Nursing Management in Common Childhood Diseases
Respiratory System: Congenital Disorders
Table of Contents
Tracheoesophageal Fistula (TEF) Overview & Types Pathophysiology Clinical Manifestations Diagnostic Assessment Nursing Management Nursing Care Plan Diaphragmatic Hernia Overview & Types Pathophysiology Clinical Manifestations Diagnostic Assessment Nursing Management Nursing Care Plan Comparison: TEF vs CDHTracheoesophageal Fistula (TEF)
Overview
Tracheoesophageal fistula (TEF) is a congenital anomaly involving the abnormal development of the trachea and esophagus during fetal development. It typically involves an abnormal connection (fistula) between the trachea and esophagus, often accompanied by esophageal atresia (EA).
- Incidence: 1 in 3000-4500 live births
- More common in premature infants
- Associated with VACTERL syndrome in 25% of cases
- Most common type: Type C (85% of cases)
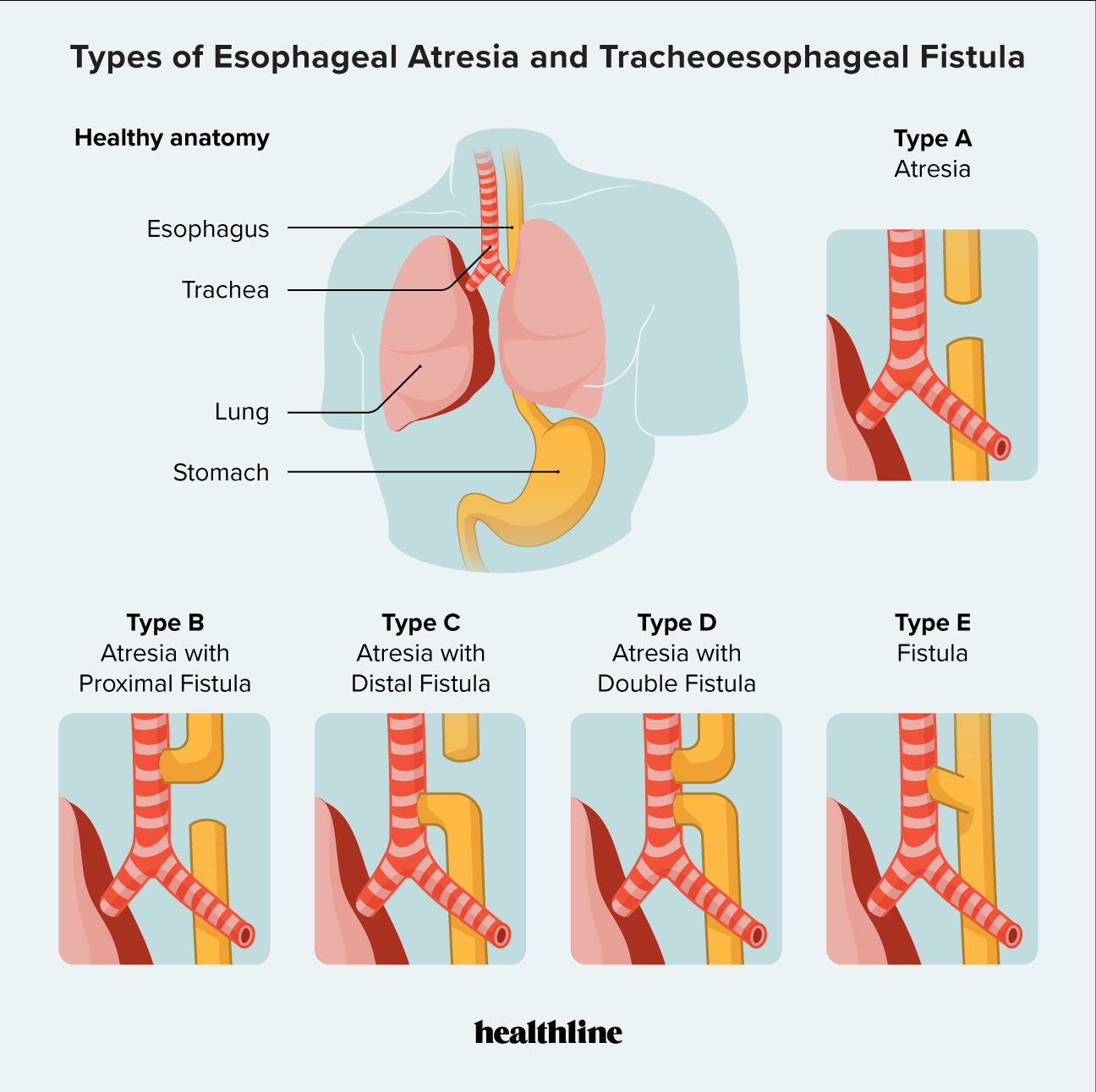
Types of Tracheoesophageal Fistula
The most widely used classification system for TEF is the Gross classification:
Classification of Tracheoesophageal Fistula (TEF) types according to Gross classification
| Type | Description | Frequency |
|---|---|---|
| Type A | Esophageal atresia without fistula (pure EA) | 10% |
| Type B | Esophageal atresia with proximal TEF | <1% |
| Type C | Esophageal atresia with distal TEF | 85% |
| Type D | Esophageal atresia with proximal and distal TEFs | <1% |
| Type E | TEF without esophageal atresia (H-type fistula) | 4% |
Pathophysiology
Tracheoesophageal fistula occurs during embryonic development, typically between the 4th and 5th weeks of gestation. During this period, the primitive foregut should normally divide into the anterior respiratory tract and the posterior esophagus. Failure of this separation results in TEF.
