Comprehensive Nursing Guide to Thumb Sucking in Children
An evidence-based approach to identification, diagnosis, and management of thumb sucking behaviors
Table of Contents
1. Introduction to Thumb Sucking in Children
Thumb sucking in children is a common behavior that can be categorized under non-nutritive sucking habits. Within this group, we also find the use of pacifiers, blankets, or sucking on other fingers as comforting behaviors. Thumb sucking serves as an adaptive function by providing stimulation or self-soothing for young children.
Key Points:
- Non-nutritive sucking habits are common in young children
- Most children stop thumb sucking spontaneously between ages 2-4
- Thumb sucking beyond age 4-5 may require intervention
- Prolonged thumb sucking can lead to dental and psychological issues
As nursing professionals, understanding thumb sucking in children is essential for providing appropriate guidance to parents and implementing effective interventions when necessary. This comprehensive guide will equip nursing students with the knowledge and tools needed for assessment, diagnosis, and management of thumb sucking behaviors across various settings.
Nursing Consideration:
The approach to thumb sucking should be developmentally appropriate and consider both the physical and psychological aspects of the behavior. Early intervention focuses on prevention and education, while later interventions may require more structured approaches.
2. Identification & Diagnosis of Thumb Sucking in Children
Identifying and properly diagnosing thumb sucking in children requires a comprehensive assessment that considers the frequency, intensity, and duration of the behavior. Early recognition allows for timely intervention when necessary.
Clinical Assessment
| Assessment Area | Findings | Nursing Implications |
|---|---|---|
| Physical Examination |
– Calluses or blisters on thumb – Skin irritation or maceration – Nail deformities – Finger/thumb hygiene issues |
Document severity and appearance of physical changes; assess if complications like paronychia are present |
| Oral Examination |
– Anterior open bite – Protrusion of upper incisors – Retroclination of lower incisors – Changes in palate structure |
Note dental alignment issues; consider dental consultation for children over 4 years with persistent habit |
| Behavioral Assessment |
– Frequency (occasional vs. constant) – Intensity (passive vs. vigorous) – Trigger situations (stress, fatigue, etc.) – Age-appropriateness |
Determine if the behavior is developmentally appropriate or requires intervention |
| Psychosocial Factors |
– Anxiety or stress indicators – Comfort-seeking patterns – Self-regulation abilities – Parent-child interactions |
Assess underlying psychological factors that may contribute to persistent thumb sucking |
Diagnostic Criteria:
When evaluating thumb sucking in children, consider the following diagnostic parameters:
- Normal (Requires Monitoring): Thumb sucking in children under 4 years, occasional, self-limiting
- Concerning (May Require Intervention): Thumb sucking that continues after 4 years of age, especially during waking hours
- Problematic (Requires Intervention): Thumb sucking after 5 years, causes dental changes, affects speech, or causes social issues
Diagnostic Tools
- Behavior Frequency Chart: Parents record instances of thumb sucking throughout the day
- Functional Assessment: Identifies triggers and maintaining factors
- Dental Evaluation: Assesses impact on dentition and oral structures
- Developmental Assessment: Places behavior in context of overall development
Differential Considerations
- Self-Soothing: Normal developmental behavior
- Anxiety: May indicate emotional distress
- Habit: Continues beyond self-soothing purpose
- Oral Fixation: May be related to inadequate oral stimulation during development
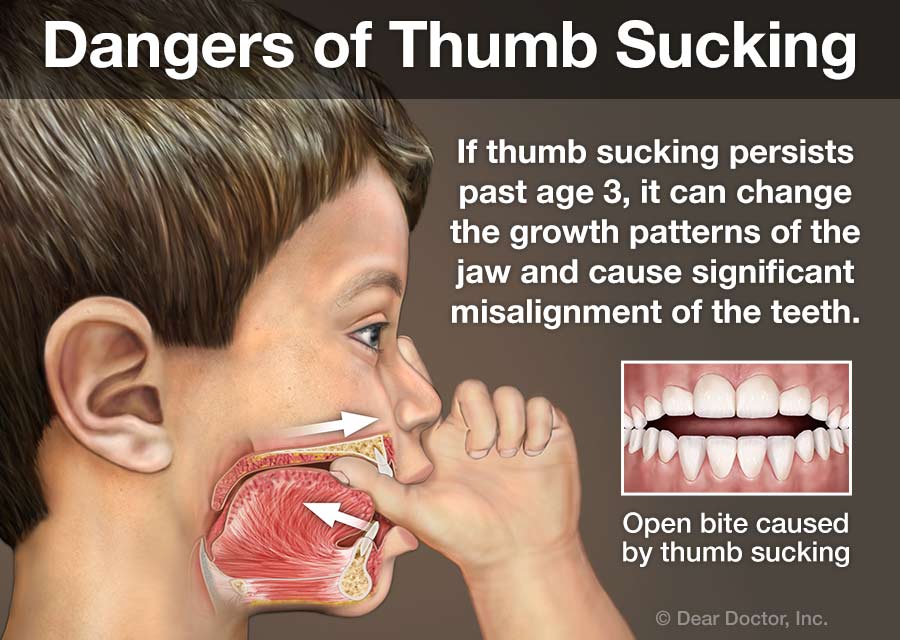
Figure 1: Dental effects of prolonged thumb sucking showing anterior open bite and dental malocclusion
Nursing Tip:
When assessing thumb sucking in children, avoid making the child feel ashamed or criticized. Approach the assessment with curiosity and a non-judgmental attitude to get accurate information from both the child and parents.
