Urinary System Management: Community Health Nursing Perspectives
Management of Common Urinary Conditions and Emergencies in Community Health Settings
Introduction to Urinary System Management
Community health nurses play a pivotal role in the prevention, early detection, and management of urinary system disorders. This comprehensive guide focuses on the community health nursing perspective of managing common urinary tract infections (UTIs) and related emergencies in various population groups.
The urinary system, comprising the kidneys, ureters, bladder, and urethra, is vulnerable to various infections and disorders that significantly impact public health. In community settings, nursing interventions focus on prevention, screening, early detection, and timely management of urinary system conditions to reduce complications and hospitalization rates.
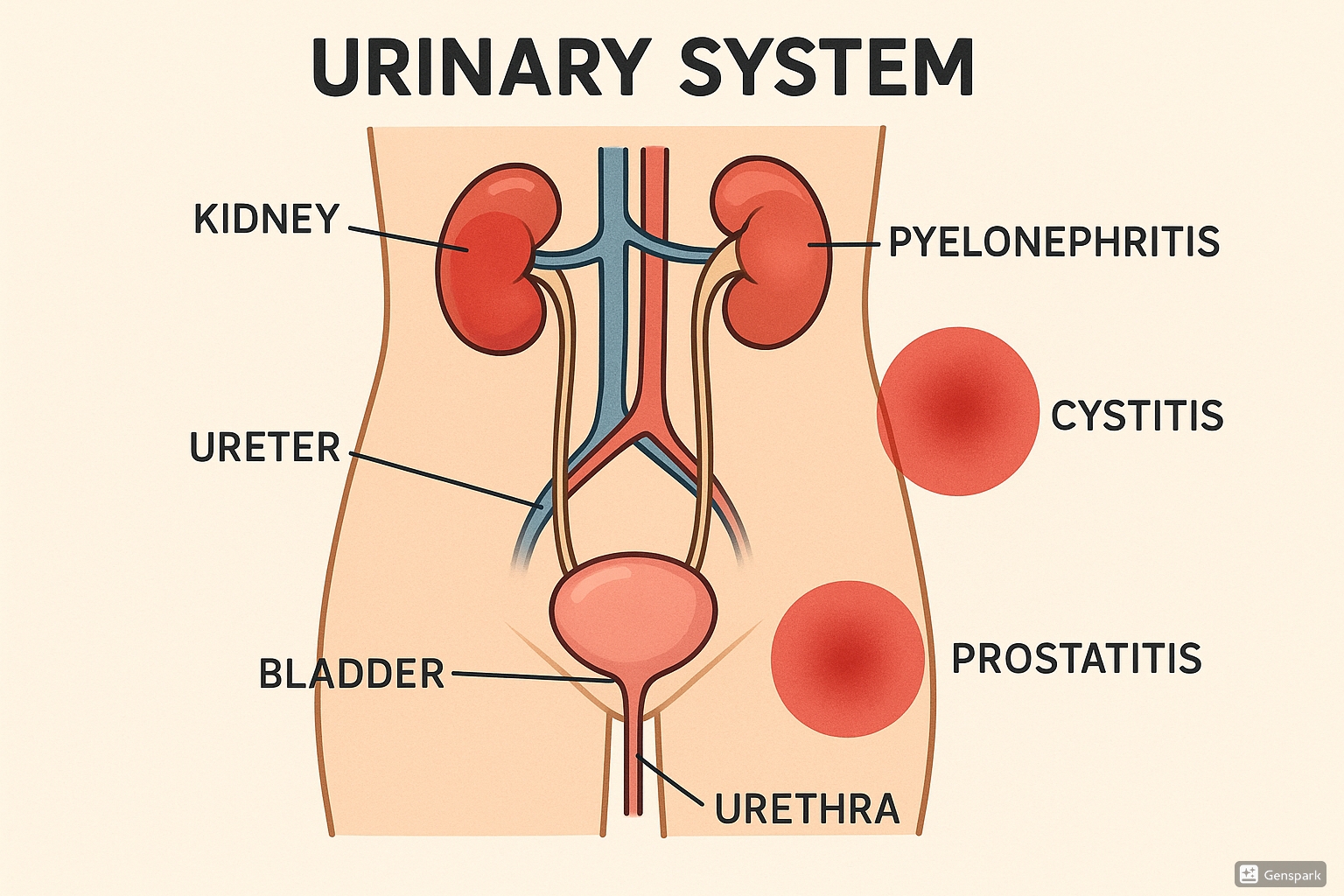
Figure 1: Anatomical representation of the urinary system showing common infection sites including cystitis, pyelonephritis, and prostatitis.
