Comprehensive Nursing Notes: Uterine and Cervical Fibroids and Polyps
Evidence-based nursing education guide for understanding, assessing, and managing patients with gynecological fibroids and polyps
Introduction
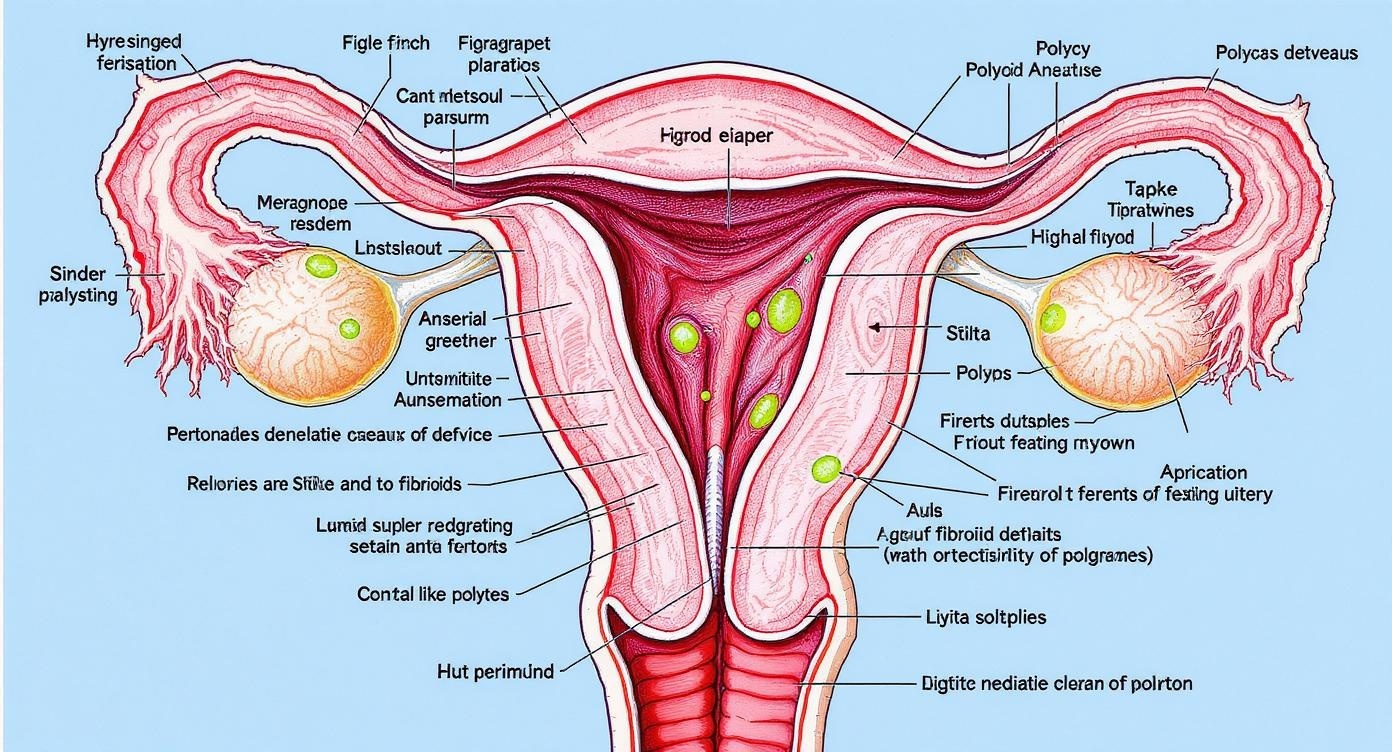
Medical illustration showing uterine and cervical anatomy with fibroids and polyps
Uterine and cervical fibroids and polyps represent some of the most common gynecological conditions encountered in clinical practice. These benign growths affect millions of women worldwide and present unique challenges for healthcare providers, particularly nurses who play a crucial role in patient assessment, education, and ongoing care management.
Understanding the complexity of fibroids and polyps is essential for nursing students preparing to provide comprehensive women’s health care. These conditions can significantly impact a woman’s quality of life, reproductive health, and overall well-being. As a nurse, developing expertise in recognizing symptoms, understanding treatment modalities, and providing compassionate care is fundamental to achieving positive patient outcomes.
