Modern Approaches to Child Health: Shifting Trends in Preventive, Promotive & Curative Care
Comprehensive guide for nursing students on the evolution of pediatric healthcare
Introduction
Child healthcare is experiencing a paradigm shift from a predominantly curative approach to a more balanced model that integrates preventive, promotive, and curative elements. This shift recognizes that optimal child health requires not just treating illnesses but preventing them and actively promoting positive health behaviors and environments.
Modern child healthcare is built upon three interconnected pillars that work together to ensure optimal health outcomes:
- Preventive Care: Focuses on preventing diseases, injuries, and other health problems before they occur through immunizations, screenings, and anticipatory guidance.
- Promotive Care: Actively enhances well-being by fostering positive health behaviors, supportive environments, and policies that enable children to thrive.
- Curative Care: Addresses existing health conditions through diagnosis, treatment, and management to restore health and prevent complications.
The integration of these three approaches represents a comprehensive strategy to address the complex and evolving healthcare needs of children in the 21st century. This shifting trend acknowledges that children’s health is influenced by multiple factors, including biological, behavioral, environmental, and social determinants.
The Shifting Paradigm in Child Healthcare
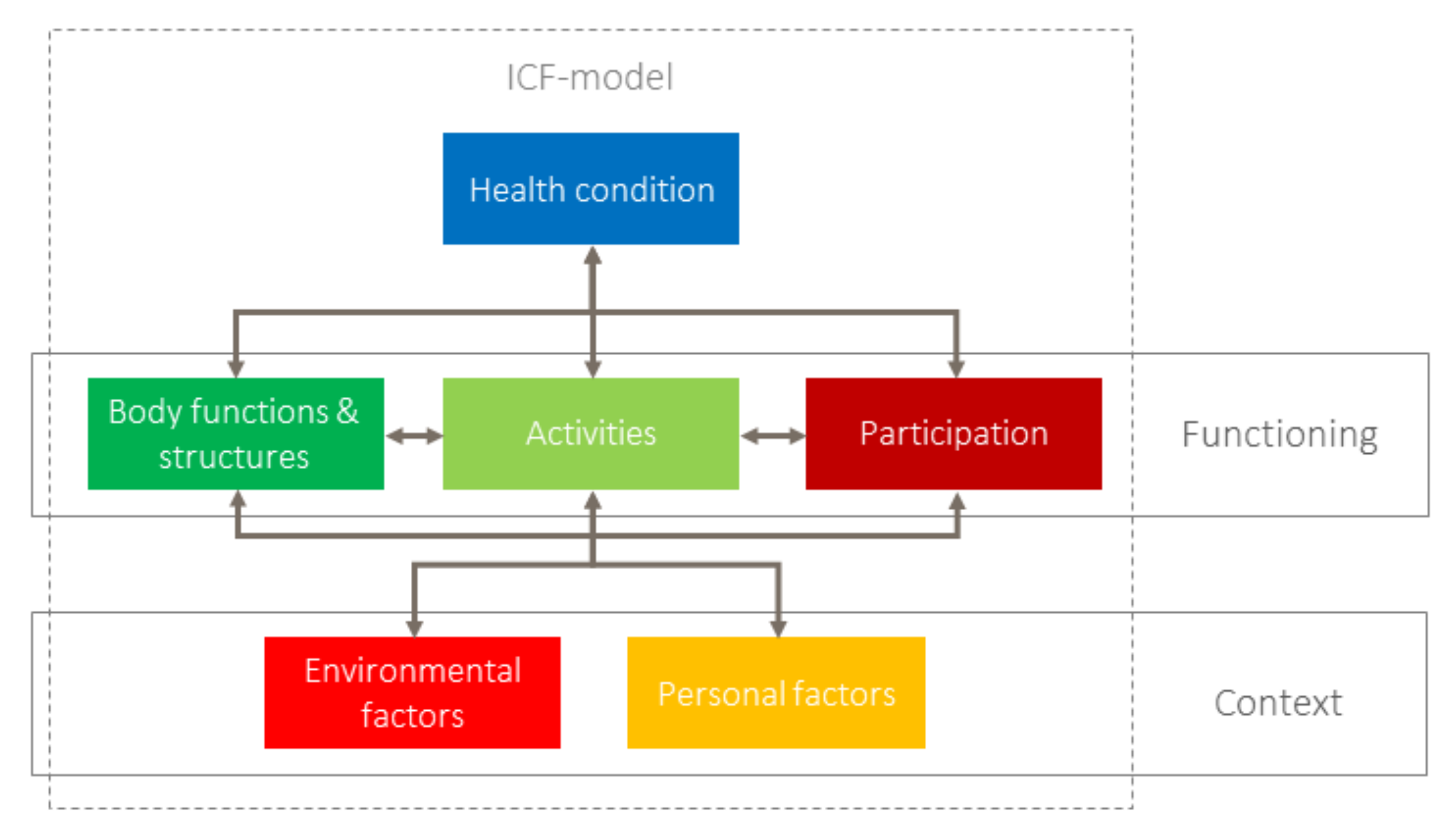
Figure 1: Integration of preventive, promotive, and curative approaches in modern child healthcare.
Evolution of Child Healthcare
Child healthcare has evolved significantly over the past century, transitioning from a primarily curative approach focused on treating disease to a more comprehensive model that emphasizes prevention and health promotion.
Early 20th Century: Disease-Focused Care
Healthcare primarily focused on treating infectious diseases. High child mortality rates due to limited preventive measures and medical knowledge.
Mid-20th Century: Emergence of Preventive Care
Introduction of vaccination programs, well-child visits, and public health initiatives. Significant reduction in infectious disease mortality.
Late 20th Century: Family-Centered Care
Recognition of family’s role in child health. Development of models integrating family preferences and needs into care planning and delivery.
Early 21st Century: Social Determinants Focus
Increased awareness of social, economic, and environmental factors affecting child health. Development of programs addressing social determinants of health.