Urinary tract infections are among the most common bacterial infections encountered in community practice, affecting approximately 150 million people worldwide each year. Community health nurses must be proficient in identifying risk factors, recognizing symptoms, and implementing appropriate interventions to manage these infections effectively.
Standing Orders
Definition and Uses
Standing orders are written documents containing rules, policies, procedures, regulations, and protocols for the administration of medications and medical treatments by designated health professionals in specific situations, particularly when a physician is not immediately available.
Key Components of Standing Orders
Standing orders for urinary system conditions typically include:
- Clinical protocols for assessment and diagnosis
- Criteria for initiating treatment
- Specific medication protocols including dosages
- Patient education requirements
- Documentation procedures
- Follow-up and referral guidelines
- Conditions requiring immediate physician notification
In the context of urinary system management, standing orders allow community health nurses to initiate appropriate diagnostic procedures and treatment measures for common urinary infections without delay, particularly in remote or underserved areas where physician access may be limited.
Implementation in Community Settings
Standing orders for urinary tract infections in community settings typically cover:
| Clinical Scenario | Authorized Actions | Parameters for Referral |
|---|---|---|
| Uncomplicated UTI in adult females | Collection of urine sample for dipstick/culture, initiation of empiric antibiotics (e.g., nitrofurantoin, trimethoprim-sulfamethoxazole) | Fever >38°C, flank pain, pregnancy, immunocompromised state |
| Suspected pyelonephritis | Urine and blood sample collection, vital sign monitoring, initial dose of antibiotics | All cases require physician evaluation; hospitalization criteria include severe pain, inability to tolerate oral medications, high fever |
| Pediatric UTI symptoms | Urine collection, preliminary assessment, documentation of symptoms | All suspected pediatric UTIs require physician evaluation |
| Urinary retention | Bladder scanning, straight catheterization if indicated | Retention >500ml, pain, history of recent surgery |
| Recurrent UTI | Urine collection, symptom assessment, review of previous cultures | ≥3 infections in 12 months, treatment failure |
Important Considerations
Standing orders must be:
- Reviewed and approved by institutional authorities
- Updated regularly to reflect current evidence-based guidelines
- Clearly written to avoid misinterpretation
- Accompanied by appropriate training for all implementing staff
- Subject to quality assurance monitoring
Screening and Diagnosis
Screening Methods
Effective community-based screening for urinary system disorders focuses on identifying high-risk populations and implementing appropriate screening protocols. The primary goal is early detection of urinary tract infections and associated conditions to prevent complications.
