Thyroid Diseases in Community
A Comprehensive Guide for Nursing Students
Table of Contents
Introduction to Thyroid Disorders
Thyroid disorders represent a significant public health challenge globally, affecting millions of people across all demographics. The thyroid gland, a butterfly-shaped organ located in the neck, produces hormones that regulate metabolism, growth, and development. When this gland functions abnormally, it leads to various thyroid disorders that impact multiple body systems.
Community health nurses play a pivotal role in the early detection, management, and follow-up care of individuals with thyroid disorders. Their involvement spans from community screening programs to patient education, medication management, and long-term monitoring of thyroid conditions.
Public Health Significance of Thyroid Disorders:
- Affects approximately 200 million people worldwide
- Many cases remain undiagnosed due to subtle symptoms
- Untreated thyroid disorders can lead to serious complications including cardiovascular disease, osteoporosis, and developmental issues
- Preventable through early detection and management
- Requires coordinated community-based approaches for effective management
Epidemiology of Thyroid Diseases
Global Prevalence
Thyroid disorders affect approximately 5-10% of the global population, with significant regional variations. Iodine deficiency remains the most common cause of thyroid disorders worldwide, affecting nearly 2 billion people globally.
Age and Gender Distribution
Thyroid disorders show a marked gender disparity, affecting women 5-8 times more frequently than men. The prevalence increases with age, with peak incidence between 30-50 years. Subclinical hypothyroidism affects up to 10% of women over 60 years of age.
Regional Variations
The prevalence of specific thyroid disorders varies significantly by geographic region, largely influenced by dietary iodine intake, genetic factors, and environmental exposures.
Prevalence of Common Thyroid Disorders
| Thyroid Disorder | Global Prevalence | Key Demographics |
|---|---|---|
| Hypothyroidism | 4.6-9.5% | More common in women, especially >60 years |
| Hyperthyroidism | 1.2-1.6% | Peaks in 20-40 years, F:M ratio 5:1 |
| Thyroid Nodules | 4-7% | Increases with age, 50% by age 60 |
| Thyroid Cancer | ~2% of all cancers | Higher in women, increasing incidence |
| Iodine Deficiency | ~29% globally | Concentrated in developing regions |
Epidemiological Trends
- Rising Incidence: The detection of thyroid disorders has increased in recent decades, partly due to improved screening methods and awareness.