Key Pathophysiological Consequences
- Aspiration Risk: Abnormal communication allows food/secretions to enter the respiratory tract
- Blind Pouch: In esophageal atresia, oral secretions pool in the proximal pouch
- Gastric Distension: Air can pass through the distal fistula into the stomach when the baby cries or is ventilated
- Esophageal Dysmotility: The distal esophagus in EA has poor or absent peristaltic waves
Associated Conditions: VACTERL Syndrome
TEF is commonly associated with VACTERL syndrome, which includes:
- Vertebral defects
- Anorectal malformations
- Cardiovascular defects
- Tracheoesophageal defects
- Renal anomalies
- Limb deformities
VACTERL syndrome is diagnosed when 3 or more of these anomalies are present (occurs in ~25% of TEF cases).
Clinical Manifestations
Mnemonic: “The Three Cs of TEF”
- Coughing
- Choking
- Cyanosis during feeding
Common Signs & Symptoms
| Clinical Manifestation | Description |
|---|---|
| Excessive Oral Secretions | Neonate drools and has substantial mucus with excessive oral secretions due to inability to swallow |
| Feeding Difficulties | If suckling at breast or bottle is attempted, baby appears to choke and has difficulty maintaining airway |
| Respiratory Distress | Aspiration pneumonia may develop due to reflux of gastric contents into the lungs through the fistula |
| Seal-bark Cough | A characteristic sonorous “seal-bark” cough that may indicate concomitant tracheomalacia |
| Abdominal Distension | In cases with distal TEF, air enters the GI tract through the fistula causing distension |
| Inability to Pass NG Tube | Attempted passage of a nasogastric tube becomes obstructed at approximately 10-11 cm from the lips |
The presence of the “Three Cs” (Coughing, Choking, Cyanosis) during feeding attempts in a newborn should immediately raise suspicion of TEF. Attempts to feed these infants should be discontinued until TEF is ruled out.
Diagnostic Assessment
Prenatal Indicators
- Polyhydramnios: Present in approximately 33% of mothers with fetuses with EA and distal TEF, and in virtually 100% of mothers with fetuses with EA without fistula
- Small or absent gastric bubble on prenatal ultrasound
Postnatal Diagnostic Tests
| Diagnostic Test | Findings | Purpose |
|---|---|---|
| Inability to pass NG tube | Tube becomes obstructed at 10-11 cm from lips | Initial bedside screening test |
| Chest X-ray with tube in place | Visualizes coiled tube in blind upper esophageal pouch | Confirms esophageal atresia |
| Chest X-ray with contrast | Shows contrast material outlining the blind upper pouch | Confirms esophageal atresia, may show fistula |
| Abdominal X-ray | Air in GI tract suggests distal TEF; absence of gas may indicate isolated EA | Differentiates types of TEF |
| Echocardiography | Evaluates for congenital heart defects | Rules out associated VACTERL anomalies |
| Renal Ultrasound | Evaluates for kidney abnormalities | Rules out associated VACTERL anomalies |

Plain X-ray showing radio-opaque tube in the blind upper esophageal pouch
Nursing Management
Preoperative Management
Key Nursing Interventions – Preoperative
- Positioning: Elevate head of bed 30-45° to reduce risk of aspiration
- Suction Management: Place a 10-French Replogle double-lumen tube in the proximal pouch for continuous suctioning of secretions
- Respiratory Assessment: Monitor respiratory status closely; assess for signs of respiratory distress
- NPO Status: Maintain strict NPO status
- IV Therapy: Establish IV access for fluids and medication administration
- Antibiotic Therapy: Administer prophylactic antibiotics as ordered (typically ampicillin and gentamicin)
- Parent Education: Explain condition, treatment plan, and expected outcomes to parents
Surgical Management
Surgical correction is the definitive treatment for TEF and EA. The procedure typically involves:
- Division of the fistula and closure of the tracheal defect
- Primary anastomosis of the esophagus (if possible)
- Creation of a gastrostomy tube (in some cases)
- For long-gap EA, staged repair may be necessary
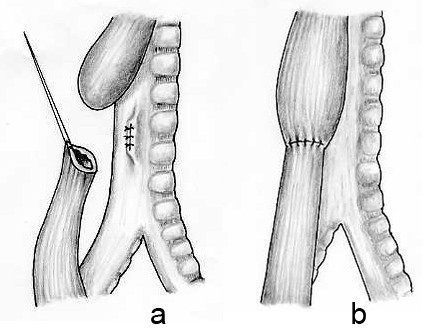
Operative repair of an esophageal atresia and distal tracheoesophageal fistula