Key Learning Objectives
- Differentiate between uterine fibroids and cervical polyps
- Identify risk factors and pathophysiology
- Recognize clinical manifestations and complications
- Understand diagnostic procedures and nursing considerations
- Implement evidence-based nursing interventions
- Provide effective patient education and support
Statistical Overview
Research indicates that uterine fibroids affect approximately 70-80% of women by age 50, with varying degrees of symptoms. Cervical polyps occur in about 2-5% of women, most commonly during reproductive years. Understanding these statistics helps nurses appreciate the widespread impact of these conditions.
Pathophysiology
Uterine Fibroids
Uterine fibroids are benign smooth muscle tumors that develop from the myometrium. The exact etiology remains unclear, but several factors contribute to their development and growth.
- Hormonal influence (estrogen and progesterone)
- Genetic predisposition
- Growth factors (IGF-1, EGF)
- Cellular matrix changes
Cervical Polyps
Cervical polyps are benign growths extending from the cervical canal or ectocervix. They develop through inflammation and hormonal stimulation of the cervical epithelium.
- Chronic cervical inflammation
- Hormonal fluctuations
- Infection or irritation
- Vascular congestion
Memory Aid: FIBROIDS Pathophysiology
F – Factors (hormonal)
I – Inheritance (genetic)
B – Blood supply increased
R – Receptors (estrogen/progesterone)
O – Ovarian hormones
I – IGF-1 growth factors
D – DNA alterations
S – Smooth muscle proliferation
Molecular Mechanisms
The development of fibroids involves complex interactions between steroid hormones, growth factors, and extracellular matrix components. Estrogen and progesterone receptors are overexpressed in fibroid tissue compared to normal myometrium, explaining the hormone-dependent growth patterns observed clinically.
Understanding these mechanisms helps nurses appreciate why fibroids often grow during pregnancy and reproductive years, while typically shrinking after menopause when hormone levels decline.
Types and Classification
Uterine Fibroids Classification
| Type | Location | Characteristics | Clinical Impact |
|---|---|---|---|
| Intramural | Within uterine wall (myometrium) | Most common type (70%), can be multiple | Heavy bleeding, pelvic pressure, enlarged uterus |
| Submucosal | Beneath endometrium, into uterine cavity | Least common (5%), most symptomatic | Heavy menstrual bleeding, infertility, miscarriage |
| Subserosal | Outer uterine surface (serosa) | Can become pedunculated | Pelvic pressure, urinary symptoms, less bleeding |
| Pedunculated | Attached by stalk to uterus | Can twist (torsion), mobile | Acute pain if torsion occurs, mass effect |
Cervical Polyps Classification
Endocervical Polyps
- Arise from endocervical canal
- More common in reproductive age
- Usually smaller and redder
- Glandular epithelium
Ectocervical Polyps
- Arise from ectocervix
- More common in postmenopausal women
- Usually larger and paler
- Squamous epithelium
Memory Aid: POLYPS Classification
P – Position (endo vs ecto)
O – Origin (cervical canal)
L – Location matters
Y – Young (endo) vs old (ecto)
P – Pale (ecto) vs pink (endo)
S – Size varies
Clinical Manifestations
Uterine Fibroids Symptoms
Menstrual Symptoms
- • Menorrhagia (heavy menstrual bleeding)
- • Prolonged menstrual periods
- • Irregular bleeding patterns
- • Clot formation
Pressure Symptoms
- • Pelvic pressure and fullness
- • Urinary frequency or urgency
- • Constipation
- • Back pain
Reproductive Issues
- • Infertility challenges
- • Recurrent pregnancy loss
- • Pregnancy complications
- • Dyspareunia (painful intercourse)
Cervical Polyps Symptoms
Bleeding Manifestations
- • Intermenstrual bleeding
- • Postcoital bleeding
- • Postmenopausal bleeding
- • Spotting between periods
Visible Changes
- • Abnormal vaginal discharge
- • Mucoid or bloody discharge
- • Visible growth on examination
- • Usually asymptomatic if small
Important Note
Many cervical polyps are asymptomatic and discovered incidentally during routine gynecological examinations. This emphasizes the importance of regular screening.