Current Era: Integrated Care Model
Balanced integration of preventive, promotive, and curative approaches. Enhanced by technology, data analytics, and personalized care strategies.
Key Shifts in Child Healthcare
- From disease treatment to disease prevention and health promotion
- From fragmented care to integrated, coordinated care systems
- From provider-centered to family-centered and child-centered approaches
- From focus on physical health to holistic approach including mental, emotional, and social well-being
- From standardized care to personalized, precision medicine approaches
Preventive Care Approaches
Preventive care encompasses strategies aimed at avoiding the onset of disease, detecting conditions at an early stage, and limiting the impact of established diseases. In pediatric healthcare, prevention is categorized into three levels:
Primary Prevention
Measures aimed at preventing the occurrence of disease or injury before it develops.
- Immunizations: Routine childhood vaccines against infectious diseases
- Nutritional Support: Promoting breastfeeding, preventing micronutrient deficiencies
- Health Education: Teaching families about safety measures and healthy habits
- Environmental Interventions: Reducing exposure to toxins, pollutants, and hazards
- Genetic Counseling: For families with hereditary disease risk
Shifting Trends in Primary Prevention:
- Expanded immunization schedules with new vaccines
- Increased emphasis on early-life nutrition and first 1000 days
- Focus on adverse childhood experiences (ACEs) prevention
- Use of digital tools for preventive education
- Precision approaches based on genetic and environmental risk profiles
Secondary Prevention
Efforts to detect and address health problems at an early stage before they cause significant symptoms or complications.
- Screenings: Growth monitoring, developmental assessments, vision and hearing tests
- Early Detection Programs: Newborn screening, autism screening, mental health assessments
- Surveillance: Regular monitoring for high-risk conditions
- Anticipatory Guidance: Age-appropriate counseling on emerging health issues
Shifting Trends in Secondary Prevention:
- Expanded newborn screening panels using metabolomic and genomic approaches
- Integrated developmental-behavioral screening at routine visits
- Implementation of universal mental health screening
- Technology-enabled home monitoring solutions
- AI-assisted interpretation of screening results
Tertiary Prevention
Interventions to manage established health conditions, prevent complications, and restore function.