- Geographical Patterns: High prevalence of iodine deficiency disorders in mountainous regions and areas distant from seas.
- Socioeconomic Factors: Lower socioeconomic groups often have higher prevalence of iodine deficiency disorders due to limited access to iodized salt and healthcare.
- Thyroid Cancer: Rising incidence globally, particularly papillary thyroid cancer, though mortality rates remain stable.
Anatomy and Physiology of the Thyroid Gland
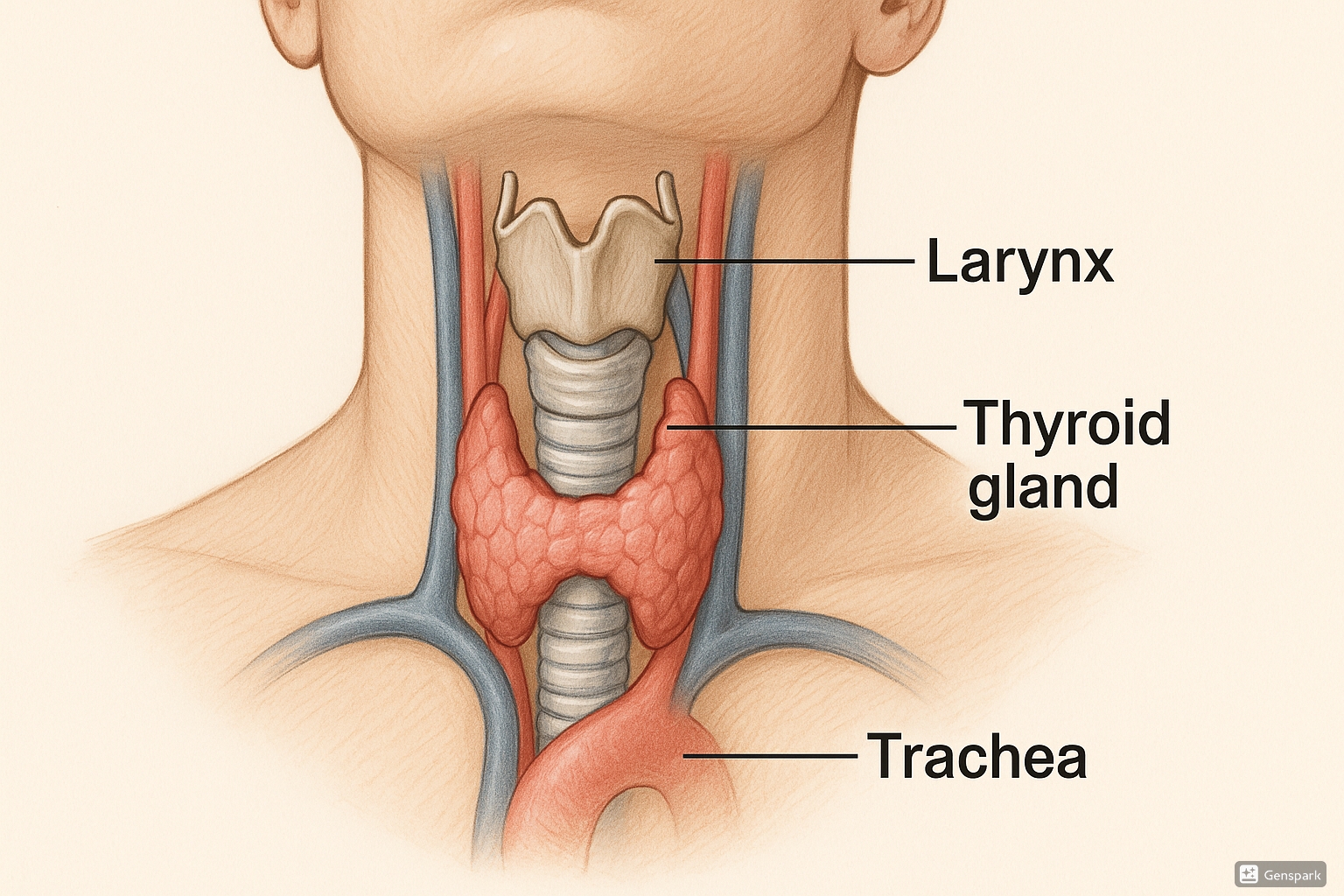
The thyroid gland is a bilobed endocrine organ located anteriorly in the neck, extending from the fifth cervical to the first thoracic vertebrae. It weighs approximately 15-20 grams in adults and consists of two lateral lobes connected by a thin isthmus that crosses anterior to the trachea.
Functional Anatomy
- Consists of spherical follicles lined by follicular cells
- Follicular cells produce thyroxine (T4) and triiodothyronine (T3)
- Parafollicular C cells produce calcitonin, which regulates calcium metabolism
- Highly vascular organ with extensive blood supply from superior and inferior thyroid arteries
Hormone Synthesis and Regulation
The synthesis of thyroid hormones requires iodine and involves several steps:
- Iodide trapping (active transport of iodide into follicular cells)
- Oxidation of iodide to iodine
- Iodination of tyrosine residues in thyroglobulin
- Coupling of iodotyrosines to form T3 and T4
- Storage in colloid
- Release into circulation in response to TSH stimulation
The Hypothalamic-Pituitary-Thyroid (HPT) Axis
Thyroid function is regulated through a negative feedback system involving:
Hypothalamus
Produces Thyrotropin-Releasing Hormone (TRH)
Anterior Pituitary
Produces Thyroid-Stimulating Hormone (TSH)
Thyroid Gland
Produces T3 and T4 hormones
Increased levels of T3 and T4 inhibit the production of TRH and TSH through negative feedback, maintaining hormone levels within normal ranges.
Types of Thyroid Disorders
Hypothyroidism
Hypothyroidism occurs when the thyroid gland produces insufficient thyroid hormones. It is one of the most common thyroid disorders worldwide.
Common Causes:
- Hashimoto’s thyroiditis (autoimmune)
- Iodine deficiency
- Post-surgical or radiation treatment
- Congenital hypothyroidism
- Medications (lithium, amiodarone)
Clinical Manifestations:
- Fatigue and lethargy
- Cold intolerance
- Weight gain
- Dry skin and hair
- Constipation
- Bradycardia
- Menstrual irregularities
- Cognitive impairment (“brain fog”)
Hyperthyroidism
Hyperthyroidism is characterized by excessive production of thyroid hormones, resulting in accelerated metabolism and hyperactivity of multiple organ systems.