3. Etiology & Risk Factors of Thumb Sucking in Children
Understanding the causes and risk factors associated with thumb sucking in children helps nurses formulate targeted interventions and provide appropriate guidance to families.
Developmental Factors
- Innate Sucking Reflex: Present before birth and persists in early infancy
- Oral Satisfaction: Sucking provides pleasure and comfort
- Self-Soothing: Helps babies and young children regulate emotions
- Transitional Object: Thumb becomes a self-controlled comfort object
Psychological Factors
- Anxiety & Stress: Increases during periods of emotional distress
- Security & Comfort: Provides reassurance in unfamiliar situations
- Boredom: May increase during periods of inactivity
- Sleep Association: Often linked to falling asleep
Risk Factors for Persistent Thumb Sucking
| Risk Factor | Description | Evidence Level |
|---|---|---|
| Insufficient Breastfeeding | Research suggests that shorter breastfeeding duration is associated with higher likelihood of thumb sucking behavior | Moderate |
| Family Stress | Children in high-stress home environments may continue thumb sucking as a coping mechanism | Moderate |
| Psychological Disposition | Children with anxious temperaments may be more likely to continue the habit | Moderate |
| Parental Reinforcement | Excessive attention to the behavior (positive or negative) may inadvertently reinforce it | High |
| Genetic Factors | Some studies suggest a genetic predisposition to oral habits | Low |
The T.H.U.M.B. Mnemonic for Understanding Causes
T – Transitional developmental phase (normal in young children)
H – Habit formation through repeated behavior
U – Unmet oral needs (including insufficient nursing/feeding)
M – Mood regulation and emotional comfort
B – Boredom or inadequate stimulation
Critical Thinking Alert:
When assessing thumb sucking in children, avoid making assumptions about parenting quality. Many well-parented children engage in thumb sucking as a self-soothing behavior. Focus instead on understanding the specific triggers and functions the behavior serves for each individual child.
4. Effects & Complications of Thumb Sucking in Children
Prolonged thumb sucking in children, particularly beyond the age of 4-5 years, can lead to various physical, dental, and psychosocial complications. Understanding these potential effects helps nurses educate families and prioritize interventions.