Postoperative Management
Key Nursing Interventions – Postoperative
- Respiratory Management: Continue ventilatory support as needed; monitor oxygen saturation
- Pain Management: Assess pain regularly using age-appropriate scales; administer analgesics as ordered
- Chest Tube Care: If present, monitor drainage and maintain water seal at 2cm; avoid suction which could encourage anastomotic leak
- Wound Care: Assess incision site for signs of infection; maintain clean, dry dressing
- Nutritional Support: Maintain NPO status until anastomosis is healed; provide TPN or enteral feeds via gastrostomy if present
- Monitoring for Complications: Watch for signs of anastomotic leak (increased secretions, respiratory distress, fever)
- Gradual Feeding Introduction: Once anastomosis is healed, feeding is gradually introduced following surgeon’s orders
- Anastomotic Leak: Signs include increased secretions, respiratory distress, fever
- Stricture Formation: May cause feeding difficulties and regurgitation
- Gastroesophageal Reflux: Common long-term complication
- Recurrent TEF: Can develop at the site of the original repair
- Tracheomalacia: Results in a characteristic “barking” cough
Nursing Care Plan
Nursing Diagnosis 1: Impaired Gas Exchange
Related to: Abnormal opening between esophagus and trachea
As evidenced by: Cyanosis, respiratory distress, abnormal arterial blood gases
Expected Outcomes:
- Infant will maintain oxygen saturation >95% on prescribed oxygen therapy
- Infant will demonstrate normal respiratory rate and pattern for age
- Infant will exhibit pink skin color and mucous membranes
Nursing Interventions:
- Monitor vital signs, especially respiratory rate, effort, and oxygen saturation, at least hourly
- Position infant with head elevated 30-45 degrees to reduce risk of aspiration
- Maintain continuous suction of the proximal esophageal pouch
- Administer oxygen therapy as prescribed
- Assess breath sounds every 2-4 hours and as needed
- Monitor arterial blood gas results and report abnormalities
- Maintain IV hydration to prevent thick secretions
Nursing Diagnosis 2: Risk for Aspiration
Related to: Abnormal connection between trachea and esophagus, pooling of secretions
Expected Outcomes:
- Infant will remain free of aspiration
- Infant will maintain clear breath sounds
- Infant will not exhibit signs of respiratory distress
Nursing Interventions:
- Maintain NPO status until surgical repair is complete
- Position infant with head elevated 30-45 degrees
- Ensure proper functioning of sump tube in proximal pouch with continuous suction
- If a gastrostomy tube is present, ensure proper functioning and drainage
- Monitor for signs of aspiration: increased secretions, respiratory distress, decreased oxygen saturation
- Have suction equipment readily available at bedside
- Monitor quality, color, and amount of secretions
Nursing Diagnosis 3: Anxiety (Parents)
Related to: Hospitalization of infant, unfamiliar environment, surgical procedure, uncertain prognosis
As evidenced by: Verbalization of concerns, increased questioning, restlessness, tearfulness
Expected Outcomes:
- Parents will verbalize understanding of infant’s condition and treatment plan
- Parents will demonstrate appropriate bonding behaviors with infant
- Parents will utilize effective coping strategies
Nursing Interventions:
- Establish a therapeutic relationship with parents/family
- Provide clear, concise information about infant’s condition, procedures, and treatments
- Encourage parental involvement in infant’s care as appropriate
- Facilitate skin-to-skin contact when infant’s condition permits
- Refer to support services: social work, pastoral care, parent support groups
- Allow expression of feelings and concerns; validate emotional responses
- Provide anticipatory guidance about expected course and home care needs
Diaphragmatic Hernia
Overview
Congenital diaphragmatic hernia (CDH) is a birth defect characterized by incomplete formation of the diaphragm, allowing abdominal organs to migrate into the thoracic cavity during fetal development. This results in pulmonary hypoplasia and can cause severe respiratory distress at birth.