Common Causes:
- Graves’ disease (autoimmune)
- Toxic nodular goiter
- Thyroiditis (transient)
- Excessive iodine intake
- Thyroid-stimulating hormone-secreting pituitary tumors
Clinical Manifestations:
- Weight loss despite increased appetite
- Heat intolerance and increased sweating
- Tachycardia and palpitations
- Tremors
- Anxiety and irritability
- Diarrhea
- Menstrual irregularities
- Exophthalmos (in Graves’ disease)
Thyroiditis
Inflammation of the thyroid gland that can cause either hyperthyroidism or hypothyroidism, depending on the stage and type.
Types:
- Hashimoto’s thyroiditis: Chronic autoimmune condition leading to hypothyroidism
- Subacute thyroiditis: Painful inflammation often following viral infection
- Postpartum thyroiditis: Occurs within one year after childbirth
- Silent thyroiditis: Painless inflammation with transient hyperthyroidism
Goiter and Nodules
Enlargement of the thyroid gland or development of nodules within the gland.
Types:
- Simple goiter: General enlargement without nodules, often due to iodine deficiency
- Multinodular goiter: Multiple nodules within the thyroid
- Solitary thyroid nodule: Single nodule requiring evaluation for malignancy
- Toxic nodular goiter: Nodules producing excess thyroid hormone
Thyroid Cancer
Malignant neoplasm of the thyroid gland, with several histological types varying in aggressiveness and prognosis.
Types:
- Papillary (80%): Most common, excellent prognosis
- Follicular (10%): Good prognosis
- Medullary (5-10%): Arises from C cells, moderate prognosis
- Anaplastic (1-2%): Aggressive with poor prognosis
Risk Factors:
- Radiation exposure (especially in childhood)
- Family history of thyroid cancer
- Genetic syndromes (MEN2, familial adenomatous polyposis)
- History of goiter or thyroid nodules
- Female gender
Mnemonic: “THYROID” for Common Thyroid Disorders
Thyroiditis
Hypothyroidism
Young adults (commonly affected)
Radiation effects
Overactivity (Hyperthyroidism)
Iodine deficiency
Diffuse goiter
Risk Factors for Thyroid Disorders
Non-Modifiable Risk Factors
Genetic Factors
- Family history of thyroid disorders increases risk by 2-8 times
- Specific genetic mutations (e.g., RET proto-oncogene for MTC)
- Genetic syndromes: Multiple Endocrine Neoplasia (MEN), Cowden syndrome
Age
- Incidence of thyroid disorders increases with age
- Hypothyroidism prevalence reaches 10% in women over 60
- Thyroid nodules present in >50% of individuals by age 60
Gender
- Women 5-8 times more likely to develop thyroid disorders
- Autoimmune thyroid diseases particularly more common in women
- Hormonal factors play significant role in gender disparity
Modifiable Risk Factors
Nutritional Factors
- Iodine deficiency or excess
- Selenium deficiency
- Consumption of goitrogenic foods (when excessive)
Environmental Exposures
- Radiation exposure (medical or environmental)
- Endocrine-disrupting chemicals
- Heavy metals exposure
- Certain medications (amiodarone, lithium)
Health Conditions
- Other autoimmune conditions (type 1 diabetes, rheumatoid arthritis)
- Pregnancy and postpartum period
- Chronic stress
- Smoking (Graves’ disease and ophthalmopathy)
High-Risk Populations for Thyroid Disorders
Community health nurses should be particularly vigilant for thyroid disorders in these high-risk groups:
- Women over 50 years of age
- Individuals with family history of thyroid disease
- Persons living in iodine-deficient areas
- Those with other autoimmune conditions
- Pregnant and postpartum women
- Individuals with history of radiation exposure to head/neck
- Elderly patients with unexplained fatigue, depression, or cognitive changes
Prevention and Control Measures for Thyroid Disorders
Primary Prevention
Measures aimed at preventing the occurrence of thyroid disorders in the population.
Key Strategies:
- Iodine supplementation: Universal salt iodization programs
- Education: Public awareness about thyroid health
- Radiation protection: Minimizing unnecessary radiation exposure
- Maternal nutrition: Adequate iodine intake during pregnancy and lactation
- Avoiding environmental toxins: Reducing exposure to endocrine disruptors
Secondary Prevention
Early detection and prompt intervention to minimize disease progression and complications.