Symptom Severity Assessment
Mild
Minimal impact on daily activities, manageable symptoms
Moderate
Some interference with lifestyle, noticeable symptoms
Severe
Significant impact on quality of life, intervention needed
Memory Aid: HEAVY Bleeding Assessment
H – Heavy flow (>80ml per cycle)
E – Extended duration (>7 days)
A – Anemia development
V – Very large clots
Y – Yearly quality of life impact
Diagnostic Procedures
Comprehensive Diagnostic Approach
| Diagnostic Method | Purpose | Nursing Considerations | Advantages |
|---|---|---|---|
| Pelvic Examination | Initial assessment, detect masses | Ensure privacy, explain procedure, positioning | Non-invasive, immediate results |
| Transvaginal Ultrasound | Visualize fibroids, measure size/location | Empty bladder, explain probe insertion | High resolution, real-time imaging |
| Hysteroscopy | Direct visualization of uterine cavity | Pre-procedure preparation, monitor vitals | Can treat while diagnosing |
| MRI | Detailed anatomy, surgical planning | Screen for metal, claustrophobia assessment | Excellent soft tissue contrast |
| Endometrial Biopsy | Rule out malignancy | Pain management, infection prevention | Tissue diagnosis |
Laboratory Tests
-
Complete Blood Count (CBC)
Assess for anemia secondary to heavy bleeding
-
Iron Studies
Evaluate iron deficiency status
-
Pregnancy Test
Rule out pregnancy before procedures
-
Thyroid Function
Assess for underlying endocrine disorders
Pre-Procedure Nursing Care
-
Patient Education
Explain procedure, risks, benefits
-
Informed Consent
Ensure understanding and documentation
-
Baseline Assessment
Vital signs, allergies, medical history
-
Emotional Support
Address anxiety and concerns
Memory Aid: EXAMINE Diagnostic Process
E – Examine physically first
X – X-ray studies (ultrasound)
A – Assess blood work
M – MRI for detailed view
I – Investigate with scope
N – Note patient concerns
E – Educate throughout process
Treatment Options
Treatment Approaches for Fibroids
Medical Management
- Hormonal contraceptives
- GnRH agonists
- Tranexamic acid
- NSAIDs for pain
- Iron supplementation
Minimally Invasive
- Uterine artery embolization
- Focused ultrasound
- Laparoscopic myomectomy
- Hysteroscopic resection
- Radiofrequency ablation
Surgical Options
- Abdominal myomectomy
- Hysterectomy (total/partial)
- Robotic-assisted surgery
- Endometrial ablation
- Emergency procedures
Cervical Polyps Treatment
| Treatment Method | Procedure | Nursing Care | Recovery |
|---|---|---|---|
| Simple Polypectomy | Twist and remove with forceps | Position, assist, monitor bleeding | Minimal, same-day discharge |
| Electrocautery | Burn base with electrical current | Ensure grounding, ventilation | 1-2 weeks healing |
| Laser Removal | Precise tissue ablation | Eye protection, assist positioning | Quick healing, minimal scarring |
| Cryotherapy | Freeze tissue with liquid nitrogen | Monitor for vasovagal response | 2-3 weeks with discharge |
Treatment Decision Factors
Patient Factors
- Age and fertility desires
- Symptom severity
- Medical comorbidities
- Quality of life impact
Clinical Factors
- Size and location
- Number of lesions
- Risk of malignancy
- Response to previous treatment
Memory Aid: TREAT Decision Making
T – Try conservative first
R – Review patient preferences
E – Evaluate risks vs benefits
A – Assess fertility needs
T – Timing considerations
Nursing Assessment
Comprehensive Health History
Menstrual History
- • Age of menarche and menopause
- • Cycle length and regularity
- • Flow characteristics and duration
- • Associated pain or discomfort
Reproductive History
- • Pregnancy and delivery history
- • Contraceptive use
- • Fertility concerns or treatments
- • Previous gynecological surgeries
Family History
- • Fibroids in family members
- • Gynecological cancers
- • Genetic disorders
- • Hormonal conditions