- Disease Management: Protocols for chronic conditions like asthma, diabetes, epilepsy
- Rehabilitation Services: Physical, occupational, and speech therapy
- Care Coordination: For children with special healthcare needs
- Assistive Technologies: Supporting function and independence
- Transition Planning: Preparing for adult healthcare systems
Shifting Trends in Tertiary Prevention:
- Telehealth for chronic disease management
- Remote monitoring devices for condition tracking
- Integration of mental health support into chronic disease care
- Patient-reported outcome measures guiding interventions
- Digital health platforms for care coordination
- P: Protection through immunizations and safety measures
- R: Regular screenings and assessments
- E: Education of families about health risks and prevention
- V: Vigilance for developmental warning signs
- E: Early intervention for identified concerns
- N: Nutritional guidance and support
- T: Targeted approach based on risk factors
| Prevention Level | Traditional Approach | Shifting Trend |
|---|---|---|
| Primary | Basic immunization schedule, general safety advice | Expanded vaccines, precision risk assessment, digital health education |
| Secondary | Basic growth measurements, milestone checks | Comprehensive screening panels, AI-assisted interpretation, remote monitoring |
| Tertiary | Clinic-based management, fragmented specialty care | Telehealth, integrated care teams, patient-centered outcomes, digital coordination |
Promotive Care Approaches
Health promotion goes beyond preventing disease to actively creating supportive environments and enabling children to increase control over, and improve, their health. This approach focuses on enhancing well-being rather than just avoiding illness.
Dimensions of Health Promotion in Child Healthcare

Figure 2: Implementation model for health promotion in pediatric care.
Health Education
Empowering children and families with knowledge and skills to make informed health decisions.
- Nutritional Education: Teaching balanced diet principles and healthy eating habits
- Physical Activity Promotion: Encouraging regular exercise and active lifestyle
- Mental Health Literacy: Developing emotional intelligence and coping skills
- Digital Health Literacy: Navigating health information online safely
- Environmental Health Awareness: Understanding environmental impacts on health
Shifting Trends in Health Education:
- Age-appropriate digital education platforms
- Gamification of health education content
- Social media-based health promotion campaigns
- Peer-to-peer education models
- Cultural adaptation of health messaging
Community Empowerment
Creating supportive environments and strengthening community action for child health.
- School Health Programs: Integrating health promotion into educational settings
- Community Partnerships: Collaborating with local organizations and leaders
- Peer Support Networks: Building connections among families with similar challenges
- Community Health Workers: Extending health promotion into neighborhoods
- Youth Engagement: Involving young people in designing health initiatives
Shifting Trends in Community Empowerment:
- Virtual community building and support networks
- Co-design of health promotion interventions with communities
- Asset-based community development approaches
- Integration of health promotion into non-healthcare settings
- Cross-sector collaboration for holistic approaches
Policy Advocacy
Creating supportive policies and regulations that protect and promote child health.
- Health in All Policies: Considering health impacts across policy sectors
- Child-Friendly Urban Planning: Designing spaces that promote health and safety
- School Nutrition Policies: Ensuring healthy food environments
- Air and Water Quality Standards: Protecting children from environmental hazards
- Media and Marketing Regulations: Limiting harmful influences on children’s health choices
Shifting Trends in Policy Advocacy:
- Data-driven policy development using real-time health metrics
- Digital well-being policies for screen time and online safety
- Youth-led advocacy initiatives
- Economic analyses demonstrating health promotion return on investment
- Cross-border policies addressing global health challenges
- P: Participatory approaches involving children and families
- R: Resilience building through life skills development
- O: Optimal environments supporting healthy choices
- M: Multisectoral collaboration beyond healthcare
- O: Ownership of health by communities and individuals
- T: Technology leveraged for broader health impact
- E: Equity focus ensuring benefits reach all children
Curative Care Approaches
Curative care encompasses diagnostic, therapeutic, and management interventions aimed at treating existing health conditions. While preventive and promotive care have gained emphasis, curative care remains essential for addressing illnesses and injuries when they occur.