Key Strategies:
- Screening programs: Targeting high-risk populations
- Case finding: Opportunistic assessment during routine healthcare
- Newborn screening: Early detection of congenital hypothyroidism
- Regular monitoring: For those with risk factors
- Thyroid self-examination: Teaching proper technique
Tertiary Prevention
Management strategies to reduce complications and improve quality of life for those with established thyroid disorders.
Key Strategies:
- Optimal treatment: Maintaining euthyroid state
- Regular monitoring: Preventing under or over-treatment
- Complication management: Early intervention for associated conditions
- Rehabilitation: Physical and psychological support
- Support groups: Peer support and education
Community-Based Control Measures
Public Health Programs
- Universal salt iodization programs
- Mass education campaigns about thyroid health
- Integration of thyroid screening in primary healthcare
- School-based education and screening initiatives
- Surveillance systems for monitoring iodine status
Role of Community Health Nurses
- Health education and promotion activities
- Risk assessment and early identification
- Facilitating community screening programs
- Medication adherence support
- Follow-up coordination for detected cases
- Lifestyle modification counseling
Mnemonic: “PREVENT” for Thyroid Disorder Prevention
Proper iodine intake
Radiation protection
Education about thyroid health
Vigilant screening
Environmental toxin avoidance
Nutritional adequacy
Treatment adherence
Screening and Diagnosis of Thyroid Disorders
Screening Approaches
While universal screening for thyroid disorders is not recommended in most countries, targeted screening of high-risk groups is an effective strategy for early detection.
Recommended Screening Populations:
- Newborns (universal screening for congenital hypothyroidism)
- Pregnant women and those planning pregnancy
- Adults over 60 years, especially women
- Individuals with family history of thyroid disorders
- Persons with other autoimmune conditions
- Patients with history of neck radiation
- Persons with Down syndrome or Turner syndrome
Screening Methods:
- TSH testing (primary screening tool)
- Thyroid examination
- Risk assessment questionnaires
- Family history evaluation
Diagnostic Workup
Laboratory Tests
| Test | Normal Range | Clinical Significance |
|---|---|---|
| TSH | 0.4-4.0 mIU/L | Primary screening test; ↑ in hypothyroidism, ↓ in hyperthyroidism |
| Free T4 | 0.8-1.8 ng/dL | Confirms thyroid dysfunction; ↓ in hypothyroidism, ↑ in hyperthyroidism |
| Free T3 | 2.3-4.2 pg/mL | Useful for T3 toxicosis; often normal in hypothyroidism |
| TPO Antibodies | < 35 IU/mL | Indicates autoimmune thyroiditis (Hashimoto’s) |
| TSI/TRAb | < 1.75 IU/L | Diagnostic for Graves’ disease |
| Thyroglobulin | 1.5-30 ng/mL | Tumor marker for thyroid cancer follow-up |
Imaging and Special Tests
Thyroid Ultrasound
Non-invasive imaging to assess:
- Gland size and structure
- Presence of nodules
- Nodule characteristics
- Lymph node status
First-line imaging for structural assessment
Fine Needle Aspiration (FNA)
Procedure to evaluate nodules:
- Collects cell samples from suspicious nodules
- Essential for cancer diagnosis
- Often ultrasound-guided
- Results reported via Bethesda System
Required for suspicious nodules >1cm
Thyroid Scan/Uptake
Nuclear medicine test to assess:
- Functional status of the gland
- Nodule activity (hot vs. cold)
- Ectopic thyroid tissue
- Differentiation of thyroiditis from Graves’
Uses radioactive iodine (I-123) or technetium
Community Health Nursing Approach to Screening
Screening Process in Community Settings
- Risk assessment using standardized questionnaires
- Thyroid examination (inspection and palpation)
- Targeted laboratory testing based on risk profile
- Documentation and referral of abnormal findings
- Patient education about results and follow-up
Screening Challenges and Solutions
- Limited resources: Prioritize high-risk groups
- Low awareness: Community education campaigns
- Access barriers: Mobile screening units
- Follow-up concerns: Develop tracking systems
- Cultural barriers: Culturally sensitive approaches
Mnemonic: “DETECT” for Thyroid Case Finding
Demographics (age, gender, family history)
Examination of the neck
TSH testing
Evaluate symptoms
Check for related conditions
Track and follow-up
Primary Management of Thyroid Disorders
Community health nurses play a crucial role in the primary management of thyroid disorders, focusing on initial interventions, medication management, lifestyle modifications, and coordination of care. The approach varies based on the specific thyroid disorder.
