Immunity, Antigens & Antibodies, and Hypersensitivity Reactions
Comprehensive Nursing Study Notes
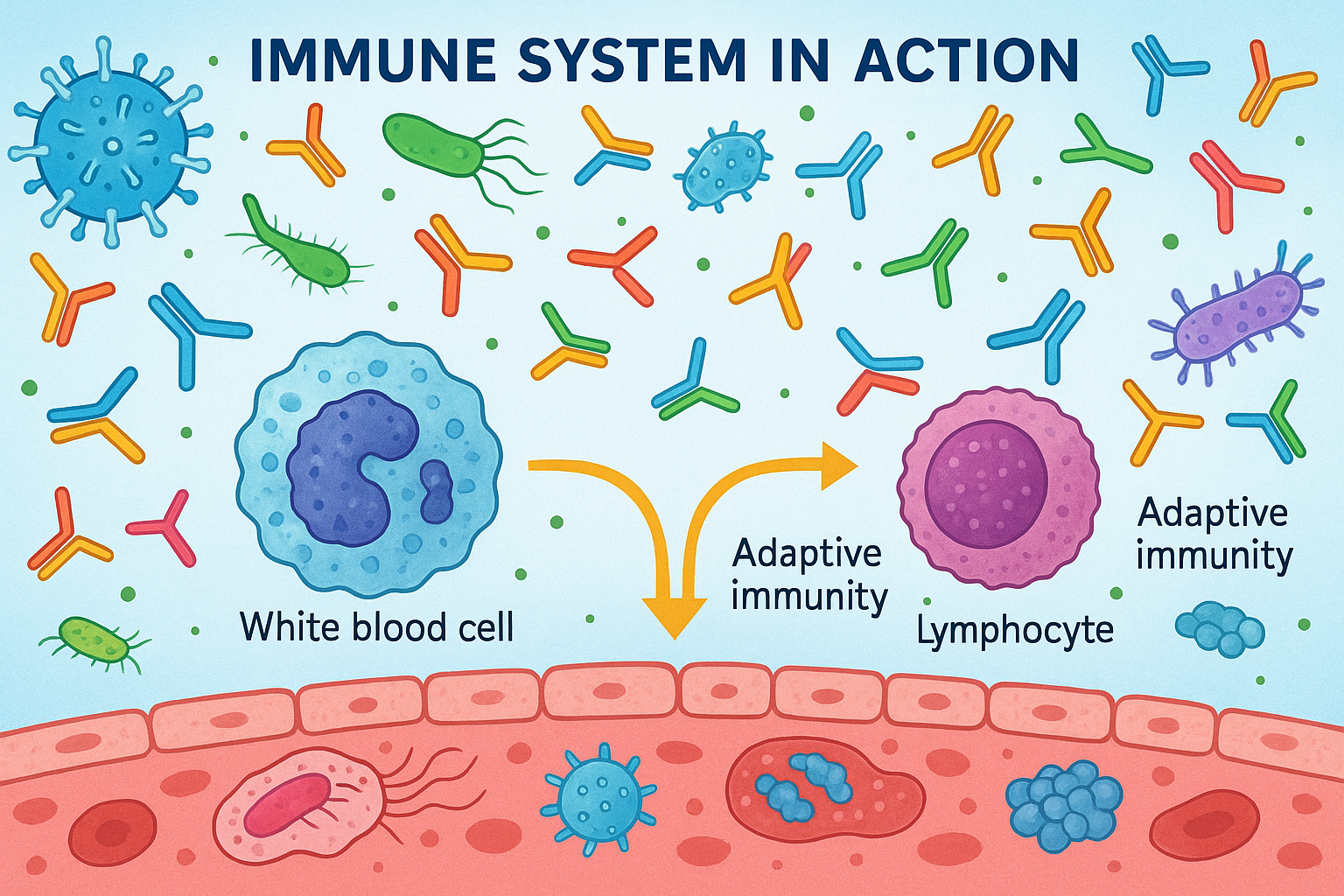
The immune system in action: antibodies, pathogens, and cellular responses
Table of Contents
1. Introduction to Immunity
2. Antigens and Antibodies
3. Hypersensitivity Reactions
4. Nursing Applications
Overview of the Immune System
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful pathogens, including bacteria, viruses, fungi, and parasites. This sophisticated defense mechanism distinguishes between “self” and “non-self” substances, providing protection while maintaining tolerance to the body’s own tissues.