- Incidence: 1 in 2500-4000 live births
- Left-sided hernias (Bochdalek) are most common (80-90%)
- Mortality rate: 30-50%, depending on severity and associated anomalies
- Liver position (intrathoracic vs. intra-abdominal) is a significant prognostic factor
Types of Diaphragmatic Hernia
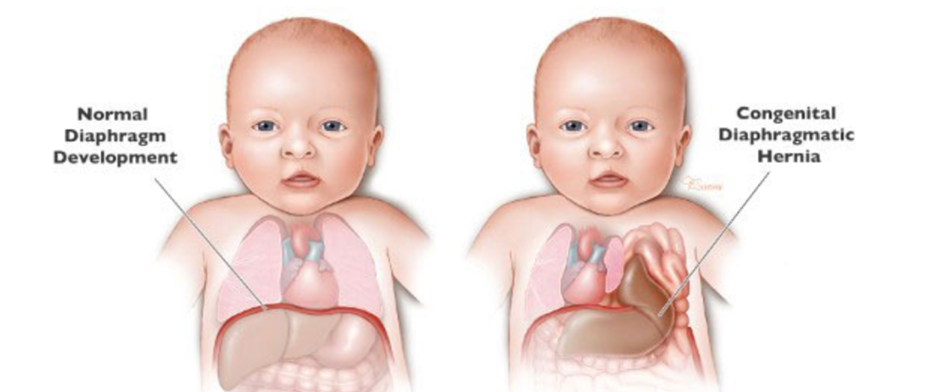
Comparison of normal diaphragm vs. congenital diaphragmatic hernia
| Type | Description | Frequency |
|---|---|---|
| Bochdalek Hernia | Posterolateral defect, most commonly on the left side | 80-90% |
| Morgagni Hernia | Anterior defect, usually right-sided | 2-3% |
| Central Hernia | Defect in the central tendon of the diaphragm | Rare |
| Total Absence | Complete absence of the diaphragm (rare, very poor prognosis) | Extremely rare |
Pathophysiology
Congenital diaphragmatic hernia occurs during embryonic development when the diaphragm fails to close properly between the 8th and 10th weeks of gestation. This allows abdominal contents to herniate into the chest cavity at a critical time of lung development.
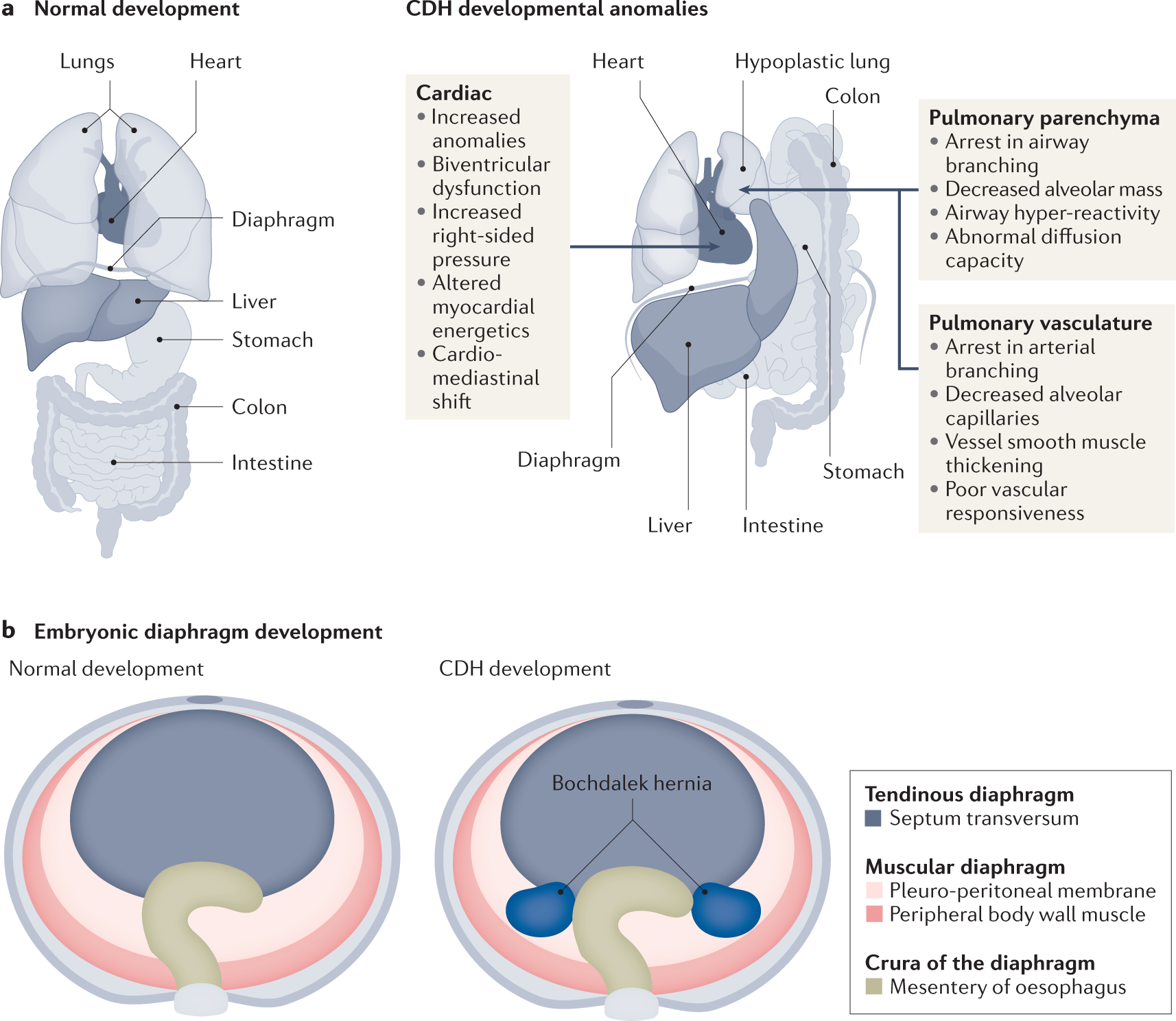
Key Pathophysiological Consequences
- Pulmonary Hypoplasia: Compression of developing lungs by herniated abdominal organs leads to underdevelopment
- Pulmonary Hypertension: Abnormal development of pulmonary vasculature leads to increased pulmonary vascular resistance
- Mediastinal Shift: Displacement of heart and mediastinum away from the affected side
- Decreased Lung Compliance: Hypoplastic lungs have decreased surfactant and functional residual capacity
Prognostic Indicators
Several factors are used to predict prognosis in CDH:
- Lung-to-Head Ratio (LHR): Ultrasound measurement of contralateral lung size relative to head circumference
- LHR < 1.0: Poor prognosis (increased ECMO need, lower survival)