The D.A.M.P. Thumb Mnemonic for Complications
D – Dental problems & Digital deformity
A – Anterior open bite & Altered growth of facial bones
M – Mucosal injury & decreased alveolar bone growth
P – Paronychia & Psychological sequelae
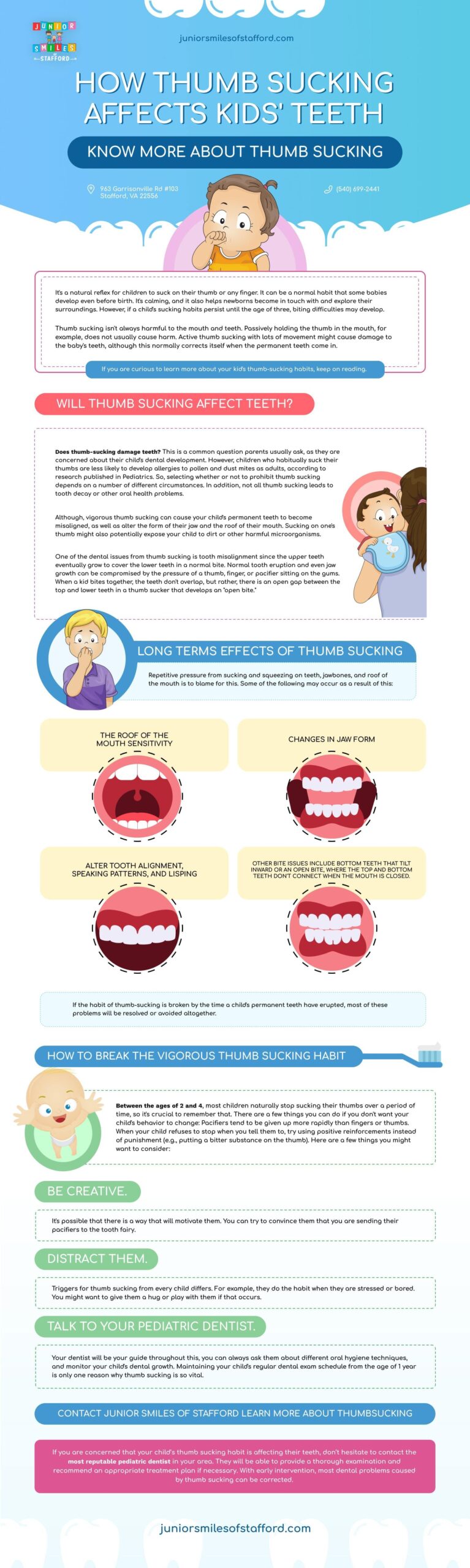
Figure 2: Various dental and oral effects of prolonged thumb sucking behavior
Physical & Dental Complications
| Complication | Description | Nursing Assessment Points |
|---|---|---|
| Anterior Open Bite | Space between upper and lower front teeth when back teeth are closed | Observe for gap between front teeth; difficulty biting into food; may affect speech |
| Malocclusion | Protrusion of upper incisors; retroclination of lower incisors | Note “buck teeth” appearance; assess impact on eating and speech |
| Palatal Changes | Narrowing of upper dental arch; high-arched palate | May contribute to crossbite or other occlusal problems |
| Digital Deformities | Flattening or deformity of the thumb; nail changes | Examine thumb for widening, flattening, or nail deformities |
| Skin Problems | Callus formation; maceration; paronychia (infection around nail) | Assess for redness, inflammation, or infection of thumb |
Psychosocial & Developmental Impacts
Potential Negative Impacts
- Social Stigma: Peer teasing or rejection in older children
- Self-Esteem Issues: Embarrassment about the habit or appearance
- Speech Problems: Articulation difficulties related to dental changes
- Dependency: Overreliance on self-soothing rather than developing other coping skills
Positive Aspects to Consider
- Self-Regulation: Helps children manage emotions independently
- Stress Relief: Provides comfort during difficult transitions
- Sleep Aid: May facilitate self-soothing to sleep
- Autonomy: Represents child’s control over their comfort
Nursing Consideration:
When educating families about thumb sucking in children, balance information about potential complications with an acknowledgment of the self-soothing benefits. Focus intervention efforts on children over 4-5 years of age when dental and social impacts become more significant.
5. Nursing Management of Thumb Sucking in Children in Hospital Settings
When caring for children in hospital settings, nurses may encounter thumb sucking in children as either a primary concern or, more commonly, as a comfort behavior during hospitalization. A thoughtful, evidence-based approach is essential.