Primary Functions of the Immune System:
- Recognition: Identifying foreign antigens and distinguishing them from self-antigens
- Response: Mounting appropriate defensive reactions against identified threats
- Memory: Developing immunological memory for rapid response upon re-exposure
- Tolerance: Preventing attacks on the body’s own healthy tissues
- Elimination: Removing pathogens, toxins, and abnormal cells from the body
Immunity Classification Flowchart
• Non-specific
• Immediate response
• Memory formation
• Delayed activation
1. Innate (Non-Specific) Immunity
Innate immunity provides the first line of defense against pathogens. It consists of physical, chemical, and cellular barriers that are present from birth and respond immediately to threats without prior exposure.
| Component | Examples | Function |
|---|---|---|
| Physical Barriers | Skin, mucous membranes, cilia | Prevent pathogen entry |
| Chemical Barriers | Stomach acid, antimicrobial peptides, lysozyme | Destroy or inhibit pathogens |
| Cellular Components | Neutrophils, macrophages, NK cells, dendritic cells | Phagocytosis and pathogen elimination |
| Molecular Components | Complement system, interferons, inflammatory mediators | Enhance immune responses and inflammation |
2. Adaptive (Specific) Immunity
Adaptive immunity develops throughout life and provides specific, long-lasting protection against particular antigens. It involves lymphocytes (B cells and T cells) and creates immunological memory.
Humoral Immunity (B Cells)
- • Antibody-mediated responses
- • Effective against extracellular pathogens
- • Memory B cells provide rapid secondary responses
- • Neutralization, opsonization, complement activation
Cell-Mediated Immunity (T Cells)
- • T cell-mediated responses
- • Effective against intracellular pathogens
- • Memory T cells provide long-term protection
- • Cytotoxicity, helper functions, regulatory control
Classification by Acquisition Method
Natural Immunity
Maternal antibodies transferred through placenta or breast milk
Immunity acquired through natural infection and recovery
Artificial Immunity
Pre-formed antibodies administered (immunoglobulins, antisera)
Immunity acquired through vaccination with antigens
Memory Aid: “PANA Classification”
Active Natural – Actual infection
Active Artificial – Administered vaccines
Duration and Characteristics
| Type | Onset | Duration | Memory | Clinical Example |
|---|---|---|---|---|
| Passive Natural | Immediate | 3-6 months | None | Newborn protection from maternal antibodies |
| Active Natural | 1-2 weeks | Years to lifetime | Yes | Recovery from chickenpox |
| Passive Artificial | Immediate | 2-8 weeks | None | Hepatitis B immune globulin |
| Active Artificial | 1-2 weeks | Years (boosters may be needed) | Yes | MMR vaccination |
Antigens: Structure and Function
An antigen (antibody generator) is any substance that can trigger an immune response by binding to antibodies or T cell receptors. Antigens are typically foreign substances, but can also include altered self-components in autoimmune conditions.
Antigen Classifications
By Origin
- Exogenous: External origin (bacteria, viruses, pollen)
- Endogenous: Internal origin (tumor antigens, self-antigens)
- Autoantigens: Body’s own molecules in autoimmune disease
- Alloantigens: From genetically different individuals
By Structure
- Complete Antigens: Can induce immune response alone
- Haptens: Require carrier molecules to be immunogenic
- Superantigens: Activate large populations of T cells
- T-dependent: Require T cell help for B cell activation
Antigenic Determinants (Epitopes)
Epitopes are specific regions of an antigen that are recognized by antibodies or T cell receptors. A single antigen may have multiple epitopes, allowing for diverse immune responses.
Antigen capture by antigen-presenting cells
Intracellular degradation and peptide generation
Display on MHC molecules for T cell recognition
Antibody Structure and Function
Antibodies, also known as immunoglobulins (Ig), are Y-shaped proteins produced by B cells that specifically bind to antigens. They consist of heavy and light chains with variable and constant regions that determine their specificity and function.
Basic Antibody Structure
- Fab region (Fragment antigen-binding): Variable region that binds specific antigens
- Fc region (Fragment crystallizable): Constant region that determines antibody class and effector functions
- Heavy chains: Determine antibody class (IgG, IgA, IgM, IgD, IgE)
- Light chains: Either kappa (κ) or lambda (λ) types
Classes of Antibodies
| Class | % in Serum | Location | Primary Function | Clinical Significance |
|---|---|---|---|---|
| IgG | 75-85% | Blood, tissues | Long-term immunity, neutralization | Crosses placenta, secondary immune response |
| IgA | 10-15% | Mucous membranes, secretions | Mucosal immunity | Found in saliva, tears, breast milk |
| IgM | 5-10% | Blood, lymph | Primary immune response | First antibody produced, complement activation |
| IgD | <1% | B cell surface | B cell activation | Antigen recognition receptor |
| IgE | <1% | Mast cells, basophils | Allergic reactions, parasite defense | Elevated in allergies and parasitic infections |
Memory Aid: “GAMED” for Antibody Classes
Antibody Functions
Direct Effects
- Neutralization: Blocking pathogen binding sites
- Agglutination: Clumping of particulate antigens
- Precipitation: Formation of immune complexes
- Opsonization: Marking pathogens for phagocytosis
Indirect Effects
- Complement activation: Enhanced pathogen destruction
- ADCC: Antibody-dependent cell-mediated cytotoxicity
- Mast cell degranulation: Release of inflammatory mediators
- Enhanced phagocytosis: Improved uptake by immune cells
Mechanisms of Antigen-Antibody Interactions
Antigen-antibody reactions are highly specific, reversible interactions governed by several factors including antigen concentration, antibody affinity, temperature, and pH. These reactions form the basis of both protective immunity and diagnostic testing.
Key Characteristics of Antigen-Antibody Binding
Specificity
Each antibody recognizes a unique epitope with high precision, similar to lock-and-key mechanism
Affinity
Strength of binding between individual antibody and antigen binding sites
Avidity
Overall strength of binding when multiple binding sites are involved
Reversibility
Non-covalent bonds allow for dynamic equilibrium between bound and unbound states
Types of Antigen-Antibody Reactions
1. Neutralization
Antibodies bind to critical sites on pathogens or toxins, preventing their harmful effects. This is the primary mechanism of protection against many viral and bacterial infections.
2. Agglutination
Cross-linking of particulate antigens (bacteria, red blood cells) by antibodies, forming visible clumps. Used extensively in diagnostic testing.
3. Precipitation
Formation of insoluble immune complexes when soluble antigens react with antibodies at optimal proportions. Used in immunodiffusion tests.
4. Opsonization
Antibodies coat pathogens, making them more recognizable and easily phagocytosed by macrophages and neutrophils.
Factors Affecting Antigen-Antibody Reactions
| Factor | Effect | Clinical Relevance |
|---|---|---|
| Temperature | Optimal at 37°C for most reactions | Cold agglutinins active at lower temperatures |
| pH | Physiological pH (7.4) is optimal | Acidic conditions can dissociate immune complexes |
| Ionic Strength | Low ionic strength enhances binding | Saline concentration affects blood bank tests |
| Antigen:Antibody Ratio | Optimal ratio produces maximum precipitation | Excess antigen or antibody inhibits reactions |
Overview and Classification
Hypersensitivity reactions are exaggerated or inappropriate immune responses to antigens that result in tissue damage rather than protection. These reactions are classified into four types based on the Gell and Coombs classification system, each involving different immune mechanisms and clinical presentations.
Gell and Coombs Classification
Memory Aid: “ACID” for Hypersensitivity Types
Cytotoxic (Type II) – Cell destruction
Delayed (Type IV) – Dermatitis reactions
General Characteristics Comparison
| Type | Mediator | Onset Time | Duration | Pathology |
|---|---|---|---|---|
| Type I | IgE, mast cells, basophils | 2-30 minutes | 2-6 hours | Smooth muscle contraction, vasodilation |
| Type II | IgG, IgM, complement, phagocytes | 5-8 hours | Hours to days | Cell lysis, phagocytosis |
| Type III | IgG immune complexes, complement | 2-8 hours | Days to weeks | Neutrophil infiltration, tissue damage |
| Type IV | T cells, macrophages, cytokines | 24-72 hours | Days to weeks | Granuloma formation, tissue destruction |
Mechanism and Pathophysiology
Type I hypersensitivity is an IgE-mediated immediate allergic reaction involving mast cell and basophil degranulation. This reaction occurs within minutes of exposure to a previously sensitized antigen and can range from localized symptoms to life-threatening anaphylaxis.
Type I Hypersensitivity Process
First exposure to allergen
IgE production by B cells
IgE binds to mast cells
Antigen cross-links IgE
Mast cell activation
Signal transduction
Release of preformed mediators
Histamine, tryptase
Chemotactic factors
Newly synthesized mediators
Leukotrienes, prostaglandins
Sustained inflammation
Clinical Manifestations
Systemic Anaphylaxis
- Cardiovascular: Hypotension, tachycardia, shock
- Respiratory: Bronchospasm, laryngeal edema, dyspnea
- Gastrointestinal: Nausea, vomiting, diarrhea, cramping
- Cutaneous: Urticaria, angioedema, flushing
- Neurological: Anxiety, confusion, loss of consciousness
Localized Reactions
- Allergic Rhinitis: Sneezing, rhinorrhea, nasal congestion
- Allergic Asthma: Wheezing, cough, shortness of breath
- Atopic Dermatitis: Eczematous lesions, pruritus
- Food Allergies: GI symptoms, oral allergy syndrome
- Drug Allergies: Skin rashes, localized swelling
Common Triggers
| Category | Common Examples | Nursing Considerations |
|---|---|---|
| Medications | Penicillin, NSAIDs, contrast agents | Always check allergy history before administration |
| Foods | Peanuts, shellfish, eggs, milk | Review dietary restrictions and meal planning |
| Environmental | Pollen, dust mites, pet dander | Environmental controls and trigger avoidance |
| Insect Stings | Bee, wasp, hornet, fire ant | EpiPen training and emergency preparedness |
- • Assess airway, breathing, circulation immediately
- • Administer epinephrine 0.3-0.5mg IM (adult dose) without delay
- • Position patient supine with legs elevated if hypotensive
- • Prepare for intubation if laryngeal edema present
- • Monitor for biphasic reactions (4-12 hours post-exposure)
Mechanism and Pathophysiology
Type II hypersensitivity involves IgG or IgM antibodies directed against cell surface or matrix antigens, leading to complement activation and cell destruction through various mechanisms including complement-mediated lysis, antibody-dependent cellular cytotoxicity (ADCC), and opsonization.
Mechanisms of Cell Destruction
Complement-Mediated Lysis
Antibodies activate complement cascade, leading to membrane attack complex formation and cell lysis.
ADCC
NK cells and macrophages recognize antibody-coated cells via Fc receptors and destroy them.
Opsonization
Antibody coating promotes phagocytosis by macrophages and neutrophils.
Clinical Examples
Hemolytic Transfusion Reactions
Mechanism: ABO or Rh incompatibility leading to recipient antibodies attacking donor red blood cells.
Timeline: Acute (minutes to hours) or delayed (days to weeks)
- • Stop transfusion immediately
- • Maintain IV access with normal saline
- • Monitor vital signs and urine output
- • Send blood samples for compatibility testing
Hemolytic Disease of Newborn (HDN)
Mechanism: Rh-negative mother develops anti-Rh antibodies that cross placenta and attack Rh-positive fetal cells.
Prevention: RhoGAM administration to Rh-negative mothers
- • Monitor for jaundice in newborn
- • Assess for signs of anemia
- • Prepare for phototherapy or exchange transfusion
- • Support family during treatment
Drug-Induced Cytopenias
Common Drugs: Quinidine, methyldopa, heparin, vancomycin
Types: Hemolytic anemia, thrombocytopenia, neutropenia
- • Monitor complete blood counts regularly
- • Assess for signs of bleeding or infection
- • Document any adverse reactions
- • Coordinate with physician for drug discontinuation
Autoimmune Manifestations
| Condition | Target Antigen | Clinical Features | Nursing Focus |
|---|---|---|---|
| Goodpasture’s Syndrome | Basement membrane collagen | Glomerulonephritis, pulmonary hemorrhage | Monitor kidney function, respiratory status |
| Pemphigus Vulgaris | Desmoglein proteins | Blistering skin lesions, mucosal ulcers | Wound care, infection prevention |
| Myasthenia Gravis | Acetylcholine receptors | Muscle weakness, ptosis, dysphagia | Respiratory monitoring, swallowing assessment |
Mechanism and Pathophysiology
Type III hypersensitivity results from the formation and deposition of antigen-antibody immune complexes in tissues, particularly in blood vessels, joints, and kidneys. These complexes activate complement and recruit inflammatory cells, causing tissue damage through inflammation rather than direct cytotoxicity.
Immune Complex Disease Progression
Antigen + Antibody
Immune complexes in bloodstream
Tissue localization
Complement activation
Neutrophil infiltration
Factors Affecting Immune Complex Disease
Complex Size and Ratio
- Large complexes: Rapidly removed by phagocytes
- Small complexes: Circulate longer, deposit in tissues
- Optimal ratio: Slight antigen excess promotes pathology
- Antibody excess: Rapid clearance, less pathogenic
Tissue Factors
- Blood flow: High flow areas accumulate more complexes
- Filtration: Kidneys are primary deposition site
- Inflammation: Increases vascular permeability
- Charge: Cationic complexes deposit more readily
Clinical Manifestations
Systemic Lupus Erythematosus (SLE)
Pathology: Immune complexes containing nuclear antigens (DNA, histones) deposit in multiple organs.
Affected Systems: Kidneys, skin, joints, cardiovascular, CNS
- • Monitor for malar rash and photosensitivity
- • Assess joint pain and morning stiffness
- • Track proteinuria and kidney function
- • Evaluate neuropsychiatric symptoms
Serum Sickness
Cause: Foreign proteins (antitoxins, therapeutic antibodies) or drugs (penicillin, sulfonamides).
Timeline: 1-3 weeks after initial exposure, 1-4 days after re-exposure
- • Fever and malaise
- • Arthralgia and arthritis
- • Skin rash (urticaria, purpura)
- • Lymphadenopathy
Hypersensitivity Pneumonitis
Triggers: Organic dusts (bird antigens, fungi, bacteria) in occupational or home environments.
Examples: Farmer’s lung, bird fancier’s lung, hot tub lung
- • Acute: Fever, cough, dyspnea (4-6h post-exposure)
- • Subacute: Progressive dyspnea, fatigue
- • Chronic: Pulmonary fibrosis, respiratory failure
Laboratory Findings
| Test | Finding | Clinical Significance |
|---|---|---|
| Complement Levels | ↓ C3, C4, CH50 | Consumed in immune complex activation |
| Circulating Immune Complexes | ↑ Levels detected | Confirms immune complex disease |
| Tissue Biopsy | Granular deposits of Ig and complement | Diagnostic for organ involvement |
| Autoantibodies | ANA, anti-DNA, RF | Identifies autoimmune component |
- • Monitor for multi-system manifestations of disease
- • Assess response to immunosuppressive therapy
- • Educate patients about trigger avoidance when applicable
- • Support patients with chronic autoimmune conditions
- • Watch for complications of immunosuppression (infections)
Mechanism and Pathophysiology
Type IV hypersensitivity is mediated by T cells rather than antibodies and typically manifests 24-72 hours after exposure to the antigen. This delayed response involves sensitized T helper cells (Th1) that release cytokines, leading to macrophage activation and tissue damage through cell-mediated mechanisms.
Type IV Hypersensitivity Process
Antigen presentation to naive T cells
Th1 cell differentiation
Memory T cell formation
Memory T cell recognition
Rapid T cell activation
Clonal expansion
IL-2, IFN-γ, TNF-α
Macrophage recruitment
Inflammatory cascade
Macrophage activation
Granuloma formation
Tissue destruction
Clinical Manifestations and Examples
Contact Dermatitis
Common Triggers: Poison ivy (urushiol), nickel, latex, cosmetics, topical medications
Pathophysiology: Hapten-protein conjugates processed by Langerhans cells
Timeline: 24-48 hours for initial reaction, 8-12 hours for repeat exposure
- • Erythema and edema
- • Vesicle and bullae formation
- • Intense pruritus
- • Well-demarcated lesions
- • Secondary bacterial infection risk
Tuberculin Skin Test (TST)
Principle: Purified protein derivative (PPD) injection elicits response in individuals with TB exposure
Reading: Induration measured at 48-72 hours post-injection
Interpretation: Size thresholds vary by risk factors
- • ≥5mm: HIV+, recent TB contact, immunosuppressed
- • ≥10mm: High-risk groups, healthcare workers
- • ≥15mm: Low-risk individuals
- • False positives: BCG vaccination, atypical mycobacteria
Granulomatous Diseases
Formation: Chronic antigenic stimulation leads to organized collections of activated macrophages (epithelioid cells)
Examples: Tuberculosis, sarcoidosis, Crohn’s disease, foreign body reactions
- • Central core of epithelioid cells
- • Multinucleated giant cells (Langhans type)
- • Surrounding lymphocytes
- • Outer fibroblast layer
- • Possible central necrosis (caseating)
Drug Hypersensitivity
Mechanisms: Direct T cell activation, hapten formation with proteins, or metabolite-mediated reactions
Common Drugs: Anticonvulsants, antibiotics, allopurinol, NSAIDs
- • Stevens-Johnson syndrome
- • Toxic epidermal necrolysis
- • DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms)
- • Acute generalized exanthematous pustulosis
Subtypes of Type IV Hypersensitivity
| Subtype | Mediating Cells | Key Cytokines | Clinical Example |
|---|---|---|---|
| IVa | Th1 cells, macrophages | IFN-γ, IL-2, TNF-α | Tuberculin test, contact dermatitis |
| IVb | Th2 cells, eosinophils | IL-4, IL-5, IL-13 | Chronic asthma, atopic dermatitis |
| IVc | CTLs (CD8+ T cells) | Perforin, granzymes | Stevens-Johnson syndrome, graft rejection |
| IVd | Th17 cells, neutrophils | IL-17, IL-22 | Acute generalized pustulosis |
Assessment Strategies
Comprehensive assessment of immune function and hypersensitivity reactions requires systematic evaluation of patient history, physical findings, and understanding of risk factors. Nurses play a critical role in early recognition and prompt intervention for immune-mediated conditions.