- LHR > 1.4: Better prognosis (higher survival rate)
- Observed/Expected LHR (O/E LHR): Adjusts for gestational age
- O/E LHR < 25%: Severe pulmonary hypoplasia, survival < 30%
- O/E LHR > 46%: Mild hypoplasia, survival > 85%
- Liver Position: Intrathoracic liver associated with worse prognosis
- Associated Anomalies: Presence of other congenital defects worsens prognosis
Clinical Manifestations
Mnemonic: “DIAPHRAGM”
- Distress, respiratory
- Increased work of breathing
- Asymmetric chest movement
- Pulmonary hypoplasia
- Heart sounds displaced
- Retractions and grunting
- Absent breath sounds on affected side
- GI sounds in chest
- Mediastinal shift
Common Signs & Symptoms
| Clinical Manifestation | Description |
|---|---|
| Respiratory Distress | Immediate and severe respiratory distress at birth, including tachypnea, grunting, retractions |
| Cyanosis | Bluish discoloration due to hypoxemia; may be refractory to oxygen therapy |
| Scaphoid Abdomen | Concave or flat-appearing abdomen due to abdominal contents in thorax |
| Barrel-shaped Chest | Enlarged chest on the affected side due to herniated abdominal contents |
| Asymmetrical Chest Movement | Unequal chest expansion during respiration |
| Decreased Breath Sounds | Diminished or absent breath sounds on the affected side |
| Bowel Sounds in Chest | Auscultation reveals intestinal sounds in the thoracic cavity |
| Displaced Heart Sounds | Heart sounds shifted away from the affected side (to the right in left-sided CDH) |
Respiratory distress in a newborn with a scaphoid abdomen and barrel chest should immediately raise suspicion of CDH. Avoid bag-mask ventilation if possible, as it can rapidly distend the stomach and intestines, further compromising lung function.
