Thermodynamics in Nursing Practice
Essential Principles for Evidence-Based Patient Care
Learning Objectives
- Understand fundamental thermodynamics principles in healthcare
- Apply heat transfer mechanisms to nursing interventions
- Recognize thermodynamics in temperature regulation disorders
- Implement evidence-based thermal management strategies
1. Thermodynamics Fundamentals
Thermodynamics forms the scientific foundation for understanding energy transfer in biological systems. In nursing practice, thermodynamics principles guide temperature management, equipment operation, and physiological assessment. The study of thermodynamics reveals how energy flows between patients and their environment, directly impacting clinical outcomes and patient safety.
Core Definitions
System
A defined region of space containing matter or energy under study. In nursing, the human body serves as a complex thermodynamic system exchanging energy with the environment.
Energy
The capacity to perform work or transfer heat. Human metabolism converts chemical energy into thermal energy, maintaining core temperature within narrow ranges.
Temperature
A measure of average kinetic energy of particles. Normal human core temperature ranges from 36.1°C to 37.2°C (97°F to 99°F).
Heat
Energy transfer due to temperature differences. Heat always flows from higher to lower temperature regions.
Clinical Example: ICU Patient Monitoring
A critically ill patient in the ICU represents a complex thermodynamic system. Nurses monitor core temperature using thermodynamics principles, understanding that fever indicates increased metabolic heat production, while hypothermia suggests inadequate heat generation or excessive heat loss to the environment.
2. Laws of Thermodynamics
The laws of thermodynamics govern all energy interactions in healthcare settings. These fundamental principles explain metabolic processes, equipment function, and therapeutic interventions. Understanding thermodynamics laws enables nurses to predict patient responses and optimize care strategies.
| Law | Principle | Nursing Application |
|---|---|---|
| Zeroth Law | Thermal equilibrium and temperature measurement | Accurate thermometer readings require thermal equilibrium between device and patient |
| First Law | Energy conservation in closed systems | Caloric intake must balance metabolic expenditure for weight maintenance |
| Second Law | Entropy increase and heat flow direction | Heat flows from patient to cool environment; warming blankets reverse this flow |
| Third Law | Absolute zero temperature reference | Temperature scale standardization for precise medical measurements |
Key Point: First Law Application
The first law of thermodynamics states that energy cannot be created or destroyed, only transformed. In nursing practice, this explains why patients with increased metabolic demands (fever, infection, trauma) require additional caloric intake to maintain energy balance and prevent catabolism.
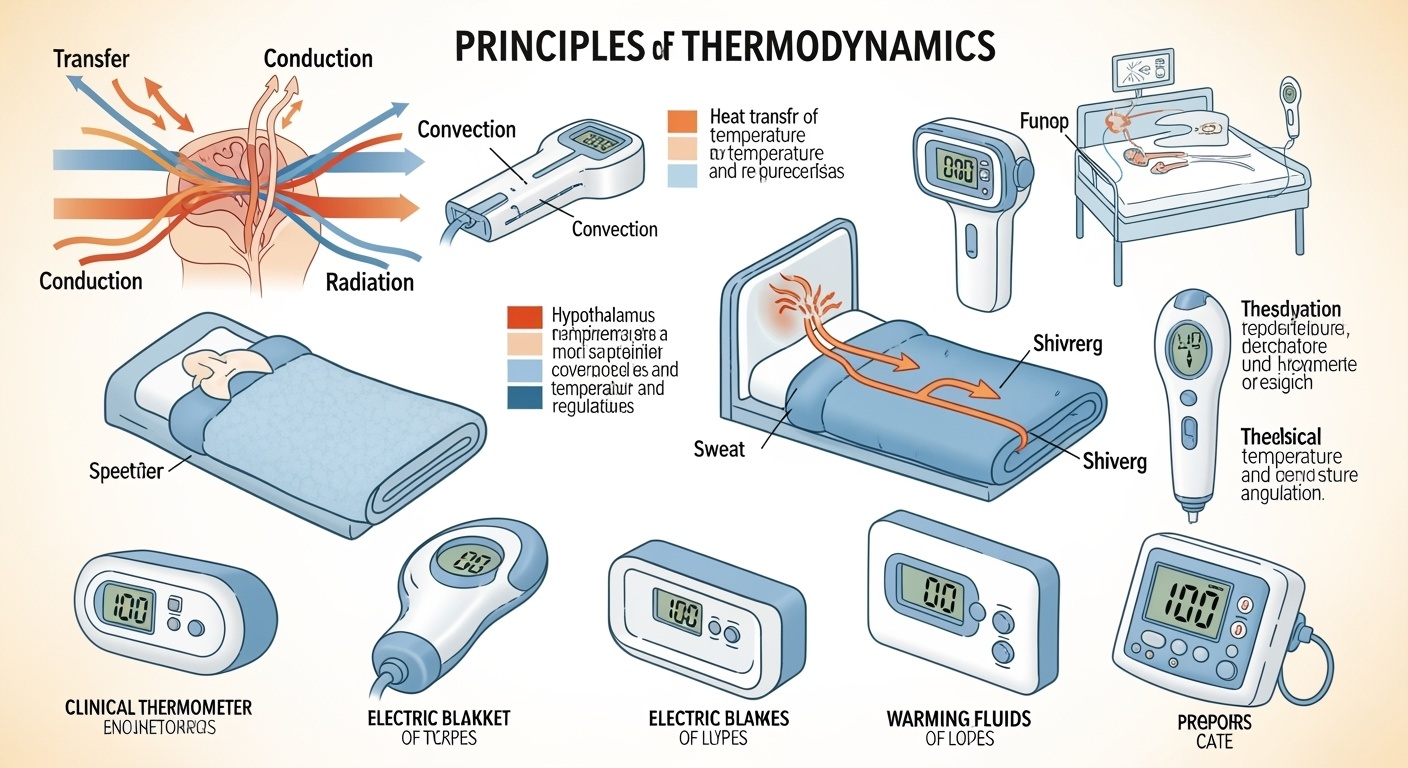
3. Heat Transfer Mechanisms
Heat transfer mechanisms determine how patients gain or lose thermal energy. Nurses utilize thermodynamics principles to implement effective temperature management interventions. Understanding these mechanisms enables precise control of patient thermal comfort and therapeutic outcomes.
Conduction
Direct heat transfer through physical contact between objects at different temperatures.