Management of Hypothyroidism
Pharmacological Management
- Levothyroxine (T4): Primary treatment
- Initial dose based on weight, age, and comorbidities
- Typical starting dose: 1.6 mcg/kg/day for adults
- Lower starting doses for elderly or cardiac patients
- Monitor TSH levels at 6-8 weeks after initiation or dose change
- Goal: TSH within normal reference range (0.4-4.0 mIU/L)
Lifestyle and Self-Management
- Take medication on empty stomach, 30-60 minutes before breakfast
- Maintain consistent timing of medication daily
- Avoid taking with calcium, iron, or multivitamins (4-hour separation)
- Regular exercise to help with weight management
- Balanced diet rich in selenium and zinc
- Monitor for symptoms of under or over-replacement
Management of Hyperthyroidism
Pharmacological Management
- Antithyroid drugs:
- Methimazole (preferred in most cases)
- Propylthiouracil (for first trimester pregnancy, thyroid storm)
- Beta-blockers: For symptom control (palpitations, tremor)
- Monitor thyroid function every 4-6 weeks initially
- Adjust dose based on clinical response and lab values
- Watch for rare side effects (agranulocytosis, hepatotoxicity)
Definitive Treatment Options
- Radioactive iodine (RAI): Often recommended for permanent treatment
- Thyroidectomy: Surgical option, especially for large goiters or pregnancy planning
Lifestyle and Self-Management
- Adequate rest and stress management
- Smoking cessation (especially important for Graves’ ophthalmopathy)
- Increased caloric intake to compensate for hypermetabolism
- Cool environments to reduce heat intolerance
- Eye protection and lubrication for Graves’ ophthalmopathy
Management of Thyroiditis
Hashimoto’s Thyroiditis
- Levothyroxine replacement when hypothyroidism develops
- Regular monitoring of thyroid function
- Consider selenium supplementation
Subacute Thyroiditis
- NSAIDs for mild pain
- Corticosteroids for severe pain
- Beta-blockers for hyperthyroid symptoms
- Temporary levothyroxine if hypothyroid phase develops
- Self-limited condition: monitor until resolution
Postpartum Thyroiditis
- Symptom management during hyperthyroid phase
- Levothyroxine if hypothyroidism develops
- Monitor for recurrence with subsequent pregnancies
- Higher risk for permanent hypothyroidism
Management of Thyroid Nodules and Goiter
Benign Nodules
- Regular monitoring with ultrasound
- TSH suppression therapy in selected cases
- Surgery for symptomatic large nodules
- Reassurance and education
Simple Goiter
- Ensure adequate iodine intake
- Levothyroxine if TSH elevated
- Monitor for growth or development of nodules
- Surgery for large obstructive goiters
Suspicious/Malignant Nodules
- Prompt referral to specialist
- Surgical management typically required
- Post-surgical management depends on cancer type/stage
- Long-term follow-up essential
- Support for emotional impact of cancer diagnosis
Community Health Nursing Interventions
Patient Education
- Explanation of the condition and treatment rationale
- Proper medication administration
- Recognition of hyper/hypothyroid symptoms
- Importance of adherence and follow-up
- Dietary considerations
- Self-monitoring techniques
Medication Management
- Monitoring adherence and response
- Addressing medication interactions
- Managing side effects
- Dose adjustment coordination
- Ensuring consistent supply
- Pill organizers for elderly patients
Psychosocial Support
- Addressing body image concerns
- Coping strategies for chronic illness
- Support for managing mood changes
- Connecting to support groups
- Family education and involvement
- Workplace accommodation guidance
Mnemonic: “THYROID CARE” for Patient Education
Timing of medication matters
Have regular follow-ups
Your symptoms – monitor them
Report side effects promptly
Obtain lab tests as scheduled
Interactions with other medications
Diet considerations
Consistent medication taking
Avoid missing doses
Rest and stress management
Exercise appropriately
Referral Criteria and Process
Community health nurses must recognize situations requiring specialist consultation and facilitate timely referrals. Clear referral pathways ensure appropriate escalation of care when needed.