Acute Care
Short-term care for sudden, severe illnesses or injuries requiring prompt intervention.
- Emergency Services: Trauma care, stabilization, and critical interventions
- Infectious Disease Management: Diagnosis and treatment of acute infections
- Surgical Interventions: Emergency and elective procedures
- Pain Management: Addressing acute pain and discomfort
- Diagnostic Workups: Rapid assessment of acute symptoms
Shifting Trends in Acute Care:
- Telemedicine for initial assessment and triage
- Point-of-care diagnostics reducing time to treatment
- Specialized pediatric emergency protocols
- Family-centered emergency care approaches
- Observation units reducing unnecessary hospitalizations
Chronic Care
Long-term management of persistent health conditions requiring ongoing attention.
- Disease Management Programs: Structured protocols for conditions like asthma, diabetes
- Care Coordination: Orchestrating services across multiple providers
- Medication Management: Optimizing pharmaceutical approaches
- Technology-Assisted Monitoring: Remote tracking of disease parameters
- Self-Management Support: Empowering children and families in care
Shifting Trends in Chronic Care:
- Personalized medicine approaches based on genetic profiles
- Digital therapeutics complementing traditional treatments
- Shared decision-making tools for treatment choices
- Transition programs preparing for adult healthcare
- Integration of mental health support in chronic disease management
Rehabilitation
Interventions aimed at restoring function, enhancing capabilities, and improving quality of life.
- Physical Therapy: Improving mobility, strength, and physical function
- Occupational Therapy: Enhancing daily living skills and independence
- Speech-Language Therapy: Addressing communication and swallowing issues
- Cognitive Rehabilitation: Supporting recovery from brain injuries
- Adaptive Technologies: Tools and devices supporting function
Shifting Trends in Rehabilitation:
- Telerehabilitation extending services to remote areas
- Virtual reality and gaming applications for therapy
- Robotics-assisted rehabilitation
- Community-based rehabilitation models
- Outcome-based reimbursement for rehabilitation services
| Curative Care Domain | Traditional Approach | Modern Approach |
|---|---|---|
| Diagnostic Methods | Basic laboratory tests, X-rays | Advanced imaging, genetic testing, point-of-care diagnostics |
| Treatment Approaches | Standardized protocols, limited options | Personalized medicine, targeted therapies, digital interventions |
| Care Delivery Models | Hospital-centered, provider-driven | Distributed care networks, telehealth, home-based options |
| Decision Making | Physician-directed with limited family input | Shared decision-making, family engagement, child participation |
| Technology Integration | Basic electronic records, limited connectivity | IoT devices, remote monitoring, AI-assisted decisions |
- C: Comprehensive approach addressing biological, psychological, and social aspects
- U: User-centered design of treatment plans and interventions
- R: Responsive care adapting to changing patient needs
- A: Access to services regardless of location or circumstances
- T: Technology-enhanced diagnosis and treatment methods
- I: Integrated with preventive and promotive strategies
- V: Value-based care focusing on outcomes and quality
- E: Evidence-informed practices using latest research
Integrated Care Models
The most significant shift in modern child healthcare is the move toward integrated models that seamlessly combine preventive, promotive, and curative elements. These models recognize that children’s health needs are interconnected and require coordinated approaches.
Integrated Child Healthcare Framework

Figure 3: Framework showing integration of preventive, promotive, and curative healthcare services.
Primary Healthcare Model
A comprehensive approach that integrates all aspects of care with community involvement and multisectoral action.