Convection
Heat transfer through fluid movement, including air and liquid circulation.
Radiation
Electromagnetic energy transfer without direct contact or medium.
Clinical Application: Surgical Hypothermia Prevention
Operating rooms utilize all three heat transfer mechanisms in thermodynamics applications:
- Conduction: Warming mattresses transfer heat directly to patient’s body
- Convection: Forced-air warming systems circulate heated air around patient
- Radiation: Overhead radiant heaters warm patient without contact
4. Body Temperature Regulation
Human thermoregulation represents a sophisticated application of thermodynamics principles. The hypothalamus functions as a biological thermostat, maintaining core temperature through complex feedback mechanisms. Nurses must understand these thermodynamics processes to assess and support patient temperature regulation effectively.
Thermoregulatory Mechanisms
Heat Production
- Cellular metabolism (primary source)
- Muscle contraction and shivering
- Brown adipose tissue thermogenesis
- Hormonal regulation (thyroid, epinephrine)
Heat Loss
- Skin vasodilation and vasoconstriction
- Sweating and evaporation
- Respiratory heat exchange
- Behavioral adaptations
| Temperature Range | Classification | Thermodynamics Response | Nursing Implications |
|---|---|---|---|
| < 35°C (95°F) | Hypothermia | Excessive heat loss exceeds production | Active rewarming protocols, monitor for complications |
| 36.1-37.2°C (97-99°F) | Normal Range | Heat production equals heat loss | Maintain thermal comfort, routine monitoring |
| 37.3-38.0°C (99.1-100.4°F) | Low-grade Fever | Increased heat production | Investigate underlying cause, comfort measures |
| > 38°C (100.4°F) | Fever | Significantly increased heat production | Antipyretic therapy, cooling measures, hydration |
5. Clinical Applications of Thermodynamics
Thermodynamics principles guide numerous clinical interventions and equipment applications in healthcare. Nurses apply these concepts daily through temperature monitoring, therapeutic hypothermia, hyperthermia treatment, and equipment operation. Understanding thermodynamics enhances clinical decision-making and patient outcomes.
Temperature Monitoring
Accurate temperature measurement relies on thermodynamics principles, requiring thermal equilibrium between measuring device and patient.
Therapeutic Hypothermia
Controlled cooling applications in thermodynamics protocols for neuroprotection and cardiac arrest management.
Emergency Application: Heat Stroke Management
Heat stroke represents a thermodynamics emergency where heat production and environmental heat gain overwhelm the body’s cooling mechanisms. Immediate nursing interventions include:
- Aggressive cooling using conduction (ice packs to major vessels)
- Convection cooling with fans and misting
- Cold intravenous fluid administration
- Continuous core temperature monitoring
- Prevention of overcooling and shivering
6. Evidence-Based Nursing Interventions
Nursing interventions based on thermodynamics principles improve patient comfort, prevent complications, and support healing. These evidence-based practices demonstrate the practical application of thermodynamics theory in clinical nursing care across various healthcare settings.
Perioperative Temperature Management
Surgical patients face significant thermodynamics challenges due to anesthesia effects, exposure, and altered metabolism.