Nursing Process for Thumb Sucking in Hospital Settings
| Nursing Process Step | Interventions for Thumb Sucking |
|---|---|
| Assessment |
– Comprehensive assessment of thumb sucking pattern and history – Evaluate for complications (dental, skin, psychological) – Identify triggers in hospital environment – Assess parental concerns and management strategies – Document baseline frequency/intensity of behavior |
| Nursing Diagnosis |
– Risk for impaired oral mucous membrane related to thumb sucking – Risk for infection related to thumb sucking – Ineffective coping related to excessive reliance on thumb sucking – Anxiety related to hospitalization manifested by increased thumb sucking – Deficient knowledge (parental) regarding management of thumb sucking |
| Planning |
– Set appropriate goals based on child’s age and developmental level – Collaborate with parents on consistent approach – Plan interventions that address underlying causes – Consider hospital-specific stressors that may increase behavior – Coordinate with multidisciplinary team if needed (Child Life, dental) |
| Implementation |
– Provide alternative comfort measures during stressful procedures – Implement hand hygiene protocol to prevent infection – Offer age-appropriate distraction activities – Teach parents positive reinforcement techniques – Document interventions and child’s response – Provide emotional support during hospitalization |
| Evaluation |
– Monitor for changes in frequency/intensity of thumb sucking – Assess effectiveness of interventions – Evaluate for complications – Adjust plan as needed – Prepare discharge teaching if thumb sucking is a concern |
Special Considerations in Hospital Settings:
- Infection Control: Frequent hand hygiene is essential to prevent infection transmission through thumb sucking
- IV Management: For children with IV lines, increased monitoring may be needed to prevent displacement
- Procedural Support: Thumb sucking may increase during painful procedures; provide alternative comfort measures
- Regression: Hospitalized children may temporarily increase thumb sucking due to stress
- Medication Considerations: Monitor for oral medications that might interact with thumb sucking (taste, absorption)
Documentation Guidelines
What to Document
- Frequency, duration, and intensity of thumb sucking
- Associated triggers observed in hospital
- Physical assessment findings (oral, digital)
- Interventions implemented and effectiveness
- Parental involvement and teaching provided
- Changes in behavior over hospitalization
Sample Documentation
“5-year-old observed sucking thumb during IV insertion and when parents leave room. No signs of skin breakdown or infection on right thumb. Parents report thumb sucking has increased since hospitalization. Child Life Specialist provided distraction techniques and comfort items. Parents educated on positive reinforcement strategies. Will continue to monitor and support during stressful procedures.”
Hospital Nursing Tip:
For hospitalized children with persistent thumb sucking, focus on infection prevention rather than habit elimination. The hospital setting is not an ideal time to address long-term behavior change unless specifically admitted for this purpose. Instead, support the child’s coping mechanisms while ensuring safety and hygiene.
6. Nursing Management of Thumb Sucking in Children at Home
Community health nurses and home visiting nurses play a crucial role in helping families address thumb sucking in children within the home environment. Home-based interventions offer the opportunity for customized approaches that fit the family’s routine and values.
Assessment in Home Setting
- Environmental Assessment: Identify home-specific triggers for thumb sucking
- Routine Analysis: Determine when thumb sucking occurs most frequently
- Family Dynamics: Observe how family members respond to the behavior
- Previous Attempts: Evaluate strategies the family has already tried
- Cultural Factors: Consider cultural perspectives on the behavior
Family Education Topics
- Normal Development: When thumb sucking is developmentally appropriate
- Potential Complications: Age-appropriate information on risks
- Positive Approaches: Non-punitive intervention strategies
- Consistency: Importance of consistent approach among caregivers
- Realistic Expectations: Timeline for behavior change
Home-Based Intervention Strategies
| Intervention Category | Specific Strategies | Nursing Support |
|---|---|---|
| Environmental Modification |
– Create thumb-free zones in the home – Provide fidget toys or alternative comfort items – Use visual reminders in key locations – Set up reward system with tracking chart |
Help family identify key locations for modifications; assist in creating age-appropriate visual cues and reward systems |
| Routine Adjustments |
– Establish consistent sleep routine that doesn’t rely on thumb sucking – Plan engaging activities during common thumb-sucking times – Create transition rituals that occupy hands – Schedule regular “check-in” times with child |
Review daily schedule with family; identify critical intervention points; develop substitute routines that promote self-regulation |
| Positive Reinforcement |
– Calendar with stickers for thumb-free periods – Celebration of incremental progress – Non-food rewards for meeting goals – Verbal praise for alternative coping strategies |
Teach parents effective praise techniques; help set realistic goals; create developmentally appropriate reward systems |
| Gentle Reminders |
– Non-verbal signals between parent and child – Use of stories or puppets to discuss the habit – Timer-based reminder system – Special “reminder” bracelet or sticker |
Demonstrate non-shaming reminder techniques; provide resources for age-appropriate stories; role-play conversations |
| Physical Aids (if appropriate) |
– Thumb guards or mittens for sleep (older children) – Bitter-tasting applications (with caution) – Adhesive bandages as reminders – Special “thumb glove” to prevent sucking |
Discuss appropriate use of physical aids; ensure safety; monitor for skin irritation or emotional distress; emphasize these as temporary measures |

Figure 3: Visual guide to thumb sucking intervention strategies for home implementation
The P.A.R.E.N.T. Approach for Home Management
P – Positive reinforcement for non-thumb-sucking periods
A – Alternatives that provide similar comfort (stuffed animals, sensory toys)
R – Routine adjustments to minimize triggers
E – Environment modifications that support habit change
N – Non-judgmental reminders and encouragement
T – Time and patience with the process of change
Home Care Warning:
Advise parents against punitive approaches to thumb sucking in children, such as harsh criticism, physical restraint, or humiliation. These can cause psychological distress and may actually increase the behavior due to anxiety. Focus instead on positive reinforcement and addressing underlying needs.