- Comprehensive Services: Offering preventive, promotive, and curative care in one setting
- First Contact Access: Serving as the entry point to the healthcare system
- Continuity of Care: Maintaining ongoing relationships with providers
- Coordination: Managing referrals and communication across the system
- Community Orientation: Addressing population health needs
Shifting Trends in Primary Healthcare:
- Integration of behavioral health into primary care
- Expanded role of community health workers
- Digital platforms connecting primary care with specialists
- Value-based payment models incentivizing prevention
- Population health management approaches
Family-Centered Care
An approach that places the family at the center of care planning and delivery, recognizing their crucial role in child health.
- Partnership with Families: Collaborative decision-making and care planning
- Information Sharing: Open and honest communication
- Respect for Diversity: Honoring cultural, ethnic, and socioeconomic differences
- Family Strengths: Building on capabilities rather than focusing on deficits
- Family Support: Addressing practical and emotional needs
Shifting Trends in Family-Centered Care:
- Digital tools for family engagement in care
- Family-reported outcome measures
- Training for providers in collaborative communication
- Family partners integrated into healthcare teams
- Care designed around family schedules and preferences
Continuum of Care
A model ensuring seamless services across the lifespan and across different healthcare settings and needs.
- Life Course Approach: Addressing health needs from preconception through adolescence
- Care Transitions: Smooth handoffs between providers and settings
- Health Information Exchange: Secure sharing of health data
- Integrated Care Teams: Multidisciplinary collaboration
- Coordinated Specialty Care: Management of complex conditions
Shifting Trends in Continuum of Care:
- Digital care coordination platforms
- Patient-controlled health information
- Cross-setting quality metrics
- Virtual integrated care teams
- Accountable care organizations spanning the continuum
| Integration Element | Preventive Component | Promotive Component | Curative Component |
|---|---|---|---|
| Well-Child Visit | Immunizations, screenings, anticipatory guidance | Growth and development support, health education | Address acute concerns, chronic condition management |
| School Health Program | Health screenings, safety education | Health literacy curriculum, physical activity programs | School nurse services, first aid, medication management |
| Technology Platform | Preventive service reminders, risk assessments | Health coaching, education resources | Symptom assessment, telehealth consultations |
| Community Health Worker | Home safety checks, screening promotion | Parenting education, community resource connection | Medication adherence support, symptom monitoring |
Technology & Innovation
Technological advances are revolutionizing child healthcare, enabling new approaches to prevention, promotion, and treatment. These innovations are expanding access, improving quality, and creating more personalized care models.
Telehealth
Remote healthcare delivery using telecommunications technology, expanding access and convenience.
- Virtual Visits: Remote consultations for assessment and follow-up
- Specialist Access: Connecting with pediatric subspecialists regardless of location
- Remote Monitoring: Tracking health parameters from home
- School-Based Telehealth: Providing care in educational settings
- Digital Care Coordination: Connecting healthcare teams virtually
Impact on Care Triad:
- Preventive: Increased access to screenings, virtual well-child visits
- Promotive: Remote health education, virtual support groups
- Curative: Continuous management of chronic conditions, acute assessment
mHealth Applications
Mobile health technologies providing tools for monitoring, education, and engagement.
- Health Tracking Apps: Monitoring symptoms, medications, and health behaviors
- Educational Platforms: Age-appropriate health information and guidance
- Wearable Devices: Continuous monitoring of vital signs and activity
- Medication Adherence Tools: Reminders and tracking for treatment plans
- Game-Based Interventions: Engaging children in health management
Impact on Care Triad:
- Preventive: Early warning systems, risk factor monitoring
- Promotive: Gamified health challenges, positive reinforcement
- Curative: Symptom tracking, treatment response monitoring
AI & Analytics
Advanced data analysis and artificial intelligence improving decision-making and personalization.