Comprehensive Allergy History
Key History Components
- Allergen identification: Specific triggers and cross-reactivity
- Reaction type: Local vs. systemic manifestations
- Timing: Immediate vs. delayed onset patterns
- Severity: Mild symptoms to life-threatening anaphylaxis
- Previous treatment: Medications used and effectiveness
- Family history: Genetic predisposition to atopy
Red Flag Symptoms
- Respiratory: Stridor, wheezing, severe dyspnea
- Cardiovascular: Hypotension, tachycardia, syncope
- Cutaneous: Generalized urticaria, angioedema
- Gastrointestinal: Severe cramping, diarrhea, vomiting
- Neurological: Altered mental status, seizures
- Multi-system: Rapid progression of symptoms
Physical Assessment Techniques
| System | Assessment Focus | Key Findings | Clinical Significance |
|---|---|---|---|
| Respiratory | Airway patency, breathing pattern | Wheezing, stridor, use of accessory muscles | Bronchospasm, laryngeal edema |
| Cardiovascular | Hemodynamic stability | Hypotension, tachycardia, weak pulse | Anaphylactic shock, volume redistribution |
| Integumentary | Skin changes and lesion distribution | Urticaria, angioedema, flushing, cyanosis | Systemic histamine release, poor perfusion |
| Gastrointestinal | Abdominal symptoms | Cramping, nausea, diarrhea | Smooth muscle contraction, inflammation |
| Neurological | Mental status, consciousness level | Anxiety, confusion, loss of consciousness | Hypoxia, hypotension, cerebral hypoperfusion |
Memory Aid: “ABCDE” Assessment for Anaphylaxis
Risk Assessment Tools
Anaphylaxis Risk Stratification
Previous severe reactions, multiple allergies, asthma, beta-blocker use
Mild previous reactions, single known allergy, atopic conditions
No known allergies, no atopic history, young age
Immunocompromise Indicators
- Recurrent infections: Unusual frequency or severity
- Opportunistic pathogens: Infections by typically benign organisms
- Poor wound healing: Delayed or abnormal repair processes
- Medication effects: Immunosuppressive therapy
- Underlying conditions: HIV, malignancy, autoimmune disease
- Laboratory abnormalities: Low lymphocyte counts, poor antibody response
Emergency Management Protocols
Anaphylaxis Emergency Protocol
Immediate Actions (First 5 minutes)
- 1. Remove or discontinue trigger if possible
- 2. Call for emergency assistance
- 3. Administer epinephrine IM (anterolateral thigh)
- 4. Position patient supine with legs elevated
- 5. Establish IV access with large-bore catheter
- 6. Administer high-flow oxygen
Secondary Interventions
- 1. IV fluid resuscitation (normal saline)
- 2. H1 antihistamine (diphenhydramine)
- 3. H2 antihistamine (ranitidine/famotidine)
- 4. Corticosteroids (methylprednisolone)
- 5. Bronchodilators if wheezing persists
- 6. Continuous monitoring and reassessment
Medication Management
| Medication | Indication | Dosage | Nursing Considerations |
|---|---|---|---|
| Epinephrine | First-line for anaphylaxis | 0.3-0.5mg IM (1:1000) | May repeat q5-15min, monitor for dysrhythmias |
| Diphenhydramine | H1 receptor blockade | 25-50mg IV/IM/PO | Sedation, anticholinergic effects |
| Methylprednisolone | Anti-inflammatory, prevent biphasic reaction | 1-2mg/kg IV | Delayed onset, monitor blood glucose |
| Albuterol | Bronchodilation | 2.5-5mg nebulized | Monitor heart rate, assess response |
Supportive Care Interventions
Hemodynamic Support
- Fluid resuscitation: 1-2L normal saline rapidly
- Positioning: Supine with legs elevated
- Vasopressors: If hypotension persists despite fluids
- Monitoring: Continuous BP, HR, urine output
- Central access: Consider if peripheral access difficult
Respiratory Support
- Oxygen therapy: High-flow oxygen via non-rebreather
- Airway management: Prepare for intubation if needed
- Positioning: Semi-Fowler’s unless hypotensive
- Monitoring: Pulse oximetry, ABGs if indicated
- Bronchodilators: Nebulized beta-agonists for wheezing
- • Never delay epinephrine – it’s the only life-saving drug in anaphylaxis
- • Observe for biphasic reactions up to 12 hours post-exposure
- • Patients on beta-blockers may not respond to epinephrine and may need glucagon
- • Document exact timeline of events and interventions for future reference
- • Ensure patient receives epinephrine auto-injector prescription before discharge
Comprehensive Patient Education Program
Effective patient education is crucial for preventing hypersensitivity reactions and managing chronic immune-related conditions. Education should be tailored to the patient’s specific condition, literacy level, and cultural background.