7. Control Strategies for Thumb Sucking in Children
When thumb sucking in children persists beyond the appropriate developmental stage, various control strategies may be implemented. The selection of appropriate interventions should be based on the child’s age, the severity of the habit, and potential complications.
Age-Appropriate Intervention Approach
| Age Group | Recommended Approach | Inappropriate Interventions |
|---|---|---|
| 0-2 years |
– Consider normal developmental behavior – No intervention typically needed – Focus on adequate breastfeeding/feeding – Provide appropriate oral stimulation |
– Physical restraints – Bitter applications – Punitive measures – Constant reminders |
| 3-4 years |
– Begin gentle discussion about the habit – Use positive reinforcement – Read children’s books about thumb sucking – Monitor for dental changes |
– Shaming tactics – Harsh physical barriers – Excessive attention to the behavior – Inconsistent approaches |
| 5-6 years |
– Active intervention appropriate – Child involvement in decision-making – Reward systems – Consider dental consultation – Gentle reminder systems |
– Public embarrassment – Forced compliance – Comparison to other children – Punishments for slips |
| 7+ years |
– More structured intervention – Behavioral contracts – Dental appliances if indicated – Cognitive-behavioral techniques – Address any underlying emotional issues |
– Treating as willful misbehavior – Ignoring potential psychological factors – Extreme measures without professional guidance – Focusing only on the habit, not the child |
Evidence-Based Intervention Hierarchy
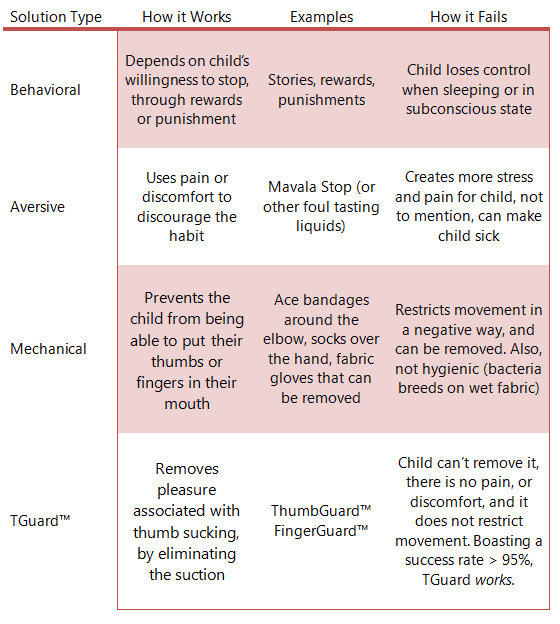
Figure 4: Comparison of treatment options for thumb sucking habit management
First-Line Approaches
- Positive Reinforcement: Reward systems, praise for non-sucking periods
- Awareness Training: Helping child recognize when the behavior occurs
- Environmental Modifications: Reducing triggers, providing alternatives
- Parent Education: Understanding development and appropriate expectations
- Motivational Strategies: Age-appropriate goal setting with child involvement
Second-Line Approaches
- Reminder Devices: Thumb guards, adhesive bandages, “thumb gloves”
- Habit Reversal Training: Teaching competing responses
- Bitter Applications: With caution and appropriate monitoring
- Behavioral Contracts: Formal agreements with older children
- Professional Counseling: For persistent cases with emotional components
Technique Spotlight: Habit Reversal Training
Habit Reversal Training (HRT) is an evidence-based approach for thumb sucking in children who are old enough to actively participate in their treatment. It involves:
- Awareness Training: Teaching the child to recognize when they are engaging in thumb sucking
- Competing Response Training: Practicing an incompatible action (like making a fist or gripping an object)
- Motivation Procedures: Creating a rewarding environment for practicing the new response
- Generalization Training: Applying the skills across different settings and situations
Nursing Role: Teach parents HRT techniques; model implementation; monitor progress; adjust as needed.
