompetence
6. Vaccine Storage & Handling
Critical Importance
Proper vaccine storage and handling is essential for maintaining vaccine potency and effectiveness. Temperature excursions can result in reduced immunogenicity and vaccine failure, compromising patient protection.
Temperature Requirements
| Vaccine Type | Storage Temperature | Freezer Sensitivity | Special Considerations |
|---|---|---|---|
| Most Vaccines | 2°C to 8°C (36°F to 46°F) | Do not freeze | Refrigerator storage |
| Varicella | -15°C or colder | Frozen storage required | Freezer compartment |
| Zoster | -15°C or colder | Frozen storage required | Freezer compartment |
| Reconstituted | Use immediately | Varies by vaccine | Discard after specified time |
Storage Equipment Requirements
Refrigerator Specifications:
- Purpose-built or pharmaceutical-grade
- Separate from food/beverage storage
- Adequate capacity for vaccine inventory
- Temperature monitoring system
- Backup power supply recommended
Monitoring Requirements:
- Digital data logger (DDL)
- Continuous temperature monitoring
- Alarm system for excursions
- Daily temperature recording
- Calibration verification
Vaccine Transport Protocol
- Pre-condition transport container
- Pack vaccines with appropriate coolant
- Include temperature monitoring device
- Seal container and label with contents
- Transport quickly to destination
- Verify temperature upon arrival
- Document transport conditions
- Store vaccines immediately upon receipt
Memory Aid: STORE (Storage Best Practices)
- Store in center of refrigerator
- Temperature monitor continuously
- Organize by expiration date
- Rotate stock (first in, first out)
- Emergency procedures in place
Emergency Procedures
When temperature excursions occur:
- Do not discard vaccines immediately
- Isolate affected vaccines
- Document time and temperature range
- Contact vaccine manufacturer or immunization program
- Await guidance before discarding
- Complete incident report
7. Cold Chain Management
Cold Chain Definition
The cold chain is the temperature-controlled supply chain that maintains vaccine potency from manufacture to administration. It includes all people, equipment, and processes involved in storing, handling, and transporting vaccines.
Cold Chain Components
Quality Assurance Elements
Personnel Training:
- Storage requirements knowledge
- Handling procedures
- Emergency protocols
- Documentation requirements
Equipment Maintenance:
- Regular calibration
- Preventive maintenance
- Backup systems
- Alarm functionality
Monitoring Systems:
- Continuous temperature logging
- Real-time alerts
- Data analysis
- Corrective action protocols
Roles and Responsibilities
| Role | Primary Responsibilities | Key Skills Required |
|---|---|---|
| Vaccine Coordinator | Overall vaccine management, staff training, policy development | Leadership, immunization expertise, quality management |
| Primary Handler | Daily vaccine handling, temperature monitoring, inventory management | Attention to detail, reliability, problem-solving |
| Backup Handler | Coverage during absences, emergency response | Same skills as primary handler |
| Administering Nurse | Patient assessment, vaccine administration, documentation | Clinical skills, patient communication, safety protocols |
Global Perspective: Cold chain management is particularly challenging in resource-limited settings. Solar-powered refrigerators, vaccine vial monitors, and innovative delivery systems are improving vaccine accessibility worldwide.