Population-Based Screening
Community health nurses should prioritize screening for the following high-risk groups:
- Pregnant women (risk of complications affecting both mother and fetus)
- Older adults (especially those with mobility limitations or catheters)
- Individuals with diabetes (due to increased infection susceptibility)
- Persons with neurological conditions affecting bladder function
- Children with history of vesicoureteral reflux or structural abnormalities
- Individuals with recurrent UTI history
Screening Techniques
Common screening methods employed in community settings include:
- Urinary symptom questionnaires
- Dipstick urinalysis (for leukocyte esterase, nitrites, protein, blood)
- Clean-catch midstream urine collection for microscopy and culture
- Post-void residual measurement using portable bladder scanners
- Risk assessment tools for recurrent infections
Diagnostic Tools
URINARY: Mnemonic for UTI Assessment
U – Urination changes (frequency, urgency, hesitancy)
R – Red flags (fever, flank pain, hematuria)
I – Incontinence (new onset or worsening)
N – Nocturia frequency
A – Abdominal/suprapubic pain
R – Risk factors assessment
Y – Yield from previous infections/treatments
Key diagnostic approaches available in community settings include:
| Diagnostic Method | Indicators | Limitations |
|---|---|---|
| Urine Dipstick | Positive for leukocyte esterase and nitrites | Lower sensitivity; false negatives possible |
| Urine Microscopy | >5 WBCs per high power field suggests infection | Requires trained personnel and equipment |
| Urine Culture | Gold standard; >10³ CFU/mL in symptomatic patients | Results delay (24-48 hours); proper collection essential |
| Point-of-Care Testing | Rapid results for nitrite, leukocyte esterase | Variable sensitivity and specificity |
| Symptom Assessment Tools | Standardized questionnaires for symptom evaluation | Subjective; requires patient comprehension |
Diagnostic Criteria for UTI in Community Settings:
- Uncomplicated UTI: Presence of urinary symptoms plus positive dipstick or culture
- Complicated UTI: Symptoms with risk factors (pregnancy, male gender, immunocompromised state, structural abnormalities)
- Recurrent UTI: ≥3 UTIs in 12 months or ≥2 in 6 months
- Asymptomatic bacteriuria: Significant bacteriuria without symptoms (treatment generally not indicated except in pregnancy)
Urinary Tract Infections
Urinary tract infections remain among the most common bacterial infections managed in community health settings. Community health nurses must understand the distinct characteristics, presentation, and management approaches for different types of UTIs.
Cystitis
Cystitis refers to inflammation of the bladder, typically due to bacterial infection. It is the most common form of UTI encountered in community practice, particularly among women.
Clinical Presentation
- Dysuria (painful urination)
- Urinary frequency and urgency
- Suprapubic discomfort or pressure
- Cloudy, malodorous urine, possibly with hematuria
- Low-grade or no fever (high fever suggests upper UTI)
Management in Community Settings
Community health nursing interventions for cystitis include:
- Assessment: Thorough symptom evaluation using standardized tools
- Diagnosis: Urinalysis and possibly culture depending on presentation
- Treatment:
- First-line empiric antibiotics per standing orders and local resistance patterns
- Common options: Nitrofurantoin 100mg BID for 5 days, Trimethoprim-sulfamethoxazole DS BID for 3 days, Fosfomycin 3g single dose
- Symptom management (pain relief, hydration)
- Patient Education:
- Completing full antibiotic course
- Increased fluid intake
- Urination after sexual intercourse
- Proper wiping technique (front to back)
- Warning signs requiring follow-up
- Prevention: Education on preventive measures for recurrent infections
Special Considerations for Cystitis
Recurrent Cystitis: For patients with ≥3 infections per year, consider:
- Post-coital prophylaxis
- Low-dose continuous prophylaxis
- Self-initiated treatment with prescribed antibiotics
- Evaluation for underlying causes
Pyelonephritis
Pyelonephritis is inflammation of the kidney, typically due to bacterial infection that has ascended from the lower urinary tract. It represents a more serious infection requiring prompt intervention.
Clinical Presentation
- Flank pain (unilateral or bilateral)
- Fever (>38°C) and chills
- Nausea and vomiting
- Lower urinary tract symptoms (frequency, urgency, dysuria)
- Costovertebral angle tenderness on examination
- Systemic symptoms (malaise, fatigue)
Management in Community Settings
Community health nursing approach to pyelonephritis:
- Triage: Assess severity and need for hospitalization
- Diagnostic Procedures: Urinalysis, urine culture, and potentially blood tests
- Treatment:
- Mild cases: Oral antibiotics (fluoroquinolones, trimethoprim-sulfamethoxazole) for 7-14 days
- Moderate-severe: Initial parenteral antibiotics, possibly in outpatient setting with close monitoring
- Severe cases: Immediate referral for hospitalization
- Monitoring: Close follow-up at 48-72 hours to assess response
- Education: Importance of completing antibiotics, hydration, fever management
Red Flags for Pyelonephritis
Conditions requiring immediate referral:
- Inability to maintain oral hydration
- Severe pain requiring parenteral analgesia
- Signs of sepsis (hypotension, tachycardia)
- Pregnancy
- Immunocompromised state
- Renal or structural abnormalities
- Failure to improve after 48-72 hours of antibiotics
Prostatitis
Prostatitis involves inflammation of the prostate gland, which may be acute bacterial, chronic bacterial, chronic prostatitis/chronic pelvic pain syndrome, or asymptomatic inflammatory prostatitis.
Clinical Presentation
- Acute Bacterial Prostatitis:
- Sudden onset of fever, chills
- Perineal, suprapubic, or low back pain
- Urinary symptoms (frequency, urgency, dysuria)
- Tender, swollen prostate on examination
- Chronic Bacterial Prostatitis:
- Recurrent UTI symptoms
- Persistent perineal discomfort
- Intermittent obstructive symptoms
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome:
- Pelvic pain without confirmed infection
- Variable urinary symptoms
- Sexual dysfunction
Management in Community Settings
Community health nurses should focus on:
- Acute Bacterial Prostatitis:
- Initial evaluation and prompt referral
- Antibiotics (fluoroquinolones, trimethoprim-sulfamethoxazole) for 2-4 weeks
- Pain management and hydration
- Chronic Forms:
- Coordination with urologists for specialized management
- Longer-term antibiotics for confirmed bacterial cases
- Symptom management for non-bacterial forms
- Patient education and support
Special Considerations for Prostatitis
Community health nursing interventions should include:
- Assessment of impact on quality of life
- Education about chronic nature of some forms
- Support for adherence to long-term treatments
- Consideration of complementary approaches (sitz baths, dietary modifications)
UTIs in Children
Urinary tract infections in children present unique challenges in diagnosis and management due to nonspecific symptoms and potential long-term consequences if not properly treated.
Clinical Presentation by Age Group
| Age Group | Common Presentations | Diagnostic Challenges |
|---|---|---|
| Neonates/Infants (<1 year) | Fever without source, irritability, poor feeding, vomiting, failure to thrive | Nonspecific symptoms, difficult urine collection |
| Toddlers (1-3 years) | Fever, abdominal pain, vomiting, foul-smelling urine, increased urinary frequency | Limited communication, toilet training issues |
| Preschool/School-age (3-12 years) | Dysuria, frequency, urgency, abdominal/flank pain, enuresis | Distinguishing from functional disorders |
| Adolescents | Similar to adults, dysuria, frequency, suprapubic pain | Sexual activity considerations, compliance issues |
Management in Community Settings
Community health nursing interventions for pediatric UTIs include:
- Specimen Collection:
- Clean catch for toilet-trained children
- Catheterization or suprapubic aspiration for non-toilet-trained (typically performed in clinical settings)
- Urine collection bags not recommended for definitive diagnosis due to high contamination rates
- Treatment:
- Prompt antibiotic therapy based on age and clinical presentation
- Duration typically 7-14 days depending on clinical scenario
- Infants <3 months typically require hospitalization
- Follow-up:
- Post-treatment urinalysis to confirm resolution
- Imaging considerations for young children, recurrent infections
- Education on prevention measures
Important Considerations in Pediatric UTIs
- Higher risk of renal scarring in children <5 years
- Evaluation for anatomical abnormalities (vesicoureteral reflux) in young children with first UTI
- Family education crucial for prevention and early recognition
- Prompt referral for febrile UTIs in infants and young children
Primary Care Management
Community health nurses provide vital primary care services for urinary system conditions, focusing on comprehensive care models that encompass prevention, treatment, and long-term management.