Interprofessional Approach
| Healthcare Professional | Role in Thumb Sucking Management |
|---|---|
| Pediatric Nurse | Assessment, family education, behavioral management strategies, monitoring progress, coordinating care |
| Primary Care Provider | Regular screening, ruling out medical concerns, referrals to specialists when needed |
| Pediatric Dentist | Evaluation of dental impacts, oral appliances when indicated, monitoring for complications |
| Child Psychologist | Assessment of underlying psychological factors, behavioral therapy, family counseling for persistent cases |
| Speech Therapist | Evaluation and treatment of speech issues related to dental changes, oral-motor exercises |
Nursing Success Strategy:
When implementing control strategies for thumb sucking in children, focus on one setting at a time (e.g., while watching TV first, then at bedtime). Gradual success is more sustainable than attempting to eliminate the behavior in all situations simultaneously.
8. Case Studies on Thumb Sucking in Children
The following case studies illustrate real-world scenarios of thumb sucking in children and effective nursing approaches to management. These examples demonstrate the application of evidence-based strategies in different contexts.
Case Study 1: Preschool Child (Age 3.5)
Presentation: Maya, a 3.5-year-old girl, sucks her thumb primarily during naptime, bedtime, and when watching television. Parents are concerned about potential dental problems but unsure if intervention is needed at this age.
Nursing Assessment:
- Developmental assessment shows age-appropriate milestones
- No dental malocclusion noted during oral examination
- Thumb appears healthy with no skin breakdown
- Behavior primarily occurs during rest/quiet times
- Parents report normal social adjustment with peers
Nursing Interventions:
- Educated parents on normal developmental aspects of thumb sucking at this age
- Provided reassurance that intervention is not urgently needed
- Discussed gentle approaches to limit thumb sucking during TV time
- Recommended children’s books about thumb sucking
- Advised regular dental monitoring
Outcome: Parents implemented a “special toy” that Maya could hold during TV time, which reduced thumb sucking in that context. They decided not to address bedtime thumb sucking at this point, understanding it was developmentally appropriate. Plan to reassess at age 4-4.5 years.
Case Study 2: School-Age Child (Age 6)
Presentation: Ethan, a 6-year-old boy, has been thumb sucking since infancy. He sucks his thumb constantly, including at school, leading to teasing from classmates. Dental examination shows beginning anterior open bite. Parents have tried verbal reminders and bitter nail polish without success.
Nursing Assessment:
- Thumb shows callus formation and mild nail deformity
- Dental changes noted (anterior open bite developing)
- Assessment reveals thumb sucking increases during anxiety-provoking situations
- Child expresses desire to stop but says “I can’t help it”
- Parents using inconsistent approaches and showing frustration
Nursing Interventions:
- Implemented habit awareness training with Ethan
- Designed reward chart with attainable goals (thumb-free periods)
- Introduced competing response training (squeezing a stress ball)
- Taught parents positive reinforcement techniques
- Coordinated with school nurse for consistent approach
- Referred to pediatric dentist for evaluation
Outcome: After 8 weeks of consistent implementation, Ethan reduced daytime thumb sucking by approximately 70%. Nighttime thumb sucking persisted, and parents opted for a thumb guard during sleep. After 6 months, thumb sucking was limited to occasional episodes during high stress. Dental monitoring continues.
Case Study 3: Hospital Setting (Age 4)
Presentation: Lily, a 4-year-old girl, is hospitalized for pneumonia. Nurses observe constant thumb sucking, which increases during procedures and when parents leave. IV placed in non-dominant hand; thumb sucking occurs with dominant hand.
Nursing Assessment:
- Thumb sucking appears to be stress response to hospitalization
- No prior concerns reported by parents; primarily at bedtime at home
- Infection control concerns in hospital environment
- Child appears anxious about medical procedures
Nursing Interventions:
- Implemented frequent hand hygiene protocol
- Provided alternative comfort measures (favorite toy, music)
- Scheduled Child Life Specialist visits before procedures
- Created predictable routine to reduce anxiety
- Educated parents about temporary increase in self-soothing behaviors
Outcome: Focus remained on infection prevention rather than habit elimination during hospitalization. Thumb sucking decreased as Lily became more comfortable in the hospital environment. Parents reported return to baseline thumb-sucking pattern (bedtime only) after discharge home.