Diagnostic Assessment
Prenatal Diagnosis
- Ultrasound: Most CDH cases are detected during routine prenatal ultrasound (typically 18-20 weeks)
- MRI: Provides detailed assessment of herniated organs and lung volumes
- Echocardiography: To rule out associated cardiac anomalies
Fetal ultrasound showing congenital diaphragmatic hernia with stomach visible in thorax
Postnatal Diagnostic Tests
| Diagnostic Test | Findings | Purpose |
|---|---|---|
| Chest X-ray | Shows intestinal loops in thorax, mediastinal shift, pulmonary hypoplasia | Confirms diagnosis and assesses severity |
| Arterial Blood Gases | Hypoxemia, respiratory acidosis, metabolic acidosis | Assesses respiratory status and acid-base balance |
| Echocardiogram | Evaluates cardiac position, function, and pulmonary hypertension | Assesses cardiac status and pulmonary vascular resistance |
| Head Ultrasound | Screening for intracranial abnormalities | Evaluates for associated anomalies |
| Chromosomal Studies | May reveal genetic abnormalities | Determines if CDH is part of a genetic syndrome |
Nursing Management
Delivery Room Management
Key Nursing Interventions – Delivery Room
- Immediate Intubation: Avoid bag-mask ventilation; immediate intubation to control ventilation
- Gastric Decompression: Place 10 Fr salem sump orogastric or nasogastric tube to low continuous suction
- Oxygen Management: Start inspired oxygen at 50%; goal saturations >65% at 5 minutes, >75% at 10 minutes of life
- Monitoring: Place preductal pulse oximeter (right hand) to assess oxygenation
- Transport: Coordinate rapid transfer to NICU with minimal stimulation
NICU Management
Key Nursing Interventions – NICU
- Monitoring:
- Pre- and post-ductal oxygen saturations
- Arterial blood pressure
- Transcutaneous CO2
- End-tidal CO2
- Ventilation Strategy:
- “Gentle ventilation” with permissive hypercapnia
- Target PaCO2: 45-65 mmHg, pH >7.25
- Low pressure ventilation (PIP <25 cmH2O)
- Consider high-frequency oscillatory ventilation if conventional ventilation fails
- Fluid Management:
- Restrict fluids (<80 mL/kg/day)
- Maintain strict I/O
- Hemodynamic Support:
- Maintain mean arterial pressure 40-45 mmHg
- Inotropes as needed (typically dopamine first-line)
- Pulmonary Hypertension Management:
- Inhaled nitric oxide for confirmed pulmonary hypertension
- Consider prostaglandins for impaired left ventricular function
- ECMO Consideration: For infants who fail conventional management
Surgical Management
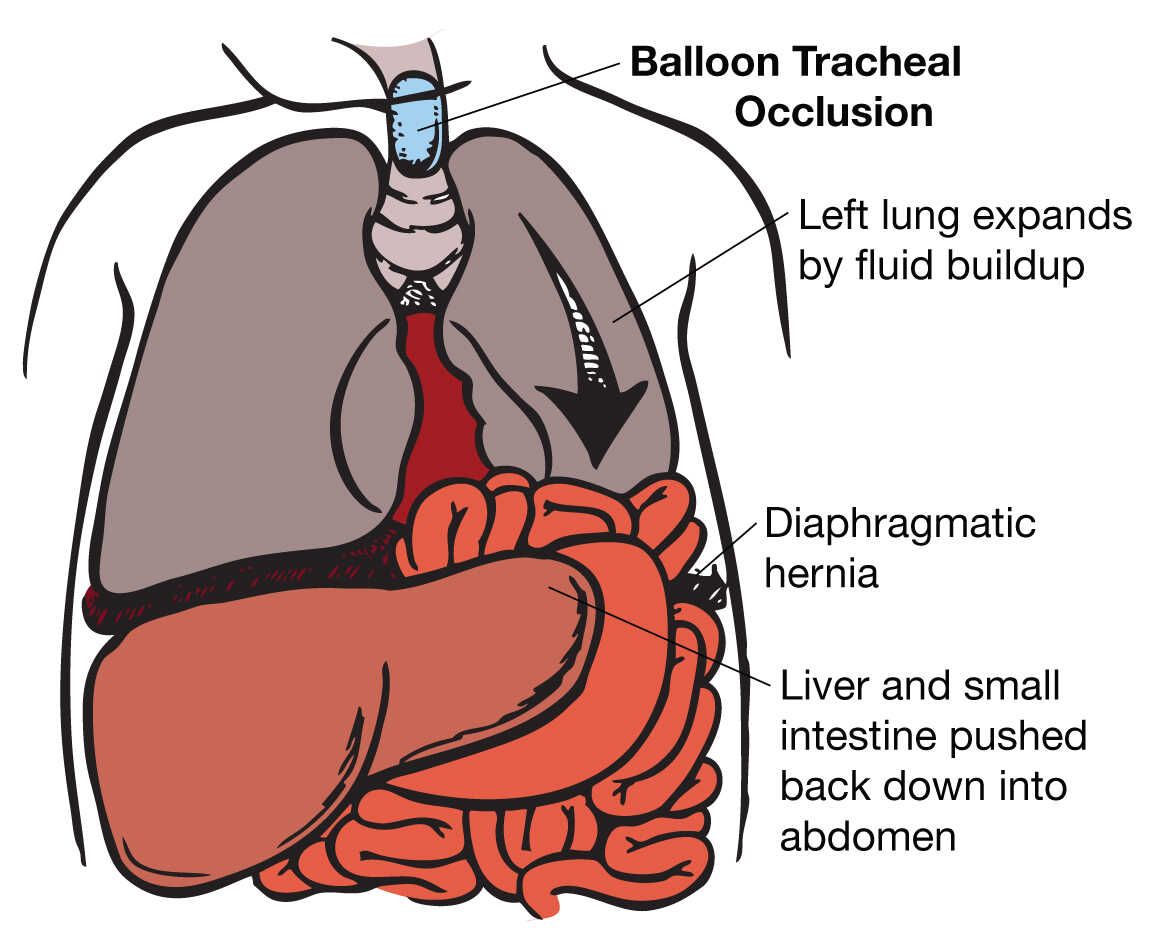
Surgical repair is performed once the infant is physiologically stable, which may be days to weeks after birth. The timing depends on the infant’s condition.

Surgical repair of congenital diaphragmatic hernia
The surgical approach includes:
- Reduction of herniated organs back into the abdominal cavity
- Closure of the diaphragmatic defect (primary closure or with patch)
- Possible placement of chest tube
Postoperative Management
Key Nursing Interventions – Postoperative
- Respiratory Management: Continue ventilatory support; monitor for respiratory compromise
- Pain Management: Regular pain assessment and administration of analgesics
- Monitoring for Compartment Syndrome:
- Assess for decreased distal pulses
- Monitor for abdominal distention
- Track urine output