- Predictive Analytics: Identifying children at risk for health issues
- Clinical Decision Support: AI-assisted diagnostic and treatment guidance
- Precision Medicine: Tailoring interventions based on individual characteristics
- Population Health Management: Analyzing trends to guide interventions
- Natural Language Processing: Extracting insights from clinical documentation
Impact on Care Triad:
- Preventive: Risk stratification, targeted screening recommendations
- Promotive: Personalized health promotion strategies
- Curative: Treatment optimization, outcome prediction
- D: Data-driven decision making using analytics
- I: Interoperability of systems and information sharing
- G: Gamification to engage children in their health
- I: Individualized care through precision approaches
- T: Telehealth expanding access and convenience
- A: Artificial intelligence enhancing clinical decisions
- L: Literacy in digital health skills for families
Equity & Access
A defining characteristic of modern child healthcare is the increased focus on ensuring that all children, regardless of background or circumstances, have access to comprehensive, high-quality services. This emphasis on equity recognizes that social determinants often have a greater impact on health outcomes than medical care alone.
Vulnerable Populations
Targeted approaches to address disparities affecting specific groups of children.
- Children with Special Healthcare Needs: Complex conditions requiring coordinated care
- Immigrant and Refugee Children: Facing language, cultural, and legal barriers
- Children in Rural Areas: Limited access to specialized services
- Children in Poverty: Multiple risk factors affecting health
- Children in Foster Care: Discontinuity of care and complex trauma
Innovative Approaches:
- Cultural adaptation of interventions and materials
- Community health worker models for trusted care
- Telehealth reducing geographic barriers
- Trauma-informed care approaches
- Mobile healthcare units serving underresourced areas
| Dimension of Equity | Traditional Challenge | Modern Approaches |
|---|---|---|
| Geographic Access | Service concentration in urban areas, transportation barriers | Telehealth, mobile units, school-based services, satellite clinics |
| Financial Access | Uninsurance, high out-of-pocket costs | Insurance expansion, sliding scale fees, value-based care models |
| Cultural Access | Language barriers, cultural mismatches, bias | Cultural competence training, diverse workforce, translation services |
| Digital Access | Digital divide, technology limitations | Device programs, public Wi-Fi, low-tech alternatives |
| Informational Access | Health literacy barriers, complex systems | Plain language materials, navigation assistance, educational resources |
Key Principles for Advancing Equity in Child Healthcare
- Universal approaches combined with targeted strategies for vulnerable groups
- Proportionate universalism — allocating resources proportionally to level of disadvantage
- Community engagement in program design and implementation
- Data collection on disparities to guide interventions
- Structural and policy-level approaches rather than individual focus alone
- Cross-sector collaboration addressing multiple determinants simultaneously
Case Studies
These case studies illustrate the application of integrated preventive, promotive, and curative approaches in modern child healthcare.
Case Study 1: Integrated Asthma Management Program
Context: A community with high prevalence of childhood asthma, particularly in low-income neighborhoods.
Preventive Elements:
- Home environment assessments to identify and mitigate triggers
- Air quality monitoring in schools and community spaces
- Regular lung function screening for at-risk children
Promotive Elements:
- School-based education on asthma awareness and management
- Community health worker-led family education sessions
- Policy advocacy for clean air initiatives and smoke-free zones
Curative Elements:
- Streamlined access to medications and spacers
- Digital symptom tracking with alerts to providers
- Telehealth follow-ups after emergency department visits
Outcomes:
- 30% reduction in emergency department visits
- 50% decrease in school absences related to asthma
- Improved medication adherence and self-management skills
- Enhanced community awareness and environmental improvements
Case Study 2: Early Childhood Development Initiative
Context: Rural region with limited access to pediatric services and high rates of developmental delays.
Preventive Elements:
- Universal developmental screening during well-child visits
- Maternal depression screening integrated into child visits
- Vision, hearing, and nutrition assessments
Promotive Elements:
- Home visiting program supporting positive parenting practices
- Community playgroups enhancing socialization and learning
- Mobile literacy program providing books and reading guidance
Curative Elements:
- Telehealth-enabled developmental specialist consultations
- Mobile therapy teams providing interventions locally
- Parent-implemented intervention protocols with remote coaching
Outcomes:
- Increased early identification of developmental concerns
- Reduced average age at intervention initiation from 36 to 18 months
- Improved school readiness metrics in community
- Enhanced parental confidence and engagement
Key Learnings from Case Studies
- Integrated approaches yield synergistic benefits exceeding the sum of individual interventions
- Community engagement is critical for program acceptance and sustainability
- Technology enables extension of services to previously underserved populations
- Data-driven approaches allow for continuous improvement and adaptation
- Cross-sector collaboration amplifies impact beyond what healthcare alone can achieve
Future Directions
The field of child healthcare continues to evolve rapidly, with several emerging trends poised to further transform preventive, promotive, and curative approaches in the coming years.