Physical Assessment Focus
General Appearance
- • Signs of anemia (pallor, fatigue)
- • Body mass index assessment
- • Overall comfort level
- • Emotional state and anxiety
Abdominal Assessment
- • Inspection for distension
- • Palpation for masses
- • Percussion for organ boundaries
- • Auscultation for bowel sounds
Vital Signs Monitoring
- • Blood pressure variations
- • Heart rate and rhythm
- • Temperature monitoring
- • Respiratory assessment
Pain Assessment Tools
| Assessment Tool | Description | Best Used For | Nursing Application |
|---|---|---|---|
| Numeric Rating Scale | 0-10 pain intensity scale | Adults, baseline measurement | Quick assessment, trending |
| Wong-Baker FACES | Facial expressions showing pain levels | Pediatric, cognitive impairment | Easy visualization, cultural sensitivity |
| Visual Analog Scale | 10cm line marking pain intensity | Research, precise measurement | Detailed pain tracking |
| PQRST Method | Provocation, Quality, Region, Severity, Timing | Comprehensive pain assessment | Complete pain characterization |
Nursing Diagnosis Priorities
- 1.Acute/Chronic Pain related to fibroid pressure
- 2.Risk for Deficient Fluid Volume related to bleeding
- 3.Activity Intolerance related to anemia
- 4.Anxiety related to diagnosis and treatment
- 5.Ineffective Coping related to chronic symptoms
Assessment Red Flags
- Sudden severe pelvic pain
- Heavy bleeding with hemodynamic instability
- Rapid growth of fibroids
- Postmenopausal bleeding
- Signs of urinary obstruction
Memory Aid: ASSESS Systematic Approach
A – Appearance and comfort
S – Symptoms and severity
S – Systems review (GU, GI)
E – Emotional state
S – Support systems
S – Safety concerns
Nursing Interventions
Pain Management
-
Pharmacological
NSAIDs, acetaminophen, prescribed analgesics
-
Non-pharmacological
Heat therapy, positioning, relaxation techniques
-
Timing
Regular assessment, proactive management
Bleeding Management
-
Monitoring
Track bleeding patterns, pad counts, vital signs
-
Iron Therapy
Oral iron supplements, dietary counseling
-
Emergency Prep
Know when to escalate, IV access readiness
Emotional Support
-
Active Listening
Validate concerns, encourage expression
-
Support Groups
Connect with other women, online resources
-
Coping Strategies
Stress management, mindfulness techniques
Pre and Post-Procedure Care
| Phase | Key Interventions | Monitoring Parameters | Patient Education |
|---|---|---|---|
| Pre-procedure | NPO status, consent, baseline assessment | Vital signs, labs, anxiety level | Procedure explanation, expectations |
| Immediate Post | Recovery position, comfort measures | Vital signs, bleeding, pain level | Normal recovery expectations |
| Ongoing | Activity progression, symptom management | Functional status, complications | Self-care instructions, follow-up |
| Discharge | Written instructions, prescriptions | Stable vital signs, understanding | Warning signs, when to call |
Evidence-Based Nursing Interventions for Fibroids
Symptom Management
- Regular menstrual cycle tracking
- Nutritional counseling for anemia prevention
- Exercise recommendations within limits
- Sleep hygiene education
Quality of Life
- Work accommodation discussions
- Sexual health counseling
- Family planning discussions
- Body image support
Memory Aid: NURSING Intervention Framework
N – Note symptoms and patterns
U – Understand patient concerns
R – Relieve pain and discomfort
S – Support emotional needs
I – Implement safety measures
N – Navigate care coordination
G – Guide patient education
Patient Education
Understanding the Condition
What are Fibroids?
Explain in simple terms that fibroids are non-cancerous growths in the uterus that are very common and usually not dangerous.
- • Use visual aids and diagrams
- • Emphasize benign nature
- • Address cancer concerns
Why Do They Occur?