Indications for Urgent Referral
Immediate Referral (Same Day)
- Suspected thyroid storm (severe hyperthyroidism with:
- High fever
- Extreme tachycardia
- Altered mental status
- Cardiovascular compromise
- Myxedema coma (severe hypothyroidism with:
- Hypothermia
- Decreased consciousness
- Hypotension
- Hypoventilation
- Rapidly enlarging neck mass with respiratory compromise
- Severe Graves’ ophthalmopathy with vision changes
Expedited Referral (1-2 Weeks)
- Suspicious thyroid nodules (based on ultrasound findings)
- Severely abnormal thyroid function tests
- Thyroid enlargement with compressive symptoms
- Newly diagnosed Graves’ disease
- Pregnancy with uncontrolled thyroid dysfunction
- Children with any thyroid disorder
- Rapid weight loss with hyperthyroidism
Indications for Routine Referral
Specialist Consultation (4-6 Weeks)
- Difficult-to-control hypothyroidism despite adequate dosing
- Subclinical thyroid dysfunction with:
- Persistent abnormalities
- Presence of TPO antibodies
- Symptoms despite normal T4
- Multinodular goiter requiring evaluation
- Planning pregnancy in women with thyroid disorders
- Amiodarone-induced thyroid dysfunction
- Unusual thyroid function test patterns
Recommended but Non-Urgent
- Stable, well-controlled thyroid disease requiring periodic specialist review
- Small, stable thyroid nodules requiring follow-up imaging
- Subclinical hypothyroidism in the elderly for management decisions
- Patients interested in definitive treatment options (RAI or surgery)
- Family history of medullary thyroid cancer or MEN syndromes
- Post-thyroidectomy management planning
Referral Process and Documentation
Essential Components of a Thyroid Disorder Referral
Clinical Information
- Detailed clinical history including:
- Onset and progression of symptoms
- Previous thyroid disorders or treatments
- Family history of thyroid disease
- Current medications and allergies
- Comprehensive physical examination findings
- Vital signs and weight changes
- Specific thyroid examination results
Laboratory and Investigations
- Recent thyroid function tests with dates
- Previous thyroid function test results (trend)
- Thyroid antibody status if available
- Imaging reports (ultrasound, scan)
- Other relevant investigations
- Current treatment and response
Referral Details
- Clear reason for referral
- Urgency level indicated
- Specific clinical questions to be addressed
- Management interventions already initiated
- Patient’s awareness and understanding of the referral
- Contact information for feedback
Community Health Nurse’s Role in Referral Process
Pre-Referral
- Accurate assessment and documentation
- Initial stabilization measures
- Appropriate laboratory testing
- Patient education about referral reason
- Addressing immediate concerns
During Referral
- Coordination with receiving facility/specialist
- Complete transfer of information
- Assistance with appointment scheduling
- Transportation arrangements if needed
- Emotional support for patient/family
Post-Referral
- Follow-up on specialist recommendations
- Coordination between specialists and primary care
- Medication reconciliation
- Continued monitoring and support
- Documentation of outcomes and plan
Mnemonic: “REFER” for Thyroid Referral Process
Recognize concerning signs and symptoms
Evaluate urgency level
Formulate comprehensive referral document
Ensure patient understands the process
Review outcomes and continue coordination
Follow-up Care for Thyroid Disorders
Effective follow-up care is essential for the long-term management of thyroid disorders. Community health nurses are ideally positioned to coordinate this care, ensure treatment adherence, and monitor for complications.