Emerging Trends in Child Healthcare
Precision Population Health
Combining population-level data with individual genetic, environmental, and social information to tailor interventions at unprecedented levels of specificity while addressing community-wide health needs.
Ambient Clinical Intelligence
AI systems that passively observe clinical encounters, automatically documenting information and providing real-time decision support without requiring direct user interaction, freeing providers to focus on the child.
Digital Therapeutics
Evidence-based therapeutic interventions delivered via software applications to prevent, manage, or treat medical conditions, providing new options for behavioral health, developmental support, and chronic disease management.
Climate-Responsive Care
Healthcare systems adapting to address the growing impact of climate change on child health through modified screening protocols, surveillance systems, and interventions targeting climate-sensitive conditions.
Microbiome-Informed Approaches
Leveraging growing understanding of the human microbiome to develop new preventive and therapeutic strategies, from precision probiotics to microbiome transplantation for various conditions.
Integrated Virtual Care Ecosystems
Comprehensive digital platforms that seamlessly connect in-person care, telehealth, remote monitoring, education, and community resources in a unified experience for families navigating the healthcare system.
Challenges and Opportunities
| Challenge | Opportunity |
|---|---|
| Digital divide exacerbating health disparities | Targeted digital equity initiatives; low-tech complementary solutions |
| Fragmentation across healthcare and social service systems | Integrated data platforms; care coordination technologies; policy alignment |
| Workforce shortages in pediatric specialties | Task-shifting models; telehealth consultation networks; AI-assisted triage |
| Rising costs of advanced technologies | Value-based payment models; shared resource networks; scaled solutions |
| Privacy and security concerns with health data | Privacy-preserving analytics; transparent data governance; family control |
Nursing Implications
Nurses play a pivotal role in implementing and advancing integrated approaches to child healthcare. The shifting trends in preventive, promotive, and curative care have significant implications for nursing practice, education, and leadership.
Practice Implications
- Expanded scope in preventive and promotive interventions
- Integration of social determinants assessment into routine care
- Enhanced care coordination across settings and services
- Telehealth and digital health tool implementation
- Culturally responsive care approaches for diverse populations
- Family engagement and partnership strategies
Education and Training Needs
- Enhanced focus on preventive and promotive concepts
- Population health competencies development
- Digital literacy and health technology skills
- Cultural humility and equity-focused approaches
- Interprofessional collaboration training
- Quality improvement and implementation science
Leadership Opportunities
- Advocacy for policies supporting comprehensive care
- Design and implementation of integrated care models
- Development of community partnerships and initiatives
- Quality measurement and improvement leadership
- Innovative practice model development and testing
- Mentorship of new generations of pediatric nurses
- I: Inform families with evidence-based health education
- N: Navigate complex systems on behalf of children and families
- T: Transform care delivery through innovation and quality improvement
- E: Engage with communities to address health determinants
- G: Guide health promotion and disease prevention efforts
- R: Respond to emerging health challenges with adaptability
- A: Advocate for policies that support child health and well-being
- T: Translate research into effective, evidence-based practice
- E: Evaluate outcomes to continuously improve care quality
Essential Competencies for Modern Pediatric Nursing
| Competency Domain | Key Skills | Application in Integrated Care |
|---|---|---|
| Health Assessment | Comprehensive assessment including social determinants; risk factor identification; developmental monitoring | Synthesizing physical, developmental, behavioral, and social data to inform interventions across the care continuum |
| Care Coordination | Interprofessional collaboration; system navigation; transition management; referral management | Ensuring seamless delivery of preventive, promotive, and curative services across multiple providers and settings |
| Health Promotion | Motivational interviewing; health coaching; anticipatory guidance; educational design | Empowering families with knowledge and skills to promote optimal health and prevent disease |
| Technology Utilization | Telehealth delivery; remote monitoring interpretation; digital tool application; data analytics | Leveraging digital solutions to extend reach of services and enhance effectiveness of interventions |
| Cultural Competence | Cultural humility; inclusive communication; bias awareness; community engagement | Ensuring care approaches respect and respond to diverse values, beliefs, and needs |
Conclusion
The landscape of child healthcare is evolving rapidly, with a clear shift toward more integrated, holistic approaches that combine preventive, promotive, and curative elements. This transition represents a fundamental reimagining of how healthcare systems can best support children’s health and development.