- Watch for skin discoloration
- Gastric Decompression: Maintain OG/NG tube to low continuous suction
- Wound Care: Monitor surgical site for signs of infection
- Nutritional Support: NPO initially; gradual introduction of feeds when bowel function returns
- Chronic Lung Disease: May require long-term oxygen therapy
- Gastroesophageal Reflux: Common complication requiring medication or surgical intervention
- Growth Delay: Common due to increased metabolic demands and feeding challenges
- Developmental Delay: Monitor for developmental milestones and refer for early intervention
- Chest Wall Deformities: May develop scoliosis or pectus deformities
- Recurrence: Especially in large defects requiring patch repair
Nursing Care Plan
Nursing Diagnosis 1: Impaired Gas Exchange
Related to: Pulmonary hypoplasia, decreased functional lung tissue, pulmonary hypertension
As evidenced by: Hypoxemia, respiratory acidosis, increased work of breathing, cyanosis
Expected Outcomes:
- Infant will maintain preductal oxygen saturation >85% with prescribed ventilatory support
- Infant will demonstrate improved arterial blood gas values (pH >7.25, PaCO2 45-65 mmHg)
- Infant will demonstrate decreased work of breathing
Nursing Interventions:
- Monitor pre- and post-ductal oxygen saturations continuously; report differences >10%
- Assess respiratory status including rate, effort, breath sounds at least hourly
- Maintain proper endotracheal tube position and secure fixation
- Collaborate with respiratory therapy to ensure optimal ventilator settings
- Maintain proper positioning to optimize ventilation
- Monitor arterial blood gases and report significant changes
- Minimize stimulation and procedures that might exacerbate pulmonary hypertension
- Administer medications to manage pulmonary hypertension as prescribed
Nursing Diagnosis 2: Decreased Cardiac Output
Related to: Mediastinal shift, pulmonary hypertension, right-to-left shunting
As evidenced by: Hypotension, tachycardia, poor perfusion, metabolic acidosis
Expected Outcomes:
- Infant will maintain mean arterial pressure within acceptable range (40-45 mmHg)
- Infant will demonstrate adequate perfusion (capillary refill <3 seconds)
- Infant will maintain appropriate urine output (≥1 mL/kg/hour)
Nursing Interventions:
- Monitor blood pressure continuously via arterial line
- Assess perfusion: capillary refill, extremity temperature, skin color every hour
- Maintain accurate intake and output measurement; report urine output <1 mL/kg/hour
- Administer vasoactive medications as prescribed (dopamine, epinephrine)
- Monitor for signs of right heart failure (hepatomegaly, edema)
- Position to minimize pressure on the vena cava and optimize cardiac output
- Monitor electrolyte levels and correct imbalances
Nursing Diagnosis 3: Risk for Fluid Volume Deficit
Related to: Restricted fluid intake, third-spacing, increased insensible losses
Expected Outcomes:
- Infant will maintain adequate hydration status
- Infant will maintain serum electrolytes within normal limits
- Infant will maintain urine output ≥1 mL/kg/hour
Nursing Interventions:
- Administer IV fluids as prescribed (typically restricted to <80 mL/kg/day)
- Monitor strict intake and output hourly
- Assess for signs of dehydration: dry mucous membranes, sunken fontanelles, decreased urine output