Key Components of Primary Care for Urinary Conditions
- Preventive Interventions:
- Education on hydration (2-3 liters daily for most adults)
- Proper hygiene practices
- Cranberry products for those with recurrent UTIs (evidence mixed but low risk)
- Voiding after sexual intercourse
- Management of constipation and proper toileting habits
- Acute Care Protocols:
- Symptom-based assessment algorithms
- Empiric treatment based on local resistance patterns
- Pain and symptom management strategies
- Clear patient instructions for medication adherence
- Chronic Management:
- Surveillance protocols for recurrent infections
- Prophylactic regimens when indicated
- Management of underlying risk factors (e.g., diabetes control)
- Quality of life assessments
PREVENT: UTI Prevention Education Framework
P – Proper wiping technique (front to back)
R – Regular urination (don’t hold urine)
E – Empty bladder completely
V – Void after intercourse
E – Ensure adequate hydration
N – Notify healthcare provider of symptoms early
T – Toilet hygiene maintenance
Patient-Centered Approaches
Community health nursing should employ patient-centered approaches including:
- Shared decision-making for treatment options
- Self-management support with clear action plans
- Cultural competence in education and interventions
- Family involvement, particularly for pediatric and elderly patients
- Consideration of socioeconomic factors affecting adherence and follow-up
Special Populations in Primary Care
| Population | Special Considerations |
|---|---|
| Pregnant Women | Screening for asymptomatic bacteriuria, antibiotic safety profile, increased risk of pyelonephritis |
| Elderly | Atypical presentation (confusion, falls), comorbidities, drug interactions, catheter management |
| Diabetics | Higher infection risk, glycemic control importance, watch for emphysematous complications |
| Immunocompromised | Broader pathogen spectrum, longer treatment duration, lower threshold for culture and follow-up |
| Catheterized Patients | Catheter care education, recognizing CAUTI, minimizing unnecessary catheterization |
Referral Guidelines
Community health nurses must know when conditions require referral to specialists or emergency services. Clear referral pathways ensure timely intervention for complex or severe urinary conditions.
Indications for Urgent/Emergency Referral
- Signs of urosepsis (hypotension, altered mental status, severe tachycardia)
- Acute urinary retention
- Severe flank pain with fever
- Gross hematuria with clots
- Acute kidney injury (rising creatinine)
- UTI in pregnancy with systemic symptoms
- Failed outpatient management (worsening after 48-72 hours)
Indications for Specialist Referral
- Recurrent UTIs (≥3 in 12 months) despite preventive measures
- UTIs associated with stones or anatomical abnormalities
- Complicated UTIs in males
- Persistent hematuria after infection resolution
- Children with recurrent UTIs or febrile infections
- Chronic/recurrent prostatitis
Referral Information Checklist
When referring patients, include:
- Detailed history of current complaint
- Previous UTI history and treatments
- Culture results and antibiotic sensitivities
- Relevant comorbidities
- Current medications
- Imaging results (if available)
- Response to current treatment
- Specific concerns prompting referral
First Aid for Urinary Emergencies
Community health nurses should be equipped to provide first aid for urinary emergencies before definitive medical care can be accessed.
Common Urinary Emergencies
| Emergency | First Aid Management |
|---|---|
| Acute Urinary Retention |
|
| Renal Colic (Kidney Stones) |
|
| Gross Hematuria |
|
| Suspected Urosepsis |
|
| Urinary Trauma |
|
First Aid Kit for Urinary Emergencies in Community Settings
- Urinary dipsticks
- Sterile specimen containers
- Clean-catch instructions and supplies
- Catheterization kit (if authorized)
- Analgesics (per standing orders)
- Antipyretics
- Bladder scanner (if available)
- Documentation forms
Warning Signs Requiring Immediate Medical Attention
Instruct patients and caregivers to seek immediate medical care for:
- High fever (>39°C/102.2°F) with flank pain
- Inability to urinate with bladder distension
- Severe abdominal/flank pain unrelieved by over-the-counter medications
- Gross hematuria with clots
- Signs of shock (hypotension, rapid pulse, confusion)
- Trauma to genitourinary region
Community-Based Interventions
Effective community health nursing extends beyond individual care to population-level interventions for urinary system health.
Health Promotion Programs
- Educational Campaigns: Community awareness programs about UTI prevention
- Targeted Outreach: Programs for high-risk groups (elderly, pregnant women, diabetics)
- School-Based Education: Age-appropriate hygiene and hydration education
- Workplace Programs: Education about hydration and bathroom access in occupational settings
Screening Programs
- Antenatal screening for asymptomatic bacteriuria
- Elderly care facility screening protocols
- Community screening events in high-risk populations
- Home health screening for catheterized patients
Community Resources Development
- Public restroom availability assessment
- Water access initiatives for adequate hydration
- Educational materials in multiple languages
- Support groups for chronic urinary conditions
- Transportation services to urological care for underserved populations
Program Implementation Framework
- Community Assessment: Identify prevalence of urinary conditions and high-risk groups
- Program Planning: Design interventions based on community needs and resources
- Resource Allocation: Secure necessary materials, personnel, and funding
- Implementation: Execute programs with community involvement
- Evaluation: Measure outcomes (reduced UTI rates, increased knowledge, improved care access)
- Refinement: Adjust programs based on evaluation findings
Global Best Practices
Examining global best practices in community management of urinary conditions reveals valuable approaches that can be adapted to diverse settings.
Innovative Approaches from Around the World
Scandinavia: Self-Care Models
Scandinavian countries have implemented successful self-care models for uncomplicated UTIs:
- Pharmacy-based symptom assessment protocols
- Patient-initiated dipstick testing with guidance
- Structured decision trees for self-management vs. seeking care
- Telephone nursing triage for UTI symptoms
These approaches reduce healthcare burden while maintaining quality care.
United Kingdom: Community Antibiotic Stewardship
The UK has pioneered community-based antibiotic stewardship for UTIs:
- Back-up prescriptions for uncertain cases
- Delayed antibiotic strategies with clear symptom thresholds
- Integration of antibiotic resistance data into primary care decision support
- Regular antibiotic prescribing feedback to community practitioners
India: Mobile Health Technologies
In resource-limited settings in India, mobile health technologies support UTI management:
- SMS reminder systems for medication adherence
- Smartphone apps for symptom monitoring and triage
- Telemedicine consultations for rural areas
- Community health worker decision support tools
Australia: Aboriginal Community UTI Programs
Australia has developed culturally appropriate UTI management programs for Aboriginal communities:
- Integration of traditional health beliefs with evidence-based practice
- Community health worker training on UTI prevention
- Pictorial education materials for diverse literacy levels
- Adaptation of screening protocols for remote settings
Canada: Integrated Care Pathways
Canadian healthcare systems have implemented integrated care pathways for UTIs:
- Coordinated management between primary care, pharmacy, and specialist services
- Electronic health record integration of UTI protocols
- Standardized follow-up and referral processes
- Special protocols for rural and First Nations communities
Adapting Global Practices Locally
When adapting global best practices to local contexts, consider:
- Available healthcare infrastructure and resources
- Cultural norms and health beliefs
- Existing healthcare policies and regulations
- Local antibiotic resistance patterns
- Community engagement and participatory approaches
- Sustainability and cost-effectiveness
References
- World Health Organization. (2023). Urinary tract infections (UTIs). https://www.who.int/news-room/fact-sheets/detail/urinary-tract-infections
- Centers for Disease Control and Prevention. (2022). Urinary Tract Infection. https://www.cdc.gov/antibiotic-use/uti.html
- National Institute for Health and Care Excellence. (2022). Urinary tract infection (lower): antimicrobial prescribing. https://www.nice.org.uk/guidance/ng109
- American Urological Association. (2022). Recurrent Uncomplicated Urinary Tract Infections in Women: AUA/CUA/SUFU Guideline. https://www.auanet.org/guidelines/guidelines/recurrent-uti
- European Association of Urology. (2023). Guidelines on Urological Infections. https://uroweb.org/guidelines
- American Academy of Pediatrics. (2021). Urinary Tract Infections in Febrile Infants and Young Children. https://publications.aap.org/pediatrics/article/138/6/e20162982/60266/Reaffirmation-of-AAP-Clinical-Practice-Guideline
- Royal College of Nursing. (2022). Management of lower urinary tract infection in non-pregnant women. https://www.rcn.org.uk/clinical-topics/infection-prevention-and-control/antimicrobial-resistance/antimicrobial-stewardship
- Medina M, Castillo-Pino E. (2019). An introduction to the epidemiology and burden of urinary tract infections. Therapeutic Advances in Urology, 11:3-7.
- Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. (2015). Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5):269-284.
- Hooton TM. (2012). Clinical practice. Uncomplicated urinary tract infection. New England Journal of Medicine, 366(11):1028-1037.