Key Takeaways
Integration is Essential: The most effective approaches to child health seamlessly blend preventive, promotive, and curative services rather than treating them as separate domains. This integration occurs at multiple levels—from individual providers to healthcare systems to community-wide initiatives.
Beyond Medical Models: Modern child healthcare extends well beyond traditional medical approaches to encompass social, environmental, educational, and policy dimensions. Addressing the broader determinants of health is becoming as important as providing clinical services.
Technology as Enabler: Digital tools, telehealth, AI, and other technologies are not simply add-ons to existing care models but transformative forces enabling entirely new approaches to service delivery, care coordination, and family engagement.
Equity as Central Focus: The shift toward more equitable approaches is not peripheral but central to improving child health outcomes. Targeted strategies for vulnerable populations combined with universal approaches represent the most promising path forward.
Collaborative Imperative: No single sector or profession can address the complex factors influencing child health. Multidisciplinary teams, cross-sector partnerships, and community collaborations are becoming the norm rather than the exception.
As these shifting trends continue to reshape child healthcare, nursing professionals have unprecedented opportunities to lead, innovate, and advocate for approaches that holistically address children’s needs. By embracing these changes and developing the competencies needed for integrated care, nurses can play a pivotal role in improving health outcomes for all children, particularly those facing the greatest challenges.
“The future of child healthcare lies not in choosing between prevention, promotion, or treatment, but in reimagining how these approaches can work together seamlessly to support every child’s journey toward optimal health and well-being.”
References
1. World Health Organization. (2023). Primary health care. https://www.who.int/health-topics/primary-health-care
2. American Academy of Pediatrics. (2023). Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents (4th ed.).
3. Center for Health Care Strategies. (2021). Accelerating Child Health Care Transformation: Key Opportunities for Improving Pediatric Care.
4. Echelon Health. (2023). Five Preventive Health Trends for 2025. https://www.echelon.health/five-preventive-health-trends-2025/
5. Wendimagegn, N. F., & Bezuidenhout, M. C. (2019). Integrating promotive, preventive, and curative health care services at hospitals and health centers in Addis Ababa, Ethiopia. Journal of Multidisciplinary Healthcare, 12, 243-255.
6. Oceanside Pediatrics. (2023). The Future of Pediatric Care: Trends and Predictions in the US. https://www.oceansidepediatricsjax.com/the-future-of-pediatric-care-trends-and-predictions-in-the-us.html
7. JAMA Pediatrics. (2022). Five-Year Trends in US Children’s Health and Well-being, 2016-2020.
8. Exemplars in Global Health. (2023). Primary Health Care. https://www.exemplars.health/topics/primary-health-care
9. Centers for Disease Control and Prevention. (2023). Preventive Health Care. https://www.cdc.gov/healthcommunication/toolstemplates/entertainmented/tips/PreventiveHealth.html
10. UNICEF. (2023). Child health and survival. https://www.unicef.org/child-health-and-survival

Social Determinants of Health
Addressing conditions in which children are born, grow, learn, play, and live that affect health outcomes.
Shifting Approaches: