Urban Health Services Organization: Staffing, Functions & Structure
Comprehensive Nursing Notes for Urban Community Health Administration
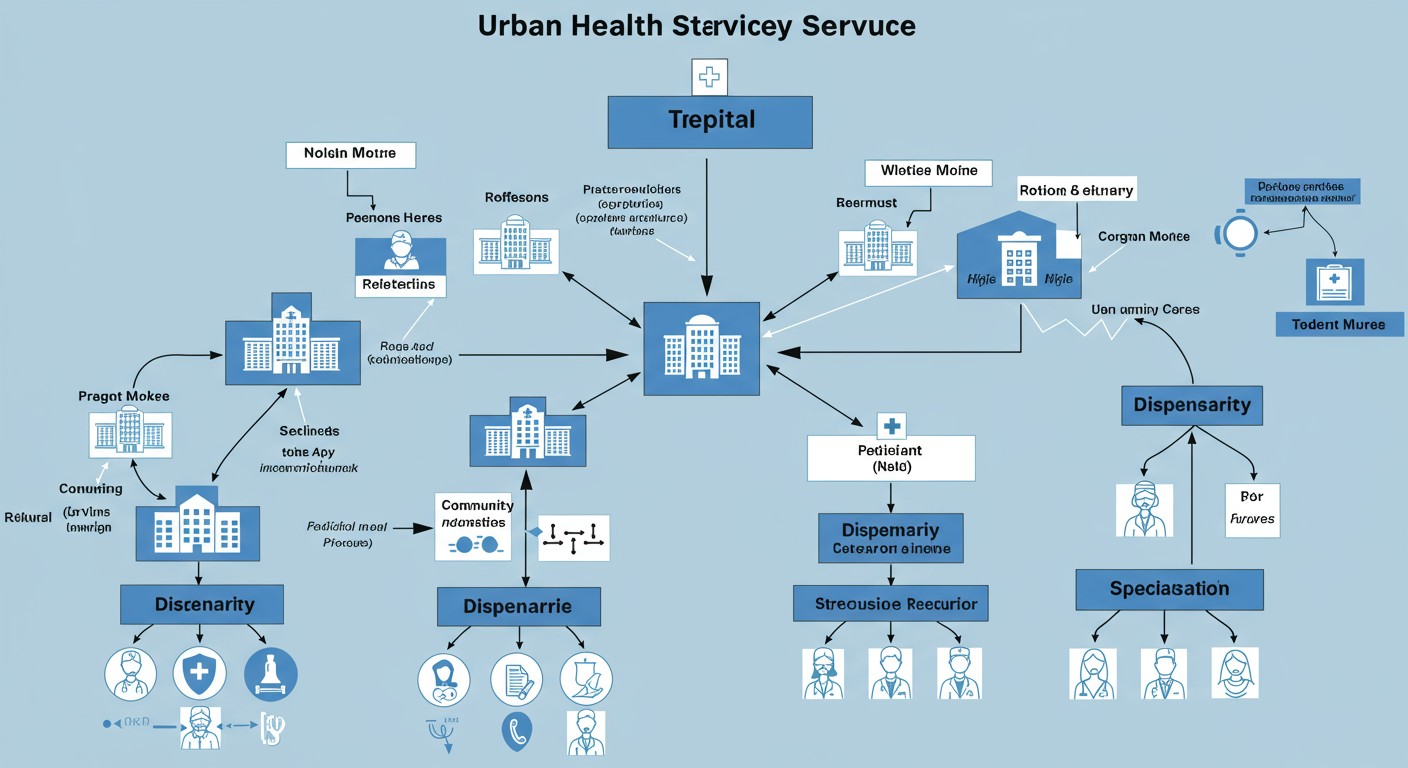
Table of Contents
- 1. Introduction to Urban Health Services Organization
- 2. Urban Health Services in Slum Areas
- 3. Dispensaries Structure and Functions
- 4. Special Clinics in Urban Areas
- 5. Municipal and Corporate Hospitals
- 6. Defense Health Services
- 7. Institutional Health Services
- 8. Best Practices and Recent Updates
1. Introduction to Urban Health Services Organization
Urban health services organization refers to the structured system of healthcare delivery established in urban settings to meet the diverse health needs of city populations. These services are critical in addressing the unique health challenges faced in densely populated urban environments.