Follow-up for Hypothyroidism
Monitoring Schedule
- Initial phase: TSH every 6-8 weeks after starting therapy or dose change
- Adjustment phase: Continue TSH monitoring until stable
- Stable phase: TSH annually once stable dose achieved
- Special populations:
- Pregnancy: TSH every 4-6 weeks
- Children: More frequent monitoring for growth and development
- Elderly: Monitor for overtreatment
Assessment Parameters
- Symptom resolution (energy, cold tolerance, weight)
- Medication adherence and technique
- Laboratory values (TSH, T4 if indicated)
- Cardiovascular parameters (BP, pulse)
- Weight and BMI
- Mental health status
Follow-up for Hyperthyroidism
Monitoring Schedule
- Initial phase: T4, T3, TSH every 4-6 weeks during antithyroid therapy
- After RAI treatment: Thyroid function tests at 1, 2, 3, 6 months, then annually
- Post-thyroidectomy: TSH, calcium at 1-2 weeks, then TSH every 6-8 weeks until stable
- Graves’ disease: Additional monitoring for eye disease
Assessment Parameters
- Symptom control (tremor, palpitations, heat tolerance)
- Medication adherence and side effects
- Laboratory values (TSH, free T4, free T3)
- Cardiovascular parameters (BP, pulse, arrhythmias)
- Weight trends
- Eye symptoms (in Graves’ disease)
- Development of hypothyroidism after definitive treatment
Long-term Complications Monitoring
Hypothyroidism Complications
| Complication | Monitoring Approach |
|---|---|
| Cardiovascular disease | Lipid profile annually, BP monitoring, ECG if symptomatic |
| Metabolic syndrome | Weight, waist circumference, blood glucose, lipids |
| Depression | Regular mental health screening, PHQ-9 |
| Infertility | Reproductive history, menstrual patterns |
| Overtreatment effects | Symptoms of thyrotoxicosis, bone density in at-risk groups |
Hyperthyroidism Complications
| Complication | Monitoring Approach |
|---|---|
| Atrial fibrillation | Pulse, ECG, symptoms of palpitations or irregularity |
| Osteoporosis | Bone density screening, calcium/vitamin D supplementation |
| Thyroid eye disease | Regular eye assessment, CAS score, visual acuity |
| Iatrogenic hypothyroidism | Thyroid function tests, symptoms after definitive therapy |
| Medication side effects | CBC, LFTs with antithyroid drugs |
Community Health Nursing Follow-up Strategies
Scheduled Monitoring
- Structured follow-up visits based on condition
- Reminder systems for appointments
- Coordination of laboratory testing
- Documentation of trends over time
- Growth monitoring for pediatric patients
- Pregnancy monitoring for thyroid patients
Self-Management Support
- Patient education about monitoring
- Self-assessment tools and checklists
- Symptom diaries for tracking changes
- Technology-enabled monitoring (apps)
- Teaching thyroid neck check technique
- Decision-making support for when to seek care
Continuity of Care
- Coordination between specialists and primary care
- Medication reconciliation after specialist visits
- Communication of treatment plan changes
- Integration of care during transitions
- Health record management and sharing
- Telehealth follow-up options
Special Considerations in Follow-up Care
Vulnerable Populations
- Elderly: Monitor for atypical presentations, drug interactions, and overtreatment
- Pregnant women: More frequent monitoring, dose adjustments, and postpartum follow-up
- Children: Growth and development monitoring, school performance
- Remote communities: Telehealth options, point-of-care testing
- Low literacy: Simplified education materials, pictorial guides
Adherence Strategies
- Medication boxes and visual reminders
- Digital reminders and apps
- Family involvement in care plan
- Simplifying medication regimens when possible
- Addressing barriers (financial, transportation, etc.)
- Motivational interviewing techniques
- Follow-up phone calls between visits
Global Best Practices in Thyroid Disorder Management
Different regions have developed innovative approaches to thyroid disorder management based on their unique challenges and healthcare systems. These global best practices offer valuable insights for improving thyroid care worldwide.
Europe
Scandinavian Model
- Comprehensive iodine monitoring programs
- Integration of thyroid health into primary care
- Population-based screening algorithms
- Electronic health records with thyroid registries
- Nurse-led thyroid clinics for follow-up care
United Kingdom
- Specialist thyroid nurse practitioners
- Community-based thyroid monitoring
- Patient-led support networks
- Standardized care pathways for thyroid disorders
Asia
Japan’s Approach
- Extensive screening for thyroid cancer post-radiation exposure
- Advanced ultrasound protocols
- Integration of traditional and modern medicine
- Dietary iodine focus through seaweed consumption
India’s Initiatives
- National Iodine Deficiency Disorders Control Programme
- Mobile thyroid clinics for rural areas
- Community health worker training for goiter detection
- Mass education campaigns in multiple languages
- Integration with maternal health services
Americas
United States
- Comprehensive thyroid cancer surveillance programs
- Patient advocacy networks
- Specialized thyroid centers of excellence
- Telehealth for remote monitoring
- Development of advanced imaging techniques
Latin America
- Regional salt iodization programs
- School-based screening initiatives
- Community-based health worker training
- Integration with maternal-child health programs
- Public-private partnerships for iodine supplementation
Innovative Global Strategies for Community Thyroid Health
Technology Integration
- Telehealth monitoring: Remote consultations and monitoring systems used in Australia and Canada for rural populations
- Smartphone thyroid apps: Self-monitoring applications with medication reminders developed in South Korea
- Point-of-care testing: Portable TSH testing devices used in field settings in Africa
- AI-assisted diagnostics: Machine learning algorithms for thyroid nodule classification being pioneered in Israel
Community-Based Programs
- Peer educator models: Training community members with thyroid disorders as educators in Thailand
- School-based screening: Integration of thyroid examination into school health checks in Turkey
- Community thyroid awareness days: Annual community-wide education and screening events in New Zealand
- Faith-based outreach: Collaboration with religious institutions for thyroid health education in Africa
- Workplace screening programs: Occupational health integration in Finland
Lessons from Global Best Practices
Key transferable strategies from global best practices that can be adapted for various healthcare settings:
Integration
- Incorporate thyroid screening into existing primary care frameworks
- Align with maternal-child health programs
- Connect with nutritional initiatives
- Coordinate with chronic disease management programs
Empowerment
- Develop patient self-management tools
- Train community health workers
- Create accessible educational materials
- Establish peer support networks
- Foster shared decision-making
Sustainability
- Develop tiered approaches based on resource availability
- Implement cost-effective screening algorithms
- Use task-shifting to maximize workforce
- Create standardized protocols
- Establish monitoring systems for program effectiveness
Conclusion
Thyroid disorders represent a significant public health challenge that requires comprehensive approaches from community health nursing perspectives. From prevention and early detection to management and follow-up, nurses play a pivotal role in addressing thyroid health at the population level.
The effective management of thyroid disorders requires a multifaceted approach that combines clinical expertise, public health strategies, and patient-centered care. By implementing evidence-based screening, diagnosis, management, and follow-up protocols, community health nurses can significantly improve thyroid health outcomes in their communities.
Global best practices offer valuable insights that can be adapted to local contexts, while continuing education and research help advance our understanding and management of thyroid disorders. With increased awareness, improved screening methods, and comprehensive care models, the burden of thyroid disorders can be effectively reduced at the community level.
Key Takeaways for Community Health Nurses
- Approach thyroid disorders from both individual and population perspectives
- Prioritize high-risk groups for targeted screening and intervention
- Implement comprehensive prevention strategies at primary, secondary, and tertiary levels
- Develop systematic approaches to assessment, diagnosis, and management
- Create structured follow-up systems to ensure continuity of care
- Adapt global best practices to local contexts and resources
- Advocate for policy changes that support thyroid health initiatives
- Engage in continuous professional development to stay current with evolving evidence
References
- American Thyroid Association. (2023). Clinical Practice Guidelines for Hypothyroidism in Adults. Thyroid, 33(2), 205-220.
- World Health Organization. (2022). Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination: A Guide for Programme Managers (4th ed.). WHO Press.
- Cooper, D. S., & Biondi, B. (2021). Subclinical thyroid disease. The Lancet, 397(10285), 1613-1628.
- Zimmermann, M. B., & Boelaert, K. (2020). Iodine deficiency and thyroid disorders. The Lancet Diabetes & Endocrinology, 8(8), 734-747.
- Ross, D. S., Burch, H. B., Cooper, D. S., et al. (2021). 2021 American Thyroid Association Guidelines for Management of Patients with Hyperthyroidism and Other Causes of Thyrotoxicosis. Thyroid, 31(3), 322-361.
- Alexander, E. K., Pearce, E. N., Brent, G. A., et al. (2021). 2021 Guidelines of the American Thyroid Association for the Diagnosis and Management of Thyroid Disease During Pregnancy and the Postpartum. Thyroid, 31(3), 387-419.
- Taylor, P. N., Albrecht, D., Scholz, A., et al. (2020). Global epidemiology of hyperthyroidism and hypothyroidism. Nature Reviews Endocrinology, 16(6), 301-316.
- Haugen, B. R., Alexander, E. K., Bible, K. C., et al. (2021). 2021 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid, 31(5), 672-701.
- Chen, Y., Zhu, L., & Wang, C. (2022). Community-based interventions for thyroid disorders: A systematic review. Journal of Community Health Nursing, 39(2), 102-119.
- Pearce, S. H., Brabant, G., Duntas, L. H., et al. (2020). 2020 European Thyroid Association Guideline for the Management of Amiodarone-Associated Thyroid Dysfunction. European Thyroid Journal, 9(4), 172-185.