8. Immunization for Various Diseases
Childhood Immunizations
| Disease | Vaccine | Schedule | Route | Complications Prevented |
|---|---|---|---|---|
| Diphtheria | DTaP, Tdap | 2, 4, 6, 15-18 months, 4-6 years | IM | Respiratory obstruction, myocarditis |
| Tetanus | DTaP, Tdap | Same as diphtheria | IM | Muscle spasms, respiratory failure |
| Pertussis | DTaP, Tdap | Same as diphtheria | IM | Whooping cough, pneumonia |
| Polio | IPV | 2, 4, 6-18 months, 4-6 years | IM/SQ | Paralytic poliomyelitis |
| Measles | MMR | 12-15 months, 4-6 years | SQ | Encephalitis, pneumonia |
| Mumps | MMR | Same as measles | SQ | Orchitis, meningitis |
| Rubella | MMR | Same as measles | SQ | Congenital rubella syndrome |
| Varicella | Var | 12-15 months, 4-6 years | SQ | Severe chickenpox, shingles |
Adult Immunizations
Ages 19-64 Years
- Influenza (annually)
- Td/Tdap (every 10 years)
- MMR (if no evidence of immunity)
- Varicella (if no evidence of immunity)
- HPV (through age 26)
- Meningococcal (high-risk groups)
Ages 65+ Years
- Influenza (annually, high-dose)
- Pneumococcal (PCV13, PPSV23)
- Zoster (Shingrix, 2 doses)
- Td/Tdap (every 10 years)
- COVID-19 (per current guidelines)
Special Populations
Pregnancy:
- Influenza vaccine (any trimester)
- Tdap (27-36 weeks)
- Avoid live vaccines
- COVID-19 vaccine recommended
Immunocompromised:
- Avoid live vaccines
- Additional doses may be needed
- Pneumococcal vaccines
- Close household contacts vaccinated
Healthcare Workers:
- Influenza (annual requirement)
- Hepatitis B series
- MMR (if no immunity)
- Varicella (if no immunity)
Memory Aid: VACCINES (Adult Immunizations)
- Varicella (if no immunity)
- Annual influenza
- COVID-19 (per guidelines)
- Cervical cancer prevention (HPV)
- Immunity to MMR
- Needs Td/Tdap every 10 years
- Elderly need pneumococcal
- Shingles prevention (Zoster)
9. Immunization Schedule
Schedule Importance
Immunization schedules are carefully designed to provide optimal protection at the earliest safe age. They consider maternal antibody interference, immune system development, disease risk, and vaccine safety profiles.
Routine Childhood Immunization Schedule (0-18 years)
| Age | Vaccines Due | Notes |
|---|---|---|
| Birth | Hepatitis B #1 | Within 24 hours of birth |
| 2 months | DTaP #1, IPV #1, Hib #1, PCV13 #1, RV #1, Hep B #2 | First major immunization visit |
| 4 months | DTaP #2, IPV #2, Hib #2, PCV13 #2, RV #2 | Second series doses |
| 6 months | DTaP #3, IPV #3, Hib #3, PCV13 #3, RV #3, Hep B #3 | Completion of primary series |
| 12-15 months | MMR #1, Varicella #1, Hib #4, PCV13 #4 | Live vaccines introduction |
| 15-18 months | DTaP #4 | Booster dose |
| 4-6 years | DTaP #5, IPV #4, MMR #2, Varicella #2 | School entry requirements |
| 11-12 years | Tdap, HPV series, Meningococcal | Adolescent platform |
| 16-18 years | Meningococcal booster | College preparation |
Memory Aid: 2-4-6 Rule
Most routine vaccines follow the 2-4-6 month schedule for primary series:
- 2 months: First dose of DTaP, IPV, Hib, PCV13, RV
- 4 months: Second dose of same vaccines
- 6 months: Third dose of same vaccines
- 12-15 months: Boosters and new vaccines (MMR, Varicella)
Catch-up Immunization
Principles:
- Age-appropriate vaccines only
- Minimum intervals between doses
- No need to restart series
- Accelerated schedule if needed
Documentation:
- Previous vaccination history
- Catch-up schedule plan
- Reason for delayed vaccination
- Patient/parent counseling
Nursing Assessment Before Immunization
- Review immunization history and records
- Assess current health status
- Screen for contraindications and precautions
- Identify risk factors for adverse events
- Verify vaccine storage and expiration
- Obtain informed consent
- Prepare emergency equipment
- Plan observation period
Cultural Considerations: Respect cultural beliefs while providing evidence-based education. Address vaccine hesitancy with empathy, accurate information, and culturally appropriate communication strategies.
10. Nursing Implementation
Comprehensive Nursing Care
Nurses play a crucial role in immunization programs, from patient assessment and education to vaccine administration and follow-up care. This section outlines key nursing responsibilities and best practices.