Preoperative
- • Baseline temperature assessment
- • Prewarming protocols
- • Risk factor identification
Intraoperative
- • Forced-air warming systems
- • Warmed intravenous fluids
- • Environmental controls
Postoperative
- • Continuous monitoring
- • Gradual rewarming protocols
- • Complication prevention
Neonatal Thermodynamics Care
Newborns require specialized thermodynamics management due to immature thermoregulation, high surface area to body mass ratio, and limited subcutaneous fat.
| Intervention | Thermodynamics Principle | Expected Outcome |
|---|---|---|
| Skin-to-skin contact | Conductive heat transfer | Maintained normothermia |
| Radiant warmer | Radiative heat transfer | Controlled warming environment |
| Incubator care | Convective heat management | Stable thermal environment |
Best Practice: Thermodynamics Assessment
Comprehensive temperature assessment involves more than single-point measurements. Nurses should evaluate thermal patterns, patient comfort, environmental factors, and physiological responses to implement effective thermodynamics-based interventions.
7. Temperature-Related Disorders
Temperature disorders represent failures in thermodynamics regulation, requiring immediate nursing assessment and intervention. Understanding the pathophysiology through thermodynamics principles enables early recognition and appropriate management of these potentially life-threatening conditions.
Hyperthermia Spectrum
Heat Exhaustion
Core temperature 37-40°C; profuse sweating, weakness, nausea
Heat Stroke
Core temperature >40°C; altered mental status, anhidrosis
Malignant Hyperthermia
Genetic disorder; rapid temperature rise, muscle rigidity
Hypothermia Spectrum
Mild Hypothermia
32-35°C; shivering, confusion, loss of fine motor control
Moderate Hypothermia
28-32°C; decreased consciousness, cardiac arrhythmias
Severe Hypothermia
<28°C; unconsciousness, cardiac arrest risk
Critical Thermodynamics Emergency
Malignant hyperthermia represents a catastrophic failure of cellular thermodynamics, with temperatures rising 1-2°C every 5 minutes. Immediate nursing actions include:
- Discontinue triggering agents immediately
- Administer dantrolene sodium (specific antidote)
- Implement aggressive cooling measures
- Monitor cardiac rhythm and electrolytes
- Prepare for potential cardiac arrest
8. Thermodynamics Case Studies
Real-world case studies demonstrate the practical application of thermodynamics principles in nursing practice. These scenarios illustrate complex temperature management challenges and evidence-based solutions that nurses implement daily.
Case Study 1: Trauma Patient Hypothermia
Patient Presentation
22-year-old male, motor vehicle accident victim, presents with core temperature 34.2°C, altered mental status, and multiple injuries. Understanding thermodynamics reveals heat loss through exposed wounds, cold IV fluids, and environmental exposure.
Thermodynamics Analysis
- • Conductive heat loss to cold surfaces
- • Convective heat loss through air circulation
- • Evaporative heat loss from open wounds
- • Reduced heat production due to shock
Nursing Interventions
- • Remove wet clothing
- • Apply forced-air warming blanket
- • Warm all IV fluids to 37°C
- • Cover head and extremities
- • Monitor core temperature continuously
- • Adjust rewarming rate (1-2°C/hour)
- • Assess for rewarming complications
Case Study 2: Post-Cardiac Arrest Cooling
Clinical Scenario
58-year-old female, successful resuscitation from ventricular fibrillation cardiac arrest. Target temperature management protocol initiated using thermodynamics principles for neuroprotection.
Temperature Management Goals
- • Target temperature: 33°C for 24 hours
- • Controlled rewarming: 0.25°C/hour
- • Prevent temperature overshoot
- • Monitor for shivering response
Thermodynamics Protocol
- • Surface cooling with gel pads
- • Cold saline infusion (4°C)
- • Sedation to prevent shivering
- • Continuous temperature monitoring
- • Gradual temperature increase
- • Electrolyte monitoring
- • Neurological assessments
- • Prevent temperature rebound
Outcomes Assessment
Both cases demonstrate successful application of thermodynamics principles in nursing care. Key outcome measures include:
- • No complications from temperature extremes
- • Prevented secondary injuries
- • Achieved target temperatures
- • Optimized recovery potential
- • Evidence-based practice adherence
- • Reduced length of stay
Key Takeaways
Essential Concepts
- Thermodynamics governs all energy transfer in healthcare
- Heat transfer mechanisms guide nursing interventions
- Temperature regulation involves complex feedback systems
- Evidence-based protocols improve patient outcomes
Clinical Applications
- Accurate temperature assessment and monitoring
- Effective thermal management strategies
- Prevention and treatment of temperature disorders
- Optimization of patient comfort and safety