Urban areas face distinct health challenges including:
- High population density leading to rapid disease spread
- Environmental pollution affecting respiratory health
- Uneven distribution of healthcare resources
- Diverse socioeconomic conditions creating health disparities
- Limited physical space for healthcare infrastructure
Memory Aid: “SUPER” Urban Health Challenges
- Sanitation issues
- Uneven resource distribution
- Population density
- Environmental hazards
- Resource constraints
2. Urban Health Services in Slum Areas
Slums are heavily polluted urban informal settlements characterized by substandard housing, overcrowding, and inadequate access to safe water, sanitation, and other infrastructure. The government provides various health services specifically tailored to address the unique challenges in these areas.
2.1. Organizational Structure in Slum Health Services
The organizational hierarchy typically follows:
- Urban Local Bodies (Municipal Corporations/Councils) at the top
- Health Department of the Municipal Corporation
- Zonal/Ward Health Officers
- Medical Officers of Primary Urban Health Centers (PUHCs)
- Public Health Nurses, ANMs, ASHAs, and other frontline workers
2.2. Staffing Pattern for Slum Health Services
| Staff Category | Number | Key Responsibilities |
|---|---|---|
| Medical Officer | 1 per 50,000 population | Overall management, clinical services, supervision |
| Public Health Nurse | 1 per 50,000 population | Nursing services coordination, supervision of ANMs |
| ANM (Auxiliary Nurse Midwife) | 1 per 10,000 population | MCH care, immunization, family planning services |
| ASHA (Accredited Social Health Activist) | 1 per 1,000-2,500 population | Community mobilization, health education, referrals |
| Pharmacist | 1 per center | Medication dispensing, inventory management |
| Lab Technician | 1 per center | Basic laboratory tests |
2.3. Functions of Slum Health Services
- Provision of basic primary healthcare services
- Maternal and child health services including antenatal care
- Immunization services for children and pregnant women
- Family planning services and counseling
- Management of common illnesses and minor injuries
- Health education and awareness programs
- Vector control and communicable disease prevention
- Water quality monitoring and sanitation promotion
- Referral services to higher facilities for complicated cases
Nursing Role Highlight
Nurses in slum health services often play multiple roles beyond clinical care, including community health education, data collection for health surveillance, and coordination with various stakeholders for holistic care delivery.
3. Dispensaries Structure and Functions
Urban dispensaries are primary healthcare units that provide basic outpatient services and medications. They serve as the first point of contact for urban residents seeking healthcare, especially in areas without larger facilities.
3.1. Organizational Structure of Urban Dispensaries
Urban dispensaries typically operate under:
- Municipal Corporation/Urban Local Body Health Department
- Medical Officer In-charge (reports to Zonal Health Officer)
- Support staff including nurses, pharmacists, and multi-purpose workers
3.2. Staffing Pattern for Urban Dispensaries
| Staff Category | Number | Key Responsibilities |
|---|---|---|
| Medical Officer | 1-2 | Clinical services, administrative oversight |
| Staff Nurse | 2-4 | Nursing care, dressing, immunization |
| Pharmacist | 1-2 | Medication dispensing, stock management |
| Lab Technician | 0-1 | Basic laboratory tests (if facility available) |
| Multi-purpose Worker | 2-4 | Outreach activities, support services |
| Administrative Staff | 1-2 | Registration, record keeping |
3.3. Functions of Urban Dispensaries
- Provision of basic outpatient services for common illnesses
- Dispensing essential medications
- First aid and emergency care
- Basic diagnostic services (if equipped)
- Immunization services
- Maternal and child health services
- Health education and counseling
- Referral to higher facilities for specialized care
- Maintenance of health records and reporting
Memory Aid: “MEDICS” Functions of Urban Dispensaries
- Medication dispensing
- Emergency first aid
- Diagnostics (basic)
- Immunization services
- Counseling and health education
- Specialist referrals
4. Special Clinics in Urban Areas
Special clinics are specialized healthcare facilities in urban areas that focus on specific health conditions or population groups. These clinics are designed to provide targeted services that may not be available at general dispensaries or primary health centers.
4.1. Types of Special Clinics in Urban Areas
| Type of Special Clinic | Target Population/Condition | Key Services |
|---|---|---|
| Maternal and Child Health Clinics | Pregnant women, infants, children | Antenatal care, postnatal care, growth monitoring, immunization |
| STI/HIV Clinics | Individuals at risk of or with STIs/HIV | Testing, treatment, counseling, prevention education |
| TB and Respiratory Disease Clinics | TB patients, respiratory conditions | Diagnosis, DOTS therapy, follow-up, pulmonary rehabilitation |
| Non-Communicable Disease Clinics | Diabetes, hypertension, CVD patients | Screening, treatment, lifestyle counseling, medication management |
| Mental Health Clinics | Individuals with mental health conditions | Psychiatric assessment, therapy, medication management |
| Geriatric Clinics | Elderly population | Comprehensive geriatric assessment, chronic disease management |
4.2. Staffing Pattern for Special Clinics
The staffing varies based on clinic specialty but generally includes:
- Specialist Medical Officer/Consultant (specific to clinic type)
- Specialized Nursing Staff
- Technicians (lab, radiology, etc. as needed)
- Counselors/Social Workers
- Administrative support staff
- Community Health Workers for outreach
4.3. Functions of Special Clinics
- Specialized diagnostic services relevant to the clinic focus
- Specialized treatment and management protocols
- Follow-up care and case management
- Health education and counseling specific to the condition
- Outreach and screening programs in the community
- Research and data collection on specialized health issues
- Training of healthcare professionals in specialized care
- Advocacy for policies related to the health condition
Critical Nursing Consideration
When working in special clinics, nurses must continuously update their specialized knowledge and skills to provide evidence-based care for the specific conditions addressed by the clinic. Participation in specialized training programs is essential.
5. Municipal and Corporate Hospitals
Municipal and corporate hospitals are larger healthcare facilities that provide comprehensive secondary and sometimes tertiary care services in urban areas. Municipal hospitals are government-owned, while corporate hospitals are privately owned and managed by corporations.
5.1. Organizational Structure of Municipal Hospitals
Municipal hospitals typically follow this hierarchical structure:
- Municipal Corporation/Urban Local Body
- Health Department of Municipal Corporation
- Hospital Administration
- Medical Superintendent/Director
- Deputy Medical Superintendents
- Heads of Various Departments
- Administrative Officer
- Clinical Departments (Medicine, Surgery, Pediatrics, etc.)
- Support Services (Radiology, Laboratory, Pharmacy)
- Administrative Departments (HR, Finance, Maintenance)
5.2. Staffing Pattern for Municipal Hospitals
| Staff Category | Typical Ratio (per 100 beds) | Key Responsibilities |
|---|---|---|
| Medical Staff | 15-25 | Clinical care, procedures, surgeries, consultations |
| Nursing Staff | 45-60 | Patient care, medication administration, monitoring |
| Paramedical Staff | 20-30 | Lab tests, imaging, physiotherapy, etc. |
| Administrative Staff | 10-15 | Administration, records, billing, HR |
| Support Staff | 25-35 | Housekeeping, security, dietary, maintenance |
5.3. Functions of Municipal and Corporate Hospitals
- Comprehensive outpatient and inpatient services
- Emergency and trauma care
- Specialized clinical services across various departments
- Diagnostic services including advanced imaging
- Surgical procedures (major and minor)
- Maternity and child care services
- Critical care and intensive care services
- Pharmacy services
- Blood bank services (in larger hospitals)
- Medical education and training (teaching hospitals)
- Research activities (in some hospitals)
Memory Aid: “COPIERS” Municipal Hospital Functions
- Clinical services (inpatient/outpatient)
- Operations and surgical procedures
- Pharmacy and medication management
- Imaging and diagnostics
- Emergency and trauma care
- Research and education
- Specialized treatment services
6. Defense Health Services
Defense Health Services provide medical care to military personnel, their dependents, and sometimes veterans. These services are managed by the Defense Health Agency (DHA) and are structured to support both combat readiness and general healthcare needs.
6.1. Organizational Structure of Defense Health Services
The typical hierarchical structure includes:
- Defense Health Agency (DHA)
- Service-specific Medical Commands (Army, Navy, Air Force)
- Military Medical Treatment Facilities (MTFs)
- Military Hospitals
- Medical Centers
- Clinics
- Field Medical Units
- Research and Development Facilities
6.2. Staffing in Defense Health Services
| Staff Category | Classification | Key Responsibilities |
|---|---|---|
| Military Medical Officers | Commissioned Officers | Clinical care, medical leadership, combat medical support |
| Military Nursing Corps | Commissioned Officers | Patient care, unit management, field nursing |
| Medical Service Corps | Commissioned Officers | Healthcare administration, logistics, planning |
| Enlisted Medical Personnel | Non-commissioned | Medical assistance, emergency response, technician duties |
| Civilian Healthcare Staff | Federal Employees | Supplementary clinical and support functions |
| Contracted Healthcare Providers | Private Sector | Specialized services, supplementary staffing |
6.3. Functions of Defense Health Services
- Combat casualty care and field medicine
- Primary care services for active duty personnel
- Comprehensive healthcare for military dependents
- Medical readiness maintenance of military forces
- Preventive medicine and health promotion
- Emergency response and disaster relief support
- Medical research focused on military health issues
- Medical training and education for military healthcare providers
- Medical intelligence and biosurveillance
- Global health engagement and humanitarian assistance
Military Nursing Uniqueness
Military nurses have dual responsibilities as both healthcare providers and military officers. They must be prepared for deployment to combat zones, be familiar with battlefield medicine, and understand military protocols and chain of command while maintaining clinical nursing excellence.
7. Institutional Health Services
Institutional health services refer to comprehensive healthcare provided in facilities like nursing homes, long-term care facilities, prison health services, and facilities for those with special needs. These are typically designed for specific populations requiring continuous or specialized care.
7.1. Types of Institutional Health Services
| Type of Institution | Target Population | Primary Services |
|---|---|---|
| Nursing Facilities | Elderly, chronically ill, rehabilitation patients | 24-hour nursing care, rehabilitation, long-term care |
| Mental Health Institutions | Individuals with psychiatric conditions | Psychiatric treatment, therapy, medication management |
| Correctional Health Facilities | Incarcerated individuals | Basic healthcare, mental health, chronic disease management |
| Intermediate Care Facilities | Individuals with intellectual disabilities | Supportive care, skill development, health monitoring |
| Residential Treatment Centers | Substance abuse, behavioral disorders | Detoxification, therapy, rehabilitation |
| Hospice Facilities | Terminal illness patients | End-of-life care, pain management, emotional support |
7.2. Staffing Pattern in Institutional Health Services
Staffing varies by institution type but generally includes:
- Medical Director/Physician (full-time or visiting)
- Director of Nursing
- Registered Nurses (24-hour coverage)
- Licensed Practical/Vocational Nurses
- Certified Nursing Assistants/Aides
- Specialists (based on facility type: psychiatrists, physical therapists, etc.)