- • Hormonal influences (estrogen/progesterone)
- • Genetic predisposition
- • Age and reproductive factors
- • Lifestyle considerations
Self-Monitoring Techniques
Menstrual Tracking
- • Use calendar or mobile apps
- • Record flow intensity and duration
- • Note associated symptoms
- • Track pain levels
Symptom Recognition
- • Increased bleeding patterns
- • New or worsening pain
- • Pressure symptoms
- • Changes in urination
Lifestyle Modifications
Dietary Recommendations
- Iron-rich foods for anemia prevention
- Increase fiber intake
- Limit processed foods
- Stay well hydrated
- Consider calcium supplements
Exercise Guidelines
- Regular moderate exercise
- Avoid high-impact during heavy periods
- Yoga and stretching
- Swimming for low impact
- Listen to your body
Stress Management
- Relaxation techniques
- Adequate sleep (7-9 hours)
- Mindfulness meditation
- Support system utilization
- Professional counseling if needed
When to Seek Medical Attention
Immediate Medical Attention Required
- Severe, sudden pelvic pain
- Heavy bleeding with dizziness
- Signs of infection (fever, chills)
- Inability to urinate
- Fainting or severe weakness
- Pregnancy concerns
Follow-up Care Schedule
Regular Monitoring
- Annual gynecological exams
- 6-month imaging if symptomatic
- Blood work as recommended
- Symptom log review
Special Circumstances
- Pre-conception counseling
- Pregnancy monitoring
- Menopause transition
- Post-treatment follow-up
Memory Aid: EDUCATE Patient Framework
E – Explain condition clearly
D – Demonstrate self-care techniques
U – Understand patient concerns
C – Clarify misconceptions
A – Assess understanding
T – Teach warning signs
E – Encourage questions
Complications
Acute Complications
Torsion of Pedunculated Fibroids
- • Sudden severe pelvic pain
- • Nausea and vomiting
- • Requires emergency surgery
- • Risk of tissue necrosis
Hemorrhage
- • Severe menorrhagia
- • Hemodynamic instability
- • May require transfusion
- • Emergency hysterectomy risk
Degeneration
- • Red degeneration in pregnancy
- • Acute pain and tenderness
- • Fever and leukocytosis
- • Conservative management usually
Chronic Complications
Anemia
- • Iron deficiency anemia
- • Fatigue and weakness
- • Reduced quality of life
- • May require iron infusion
Reproductive Issues
- • Infertility challenges
- • Recurrent pregnancy loss
- • Pregnancy complications
- • Need for fertility treatments
Pressure Effects
- • Urinary frequency/retention
- • Constipation and bloating
- • Pelvic pressure and pain
- • Lower back pain
Pregnancy-Related Complications
| Trimester | Potential Complications | Nursing Monitoring | Management Approach |
|---|---|---|---|
| First Trimester | Miscarriage risk, pain from growth | Pain assessment, bleeding monitoring | Conservative, pain management |
| Second Trimester | Red degeneration, placental issues | Fetal monitoring, maternal vitals | Bed rest, analgesia, monitoring |
| Third Trimester | Preterm labor, malpresentation | Contraction monitoring, fetal position | Delivery planning, cesarean preparation |
| Delivery | Obstructed labor, hemorrhage | Labor progress, blood loss | Cesarean delivery often required |
Malignant Transformation Risk
While extremely rare (less than 1%), leiomyosarcoma can develop within or appear similar to fibroids.
Warning Signs:
- • Rapid growth, especially postmenopause
- • New onset symptoms after menopause
- • Unusual imaging characteristics
- • Family history of sarcomas
Prevention Strategies
- Regular gynecological screening
- Early symptom recognition
- Prompt medical evaluation
- Adherence to treatment plans
- Lifestyle modifications
Memory Aid: DANGER Signs Assessment
D – Degeneration pain
A – Anemia from bleeding
N – Necrosis risk
G – Growth abnormalities
E – Emergency surgery needs
R – Reproductive complications
Global Best Practices
International Healthcare Approaches
Nordic Countries Model
- Comprehensive screening programs
- Multidisciplinary care teams
- Patient-centered decision making
- Strong primary care integration
- Evidence-based treatment protocols
Canadian Healthcare System
- Universal healthcare access
- Standardized treatment guidelines
- Quality improvement initiatives
- Nurse practitioner-led clinics
- Focus on minimally invasive techniques
UK National Health Service
- NICE guidelines implementation
- Structured patient pathways
- Regular audit and monitoring
- Specialist nurse training programs
- Patient safety initiatives
Innovative Treatment Centers
| Institution/Country | Innovation | Nursing Role | Patient Outcomes |
|---|---|---|---|
| Mayo Clinic, USA | Integrated care model with focused ultrasound | Specialized fibroid nurses, patient navigators | Reduced hospital stays, improved satisfaction |
| Netherlands Cancer Institute | Robotic-assisted surgery protocols | Advanced technology training, perioperative care | Faster recovery, minimal complications |
| Singapore General Hospital | AI-assisted diagnosis and treatment planning | Technology integration, data management | Improved diagnostic accuracy, personalized care |
| Charité Hospital, Germany | Multidisciplinary tumor boards for complex cases | Care coordination, patient advocacy | Optimized treatment decisions, reduced delays |
Emerging Technologies
Artificial Intelligence
AI-powered imaging analysis improving fibroid detection and treatment planning accuracy by up to 30%.