- Monitor weight daily
- Monitor electrolyte levels and report abnormalities
- Ensure OG/NG tube is functioning properly to quantify gastric losses
- Adjust fluid therapy based on clinical status in collaboration with medical team
Nursing Diagnosis 4: Risk for Impaired Parent-Infant Attachment
Related to: Separation due to intensive care needs, invasive procedures, uncertain prognosis
Expected Outcomes:
- Parents will demonstrate appropriate attachment behaviors
- Parents will participate in infant’s care as condition allows
- Parents will verbalize understanding of infant’s condition and treatment plan
Nursing Interventions:
- Encourage parents to visit and touch their infant as condition permits
- Facilitate skin-to-skin contact when infant’s condition stabilizes
- Involve parents in care decisions and updates
- Teach parents meaning of equipment and procedures
- Provide privacy for parent-infant interaction
- Support parents in expressing emotions and concerns
- Refer to support services: social work, pastoral care, parent support groups
- Encourage parents to bring personal items for infant (photos, small toys, special blanket)
Comparison: TEF vs CDH
Comparing Tracheoesophageal Fistula and Diaphragmatic Hernia
| Feature | Tracheoesophageal Fistula | Diaphragmatic Hernia |
|---|---|---|
| Incidence | 1 in 3000-4500 births | 1 in 2500-4000 births |
| Embryologic Timing | 4-5 weeks gestation | 8-10 weeks gestation |
| Primary Anatomic Defect | Abnormal connection between trachea and esophagus | Incomplete closure of diaphragm |
| Primary Pathophysiology | Communication between respiratory and digestive tracts | Pulmonary hypoplasia due to compression |
| Most Common Presentation | Excessive salivation, choking with feeds, inability to pass NG tube | Immediate respiratory distress, scaphoid abdomen, barrel chest |
| Diagnostic Confirmation | X-ray with radiopaque catheter in proximal pouch | Chest X-ray showing bowel in thorax, mediastinal shift |
| Emergency Management | Continuous suction of proximal pouch, NPO, position with head elevated | Immediate intubation, avoid bag-mask ventilation, gastric decompression |
| Surgical Timing | Often within first few days of life | Delayed until physiologically stable (days to weeks) |
| Major Nursing Concerns | Aspiration prevention, airway management, feeding issues | Ventilation management, pulmonary hypertension, fluid balance |
| Long-term Complications | GERD, tracheomalacia, stricture formation, recurrent TEF | Chronic lung disease, GERD, developmental delay, growth issues |
| Associated Syndromes | VACTERL association (~25% of cases) | Chromosomal abnormalities (trisomies 13, 18, 21) |
| Mortality Rate | ~10% (higher with complex cardiac anomalies) | 30-50% (depends on severity and associated anomalies) |
- Respiratory Management: Both conditions affect respiratory function, but through different mechanisms
- Nutritional Support: Both require careful feeding strategies and often delayed oral feeding
- Parental Support: Both are life-threatening conditions requiring complex care and emotional support
- Monitoring for Complications: Both require vigilant post-operative monitoring and long-term follow-up
- Developmental Assessment: Both may impact long-term growth and development