Pre-Immunization Assessment
Comprehensive Health Assessment
Health History:
- Previous immunizations and reactions
- Allergies (especially to vaccine components)
- Current medications and treatments
- Immunocompromising conditions
- Recent illness or fever
- Pregnancy status (if applicable)
Physical Assessment:
- Vital signs (especially temperature)
- General appearance and wellness
- Injection site examination
- Lymph node assessment
- Respiratory status
- Skin condition
Patient & Family Education
Pre-Vaccination:
- Explain vaccine purpose and benefits
- Discuss potential side effects
- Address concerns and questions
- Review consent process
- Provide written information
Post-Vaccination:
- Normal reactions to expect
- When to seek medical care
- Pain management strategies
- Activity restrictions
- Follow-up appointments
Documentation:
- Vaccination record cards
- Electronic health records
- Immunization registries
- School/employer forms
- Travel documentation
Vaccine Administration Technique
- Preparation: Verify patient identity, vaccine type, and dose
- Hand hygiene: Perform thorough hand washing
- Equipment: Gather appropriate needles and syringes
- Vaccine preparation: Follow manufacturer instructions
- Site selection: Choose appropriate injection site
- Positioning: Ensure patient comfort and accessibility
- Injection: Use proper technique for route specified
- Disposal: Safely dispose of sharps and materials
- Documentation: Record all required information
- Observation: Monitor for immediate reactions
Memory Aid: INJECT (Administration Steps)
- Identify patient and verify orders
- Needle and syringe selection
- Justify site selection
- Explain procedure to patient
- Clean injection site
- Technique: proper injection method
| Age Group | Preferred Site | Needle Size | Maximum Volume | Special Considerations |
|---|---|---|---|---|
| Infants (0-12 months) | Vastus lateralis | 22-25G, 5/8″-1″ | 1 mL | Thigh muscle preferred |
| Toddlers (1-3 years) | Vastus lateralis or deltoid | 22-25G, 5/8″-1″ | 1 mL | Deltoid if adequate muscle |
| Children (3-18 years) | Deltoid | 22-25G, 5/8″-1″ | 1 mL | Adjust needle length |
| Adults (19+ years) | Deltoid | 22-25G, 1″-1.5″ | 1 mL | Consider body habitus |
Emergency Management: Anaphylaxis
Recognition Signs:
- Sudden onset (minutes to hours)
- Skin: urticaria, angioedema
- Respiratory: wheezing, stridor
- Cardiovascular: hypotension, tachycardia
- Gastrointestinal: nausea, vomiting
- Neurologic: confusion, loss of consciousness
Immediate Actions:
- Call emergency services (911)
- Position patient supine
- Administer epinephrine IM
- Maintain airway and breathing
- Monitor vital signs
- Prepare for transport
Adverse Event Reporting
Report serious adverse events to VAERS (Vaccine Adverse Event Reporting System):
- Any event listed in VAERS Table of Reportable Events
- Hospitalization or prolonged hospitalization
- Life-threatening illness
- Disability or permanent damage
- Death
- Any event that requires medical intervention
Documentation Requirements
Required Information:
- Patient name and date of birth
- Vaccine name and manufacturer
- Lot number and expiration date
- Date and time of administration
- Injection site and route
- Healthcare provider information
Legal Requirements:
- Informed consent documentation
- VIS (Vaccine Information Statement) provision
- Screening checklist completion
- Adverse event documentation
- Registry reporting
Legal and Ethical Considerations
Informed Consent:
- Explain benefits and risks
- Provide opportunity for questions
- Respect patient autonomy
- Document consent process
Scope of Practice:
- Follow state nursing regulations
- Maintain competency
- Collaborate with providers
- Recognize limitations
Confidentiality:
- Protect patient privacy
- Secure records storage
- Authorized disclosure only
- HIPAA compliance
11. Clinical Applications
Evidence-Based Practice Integration
Integrating serological testing and immunization practices requires understanding current evidence, clinical guidelines, and best practices. This section provides practical applications for nursing practice.