Case Study Learning Points:
- Tailor interventions to the child’s developmental level and specific situation
- Consider context (hospital vs. home) when determining intervention priorities
- Involve the child in the process when developmentally appropriate
- Address underlying triggers rather than just the behavior itself
- Set realistic expectations and celebrate incremental progress
9. Resources & References
Parent Education Resources
Recommended Books for Children
- “David Decides About Thumbsucking” by Susan Heitler
- “Thumbs Up, Brown Bear” by Michael Dahl
- “No More Thumb Sucking” by Jane Moncure
- “Binkle and the Thumb Sucking Solution” by Dianne Warren
- “Thumbs Are for Picking and Strumming” by Harriet Ziefert
Parent Handouts & Resources
- American Academy of Pediatric Dentistry guides
- HealthyChildren.org (AAP) resources on thumb sucking
- Habit tracking charts (downloadable templates)
- Reward system examples for positive reinforcement
- FAQ sheets addressing common parent concerns
Professional Resources for Nurses
| Resource Type | Description |
|---|---|
| Clinical Guidelines |
– American Academy of Pediatrics recommendations – American Academy of Pediatric Dentistry position statements – Evidence-based nursing protocols for habit management |
| Assessment Tools |
– Thumb sucking frequency monitoring forms – Functional behavior assessment templates – Dental impact evaluation tools |
| Patient Education |
– Age-appropriate teaching materials – Family education handouts in multiple languages – Visual aids for explaining dental impacts |
| Continuing Education |
– Pediatric behavior management courses – Child development resources – Positive reinforcement training modules |
References
- Borrie FR, Bearn DR, Innes NP, Iheozor-Ejiofor Z. (2015). Interventions for the cessation of non-nutritive sucking habits in children. Cochrane Database Syst Rev, 2015(3):CD008694.
- Kumar V, Shivanna V, Kopuri RC. (2019). Knowledge and attitude of pediatricians toward digit sucking habit in children. J Indian Soc Pedod Prev Dent, 37(1):18-24.
- Nasir A, Nasir L. (2015). Counseling on Early Childhood Concerns: Sleep Issues, Thumb-Sucking, Picky Eating, School Readiness, and Oral Health. Am Fam Physician, 92(4):274-8.
- Majorana A, Bardellini E, Amadori F, Conti G, Polimeni A. (2015). Timetable for oral prevention in childhood–developing dentition and oral habits: a current opinion. Prog Orthod, 16:39.
- Tanaka O, Oliveira W, Galarza M, Aoki V, Bertaiolli B. (2016). Breaking the Thumb Sucking Habit: When Compliance Is Essential. Case Rep Dent, 2016:6010615.
- Lopes Freire GM, Espasa Suarez de Deza JE, Rodrigues da Silva IC, Butini Oliveira L, Ustrell Torrent JM, Boj Quesada JR. (2016). Non-nutritive sucking habits and their effects on the occlusion in the deciduous dentition in children. Eur J Paediatr Dent, 17(4):301-306.
- Baker E, Masso S, McLeod S, Wren Y. (2018). Pacifiers, Thumb Sucking, Breastfeeding, and Bottle Use: Oral Sucking Habits of Children with and without Phonological Impairment. Folia Phoniatr Logop, 70(3-4):165-173.
- Krishnappa S, Rani MS, Aariz S. (2016). New electronic habit reminder for the management of thumb-sucking habit. J Indian Soc Pedod Prev Dent, 34(3):294-7.
- Tanny L, Huang B, Naung NY, Currie G. (2018). Non-orthodontic intervention and non-nutritive sucking behaviours: A literature review. Kaohsiung J Med Sci, 34(4):215-222.
- American Academy of Pediatrics. (2020). Pacifiers and Thumb Sucking. HealthyChildren.org. Retrieved from https://www.healthychildren.org/English/ages-stages/baby/crying-colic/Pages/Pacifiers-and-Thumb-Sucking.aspx
Nursing Knowledge Update:
This guide to thumb sucking in children reflects current evidence as of its creation. Nursing professionals should continue to monitor for updated guidelines and emerging research in this area, particularly regarding long-term impacts and innovative intervention strategies.