- Social Workers
- Activity Directors/Recreational Therapists
- Dietary Staff
- Administrative and Support Staff
Nursing Staff Ratios (varies by institution type and regulations):
| Institution Type | Day Shift Ratio (Nurse:Patients) | Night Shift Ratio (Nurse:Patients) |
|---|---|---|
| Skilled Nursing Facility | 1:15-20 (RN), 1:8-10 (LPN/LVN) | 1:25-30 (RN), 1:15-20 (LPN/LVN) |
| Psychiatric Institution | 1:6-8 (RN), 1:10-12 (LPN/LVN) | 1:10-12 (RN), 1:15-20 (LPN/LVN) |
| Correctional Health | 1:50-100 (varies widely) | 1:100-200 (varies widely) |
| Hospice | 1:4-6 (RN), 1:8-10 (LPN/LVN) | 1:6-8 (RN), 1:10-12 (LPN/LVN) |
7.3. Functions of Institutional Health Services
- 24-hour nursing care and monitoring
- Medication administration and management
- Activities of daily living assistance
- Rehabilitation services
- Nutritional planning and dietary services
- Social and recreational activities
- Psychological and emotional support
- Care coordination with specialists
- Family support and education
- End-of-life care (where applicable)
Memory Aid: “CARE-PLUS” Institutional Health Services Functions
- Continuous monitoring
- Activities of daily living support
- Rehabilitation services
- Emotional and psychological care
- Physical health maintenance
- Long-term planning
- Unified team approach
- Specialized care delivery
8. Best Practices and Recent Updates in Urban Health Services
Best Practice #1: Integrated Urban Health Service Delivery
Recent developments have emphasized the importance of integrated service delivery models in urban settings to address fragmentation of healthcare services. This approach coordinates primary, secondary, and tertiary care through unified health information systems and referral networks.
Key Implementation Strategy: Urban health facilities are increasingly adopting hub-and-spoke models where larger hospitals serve as hubs connected to peripheral primary care centers, special clinics, and community outreach programs, creating a seamless continuum of care.
Best Practice #2: Technology-Enhanced Urban Healthcare
Digital health technologies are revolutionizing urban health service delivery through telemedicine, mobile health applications, electronic health records, and health information exchanges tailored to the urban context.
Key Implementation Strategy: Urban healthcare facilities are implementing virtual consultation systems that allow patients to connect with specialists without physical travel, particularly beneficial in congested urban environments where transportation is challenging and time-consuming.
Best Practice #3: Community Engagement and Participatory Approaches
Recognition of community members as active participants rather than passive recipients of healthcare has led to increased adoption of participatory approaches in urban health service planning and delivery.
Key Implementation Strategy: Formation of Urban Health Resource Groups at the community level that include representatives from resident welfare associations, vulnerable populations, and local healthcare providers to identify health priorities and contribute to service planning and monitoring.
Critical Nursing Consideration for Urban Settings
Nurses working in urban health services must develop cultural competence and adaptability to serve diverse populations with varying beliefs, languages, and health practices concentrated in urban areas. Training in cultural sensitivity and multilingual communication tools is becoming an essential component of urban nursing practice.
References
- World Health Organization. (2022). Strengthening Urban Health Systems. WHO Press.
- Ministry of Health and Family Welfare. (2023). National Urban Health Mission Framework. Government Press.
- Defense Health Agency. (2024). Military Health System Overview. Retrieved from https://www.health.mil/About-MHS/OASDHA/Defense-Health-Agency
- Centers for Medicare & Medicaid Services. (2024). Institutional Long Term Care. Retrieved from https://www.medicaid.gov/medicaid/long-term-services-supports/institutional-long-term-care/index.html
- American Public Health Association. (2023). Urban Health Services: Organization and Delivery Models. APHA Publications.
- Journal of Community Health Nursing. (2024). Special Issue: Nursing in Urban Settings. Vol. 41(2), 115-178.