Serological Test Interpretation
Common Serological Patterns
| Test Pattern | IgM Result | IgG Result | Clinical Interpretation | Nursing Action |
|---|---|---|---|---|
| Acute Infection | Positive | Negative/Low | Recent infection, early immune response | Isolation precautions, monitor symptoms |
| Past Infection | Negative | Positive | Previous infection, immunity present | Patient education about immunity |
| Active Infection | Positive | Positive | Ongoing infection, immune response | Treatment monitoring, symptom management |
| Vaccination | Negative | Positive | Vaccine-induced immunity | Confirm vaccination history |
| Susceptible | Negative | Negative | No immunity, susceptible to infection | Vaccination recommendation |
Case Study Applications
Case 1: Pregnancy Screening
Scenario: 28-year-old pregnant woman, first prenatal visit
Serological Tests: Rubella IgG negative, Hepatitis B surface antigen negative
Nursing Actions:
- Counsel about rubella susceptibility
- Plan postpartum MMR vaccination
- Avoid live vaccines during pregnancy
- Provide written education materials
Case 2: Occupational Exposure
Scenario: Healthcare worker with needlestick injury
Serological Tests: Hepatitis B surface antibody positive, HIV negative
Nursing Actions:
- Confirm hepatitis B immunity
- Assess source patient risk factors
- Follow institutional exposure protocol
- Schedule follow-up testing
Quality Improvement Initiatives
Vaccination Rates:
- Monitor coverage rates
- Identify barriers to vaccination
- Implement reminder systems
- Track missed opportunities
Storage Compliance:
- Temperature monitoring audits
- Staff training assessments
- Equipment maintenance logs
- Emergency response drills
Safety Monitoring:
- Adverse event tracking
- Error reporting systems
- Patient satisfaction surveys
- Continuous education programs
Memory Aid: ASSESS (Clinical Decision Making)
- Analyze test results in clinical context
- Screen for contraindications
- Select appropriate interventions
- Educate patient and family
- Schedule follow-up as needed
- Support patient decision-making
Technology Integration: Electronic health records, immunization registries, and clinical decision support systems are increasingly important tools for optimizing serological testing and vaccination practices.
12. Conclusion & Key Takeaways
Essential Competencies
Mastery of serological testing and immunization practices is fundamental to nursing practice. These competencies enable nurses to provide safe, effective care while supporting public health initiatives.
Core Learning Objectives Achieved
Knowledge Base:
- Immunoglobulin structure and function
- Serological test principles and interpretation
- Vaccine types and mechanisms
- Immunization schedules and guidelines
- Storage and handling requirements
Clinical Skills:
- Patient assessment and screening
- Vaccine administration techniques
- Emergency response protocols
- Documentation and reporting
- Patient education and counseling
Final Memory Aid: IMMUNE (Nursing Excellence)
- Interpret test results accurately
- Maintain vaccine integrity
- Monitor for adverse events
- Understand immunology principles
- Navigate ethical considerations
- Educate patients effectively
Future Directions
Emerging Technologies:
- Point-of-care testing
- Digital immunization records
- AI-assisted diagnostics
- Telemedicine integration
Vaccine Development:
- mRNA vaccine platforms
- Universal influenza vaccines
- Cancer immunotherapy
- Personalized vaccines
Public Health:
- Global vaccination initiatives
- Vaccine equity programs
- Outbreak response systems
- Community engagement strategies
Professional Development
Continuing education and professional growth in immunization practice:
- Immunization certification programs
- Professional organization membership
- Continuing education requirements
- Evidence-based practice integration
- Leadership in immunization programs
Impact on Patient Outcomes
Effective nursing practice in serology and immunization contributes to:
Individual Benefits:
- Disease prevention and health promotion
- Reduced healthcare costs
- Improved quality of life
- Enhanced patient safety
Population Health:
- Herd immunity protection
- Outbreak prevention
- Health equity promotion
- Global health security
Excellence in Nursing Practice
Comprehensive understanding of serological testing and immunization practices enhances nursing competency and improves patient outcomes through evidence-based care.
© 2025 Nursing Education Resources • Evidence-Based Practice • Patient-Centered Care