Telemedicine Integration
Remote monitoring and consultation reducing travel burden while maintaining care quality.
Precision Medicine
Genetic testing informing personalized treatment approaches and risk stratification.
International Nursing Education
Australia
Specialized women’s health nursing programs with hands-on clinical rotations in fibroid centers.
Japan
Integration of traditional and modern approaches with emphasis on holistic patient care.
Brazil
Community-based education programs addressing cultural factors in fibroid management.
Key Lessons from Global Practices
System-Level Improvements
- Standardized care pathways reduce variation
- Multidisciplinary teams improve outcomes
- Quality metrics drive continuous improvement
- Patient engagement enhances satisfaction
Nursing Practice Enhancement
- Specialized training improves competency
- Technology integration streamlines care
- Cultural competency addresses diverse needs
- Continuous education maintains standards
International Collaboration Opportunities
Global nursing organizations are creating opportunities for knowledge exchange and best practice sharing in women’s health care.
- International nursing exchanges
- Virtual learning collaboratives
- Research partnership programs
- Certification standardization efforts
Conclusion
Understanding uterine and cervical fibroids and polyps is fundamental to providing excellent nursing care in women’s health. These conditions, while common and typically benign, can significantly impact a woman’s quality of life, reproductive health, and emotional well-being. As nursing professionals, our role extends beyond basic care to encompass comprehensive assessment, patient education, emotional support, and advocacy.
The complexity of fibroids and polyps requires nurses to maintain current knowledge about diagnostic procedures, treatment options, and evidence-based interventions. From recognizing early symptoms to supporting patients through surgical procedures and long-term management, nursing care must be holistic, culturally sensitive, and patient-centered.
Global best practices demonstrate that standardized care pathways, multidisciplinary collaboration, and continuous quality improvement lead to better patient outcomes. As the healthcare landscape evolves with new technologies and treatment modalities, nurses must adapt their practice while maintaining the core principles of compassionate, evidence-based care.
Key Takeaways for Nursing Practice
- Early recognition of symptoms improves outcomes
- Patient education empowers informed decision-making
- Holistic assessment addresses all patient needs
- Cultural competency enhances care delivery
- Continuous learning maintains professional competence
Future Directions in Care
- Precision medicine approaches
- Minimally invasive treatment options
- Telemedicine integration
- AI-assisted diagnosis and monitoring
- Enhanced patient engagement tools
Final Thoughts for Nursing Students
As you develop your expertise in caring for women with fibroids and polyps, remember that each patient is unique. While evidence-based practice guides our interventions, the art of nursing lies in adapting care to meet individual needs, preferences, and circumstances.
Your role as a nurse extends beyond the clinical setting. You are an educator, advocate, and source of support during challenging times. The trust patients place in you is both a privilege and a responsibility that requires ongoing commitment to excellence.
Continue to seek learning opportunities, stay current with research, and most importantly, never underestimate the impact of compassionate, knowledgeable nursing care on patient outcomes and experiences.
Professional Development Resources
Professional Organizations
- • Association of Women’s Health, Obstetric and Neonatal Nurses (AWHONN)
- • International Association of Healthcare Central Service Material Management
- • Society of Gynecologic Nurse Oncologists
Continuing Education
- • Specialty certification programs
- • Conference presentations and workshops
- • Peer-reviewed journal subscriptions
- • Online learning modules and webinars
