Utilizing Community Resources for Client and Family Care
A comprehensive guide for nursing students on connecting clients with essential community services and support systems
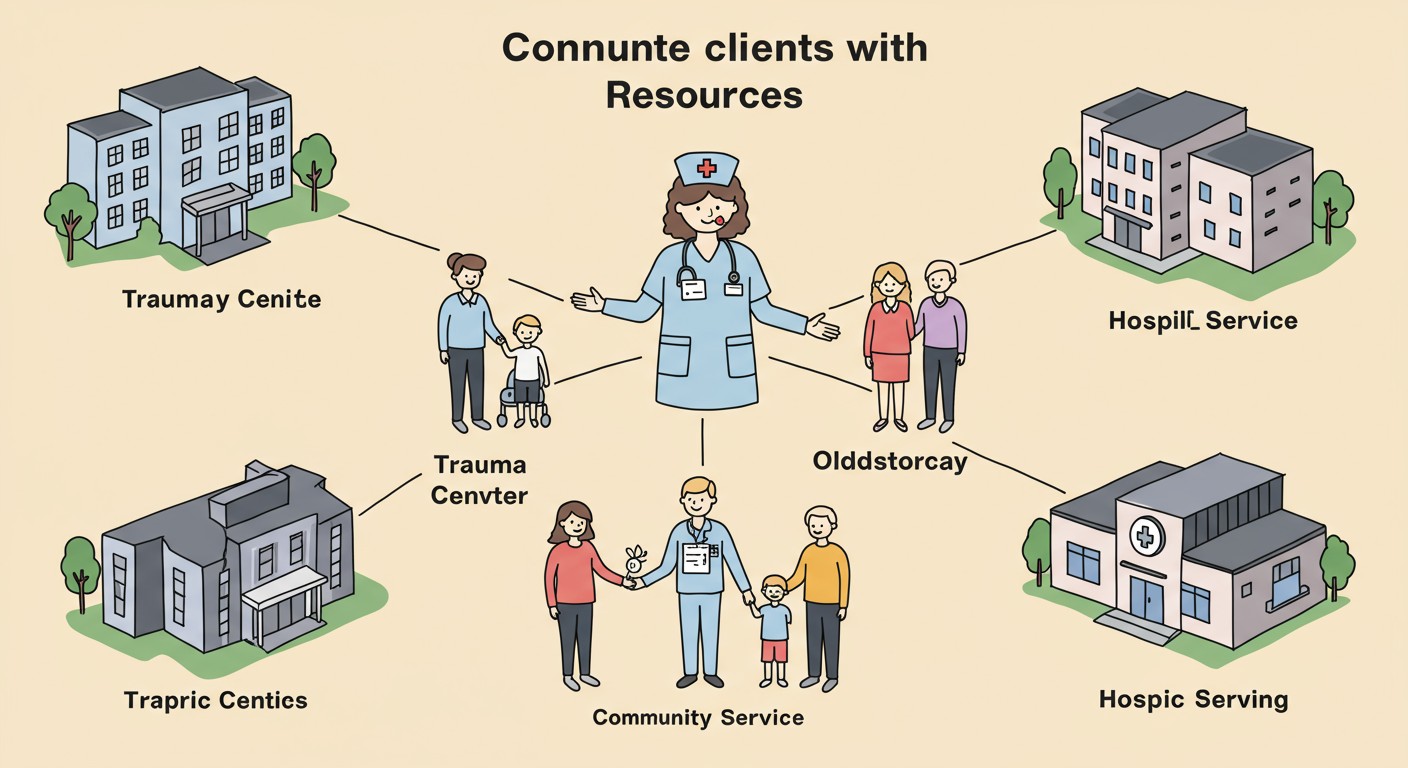
A nurse facilitating connections between families and community resources
Table of Contents
Introduction to Community Resources
Community resources represent a network of services and support systems designed to enhance the well-being of individuals and families. As community health nurses, understanding and effectively utilizing these resources is fundamental to providing holistic care. These resources bridge gaps in healthcare delivery, extending support beyond clinical settings into the everyday lives of clients.
The strategic utilization of community resources enables nurses to address the complex needs of clients that extend beyond medical treatment. These resources become vital components in care plans, particularly for vulnerable populations such as the elderly, orphaned children, physically challenged individuals, and those requiring end-of-life care.
Key Benefits of Community Resource Utilization
- Extends the continuum of care beyond hospital walls
- Addresses social determinants of health
- Reduces healthcare costs through preventative measures
- Promotes client independence and quality of life
- Provides specialized care for specific population needs
- Creates support networks for families and caregivers
Mnemonic: “RESOURCE”
Remember this mnemonic to identify key elements when assessing community resource needs:
- R – Recognize client needs and limitations
- E – Evaluate available community supports
- S – Support systems (family, social networks)
- O – Optimize independence and functioning
- U – Understand financial and access barriers
- R – Refer to appropriate specialized services
- C – Coordinate care across multiple providers
- E – Educate clients and families about resources
Trauma Services
Trauma services constitute critical community resources designed to address both physical and psychological trauma. These services encompass emergency response systems, rehabilitation centers, and psychological support networks that collectively facilitate recovery and reintegration.
Components of Trauma Services
| Service Type | Function | Nursing Role |
|---|---|---|
| Crisis Intervention Centers | Immediate psychological support and stabilization | Assessment, triage, emotional support, referrals |
| Trauma Rehabilitation Services | Physical and occupational therapy for trauma survivors | Rehabilitation nursing, progress monitoring, family education |
| Domestic Violence Shelters | Safe housing and support for abuse survivors | Safety planning, health assessment, community connection |
| Sexual Assault Response Teams | Coordinated response to sexual violence | Forensic examination, emotional support, follow-up care |
| Support Groups | Peer-based emotional support and coping strategies | Facilitation, health education, progress monitoring |
Nursing Assessment for Trauma Service Needs
When assessing clients who may benefit from trauma services, consider these key indicators:
Physical Indicators
- Unexplained injuries or inconsistent explanations
- Delays in seeking medical treatment
- Physical injuries in various healing stages
- Somatic complaints without medical cause
- Sleep disturbances and physical exhaustion
Psychological Indicators
- Hypervigilance or exaggerated startle response
- Emotional numbness or detachment
- Recurrent intrusive thoughts or flashbacks
- Avoidance behaviors related to trauma reminders
- Persistent negative emotional states
“Effective trauma services must address both the visible and invisible wounds. As community health nurses, we serve as vital bridges connecting trauma survivors with the multifaceted resources they need for holistic recovery.”
Old Age Homes
Old age homes represent essential community resources providing residential care for elderly individuals who require varying levels of support. These facilities offer alternatives when family care is unavailable or insufficient to meet complex geriatric needs.
Independent Living
Designed for seniors who require minimal assistance with daily activities.
- Private apartments or cottages
- Communal dining options
- Social and recreational activities
- Emergency response systems
- Limited housekeeping support
Assisted Living
Supports seniors who need regular assistance but not constant nursing care.
- Medication management
- Personal care assistance
- Meals and housekeeping
- Transportation services
- 24-hour supervision
Skilled Nursing Facilities
Provides comprehensive medical care for complex health needs.
- 24-hour nursing supervision
- Rehabilitation services
- Chronic disease management
- Wound care and specialized treatments
- End-of-life care
Nursing Considerations for Old Age Home Referrals
| Assessment Area | Key Considerations | Nursing Actions |
|---|---|---|
| Functional Capacity | ADL/IADL performance, mobility status, fall risk | Conduct standardized assessments (Barthel Index, Katz Index) |
| Cognitive Status | Memory function, decision-making capacity, safety awareness | Perform MMSE, Montreal Cognitive Assessment |
| Social Support | Family availability, caregiver burden, isolation risk | Map social networks, assess caregiver strain |
| Financial Resources | Insurance coverage, personal assets, eligibility for assistance | Connect with social workers, financial counselors |
| Cultural Preferences | Language, dietary needs, religious practices, cultural norms | Culturally sensitive facility matching |
Mnemonic: “ELDERS”
Use this mnemonic to guide comprehensive assessment when facilitating old age home placement:
- E – Evaluate functional abilities and limitations
- L – Living preferences and environment needs
- D – Determine cognitive and psychological status
- E – Explore financial resources and constraints
- R – Review medical conditions and care requirements
- S – Social support assessment and involvement
Orphanages
Orphanages serve as vital community resources providing care, shelter, and developmental support for children who have lost parents or cannot remain with their biological families. Modern orphanages have evolved into multifaceted childcare institutions addressing physical, emotional, educational, and social needs.
Types of Child Care Institutions
Conventional Orphanages
- Residential care for larger groups of children
- Structured daily routines and activities
- On-site educational facilities
- Communal living arrangements
- Often operated by religious organizations or NGOs
Group Homes
- Smaller residential settings (8-12 children)
- Family-like environment with consistent caregivers
- Integration with community schools
- Focus on individualized care plans
- Preparation for independent living
SOS Children’s Villages
- Family-based care model with SOS mother
- Siblings kept together when possible
- Individual houses within village community
- Long-term stability and attachment
- Community integration and support
Transitional Homes
- Temporary care during family crisis
- Goal of family reunification when possible
- Intensive family therapy and support
- Case management services
- Limited duration of stay
Community Health Nursing Role in Orphanage Settings
| Area of Responsibility | Nursing Interventions | Expected Outcomes |
|---|---|---|
| Health Assessment & Screening |
|
Early identification of health issues, complete immunization, appropriate growth trajectory |
| Health Education |
|
Improved health literacy, reduced communicable disease, better self-care practices |
| Mental Health Support |
|
Reduced trauma symptoms, improved emotional regulation, healthy attachment formation |
| Community Integration |
|
Successful school integration, development of community ties, preparation for independent living |
Nursing Assessment Framework for Children in Orphanages
When assessing and planning care for children in orphanages, apply this comprehensive framework:
Physical Domain
- Growth parameters (height, weight, BMI)
- Nutritional status and dietary patterns
- Sleep patterns and quality
- Physical activity levels
- Chronic health conditions
- Dental health status
Psychosocial Domain
- Attachment patterns and behaviors
- Peer relationships and social skills
- Emotional regulation capabilities
- Behavioral concerns and triggers
- Trauma history and responses
- Cultural and identity development
Developmental Domain
- Developmental milestones achievement
- Educational progress and needs
- Language development
- Fine and gross motor skills
- Cognitive functioning
- Life skills development
Homes for Physically Challenged Individuals
Residential facilities for physically challenged individuals represent specialized community resources designed to provide accessible living environments and comprehensive support services. These facilities enable independent living while addressing unique mobility, sensory, or physical limitations.
Types of Facilities for Physically Challenged Individuals
Accessible Independent Living Communities
Designed for individuals who maintain significant independence but require physical accommodations.
- Barrier-free architectural design
- Modified appliances and fixtures
- Emergency response systems
- Accessible community spaces
- Transportation services
Supported Living Facilities
Provides regular assistance with daily activities while promoting maximum independence.
- Personal care assistance
- Medication management
- Therapeutic services on-site
- Adaptive equipment training
- Life skills development
Specialized Care Centers
Comprehensive care for individuals with complex physical disabilities requiring specialized intervention.
- 24-hour nursing care
- Respiratory support services
- Specialized feeding assistance
- Positioning and mobility programs
- Multidisciplinary care team
Transitional Living Centers
Short-term residential support for rehabilitation and adaptation to disability.
- Intensive rehabilitation therapies
- Adaptive technology training
- Environmental assessment
- Community reintegration planning
- Caregiver training programs
Nursing Assessment and Intervention Framework
| Assessment Domain | Key Assessment Parameters | Nursing Interventions |
|---|---|---|
| Functional Mobility |
|
|
| Activities of Daily Living |
|
|
| Skin Integrity |
|
|
| Psychosocial Wellbeing |
|
|
Mnemonic: “ACCESS”
Use this mnemonic when planning care for physically challenged individuals:
- A – Assess functional abilities and limitations
- C – Coordinate multidisciplinary services
- C – Customize environment for independence
- E – Educate on adaptive techniques
- S – Support psychosocial adjustment
- S – Strengthen community connections
Homes for Destitute
Homes for the destitute represent critical community resources providing shelter, basic necessities, and rehabilitation services for individuals experiencing homelessness, extreme poverty, or social abandonment. These facilities address immediate survival needs while working toward long-term stability and reintegration.
Types of Destitute Homes
-
●
Emergency Shelters:
Temporary accommodations providing immediate shelter, basic meals, and hygiene facilities for individuals in crisis.
-
●
Transitional Housing:
Medium-term residential programs (6-24 months) with case management, life skills training, and employment assistance.
-
●
Permanent Supportive Housing:
Long-term housing with ongoing support services for chronically homeless individuals with disabilities or complex needs.
-
●
Rehabilitation Centers:
Structured residential programs addressing addiction recovery, mental health stabilization, and vocational training.
-
●
Night Shelters:
Overnight accommodations providing basic sleeping arrangements, typically operating during evening and early morning hours.
Population Characteristics
Destitute homes serve diverse populations with complex needs, often including:
Homeless Individuals
- Chronically homeless
- Recently displaced
- Economic hardship cases
Mental Health Concerns
- Untreated psychiatric conditions
- Post-traumatic stress
- Dual diagnosis cases
Vulnerable Populations
- Abandoned elderly
- Victims of violence
- Human trafficking survivors
Social Displacement
- Migrant workers
- Disaster-displaced individuals
- Social abandonment cases
Community Health Nursing Roles in Destitute Homes
| Nursing Function | Key Interventions | Challenges | Best Practices |
|---|---|---|---|
| Health Assessment |
|
|
|
| Medication Management |
|
|
|
| Health Education |
|
|
|
| Referral Coordination |
|
|
|
Critical Health Issues in Destitute Populations
Communicable Diseases
- Tuberculosis
- Hepatitis A, B, C
- HIV/AIDS
- Skin infestations (scabies, lice)
- Respiratory infections
- Gastrointestinal infections
Chronic Conditions
- Uncontrolled diabetes
- Hypertension
- COPD and asthma
- Untreated dental disease
- Musculoskeletal disorders
- Malnutrition and deficiencies
Mental Health Issues
- Depression and anxiety
- Schizophrenia spectrum disorders
- Substance use disorders
- Post-traumatic stress disorder
- Cognitive impairments
- Suicide risk
Mnemonic: “SHELTER”
Use this mnemonic when assessing and planning care for destitute populations:
- S – Safety assessment (physical, psychological)
- H – Health status evaluation (acute and chronic)
- E – Environmental factors assessment
- L – Legal/documentation needs
- T – Treatment adherence support
- E – Emotional and mental health
- R – Resource connection and referrals
Palliative Care Centers
Palliative care centers represent specialized community resources focused on improving quality of life for individuals with serious, chronic, or life-limiting illnesses. These centers provide comprehensive symptom management, psychosocial support, and care coordination across various settings.
Core Principles of Palliative Care
Holistic Approach
Addresses physical, emotional, social, and spiritual dimensions of illness experience through interdisciplinary collaboration.
Patient & Family Centered
Focuses on patient-defined goals of care while recognizing family as an integral part of the support system and care planning process.
Early Integration
Initiated at diagnosis of serious illness, operating concurrently with curative treatments to optimize quality of life throughout disease trajectory.
Types of Palliative Care Service Models
| Service Model | Key Features | Nursing Role | Advantages |
|---|---|---|---|
| Hospital-Based Consultation |
|
|
|
| Palliative Care Units |
|
|
|
| Home-Based Palliative Care |
|
|
|
| Outpatient Palliative Clinics |
|
|
|
| Community Palliative Care Centers |
|
|
|
Core Nursing Competencies in Palliative Care
Symptom Assessment and Management
-
●
Pain Management:
Comprehensive pain assessment using validated tools, pharmacological and non-pharmacological interventions, breakthrough pain management
-
●
Respiratory Symptom Management:
Dyspnea assessment and interventions, secretion management, oxygen therapy, positioning strategies
-
●
Gastrointestinal Symptom Management:
Nausea/vomiting control, constipation prevention, mouth care, appetite stimulation
Psychosocial and Spiritual Support
-
●
Psychological Assessment:
Screening for depression, anxiety, adjustment disorders; implementing therapeutic communication techniques
-
●
Family Support:
Family conferences, caregiver assessment, anticipatory grief support, resource connection
-
●
Spiritual Care:
Spiritual assessment, recognition of cultural and religious practices, facilitation of meaningful rituals
Mnemonic: “COMFORT”
Use this mnemonic for palliative care communication with patients and families:
- C – Communication (clear, compassionate, consistent)
- O – Orientation to options and resources
- M – Mindful presence and active listening
- F – Family involvement and support
- O – Openness to cultural and spiritual needs
- R – Respect for patient goals and preferences
- T – Team collaboration and coordination
Hospice Care Centers
Hospice care centers are specialized community resources providing comprehensive end-of-life care for individuals with terminal illnesses and their families. Unlike palliative care, hospice focuses exclusively on comfort measures when curative treatment is no longer pursued, typically in the last six months of life.
Hospice Care Models
-
●
Home Hospice:
Services provided in the patient’s residence with family caregivers, supplemented by regular nursing visits, home health aide support, and 24/7 on-call assistance.
-
●
Inpatient Hospice Units:
Dedicated facilities or hospital wings providing 24-hour specialized end-of-life care for patients with complex symptom management needs or when home care is not feasible.
-
●
Residential Hospice:
Homelike facilities for patients who cannot remain at home but don’t require hospital-level care, offering round-the-clock support in a non-clinical environment.
-
●
Day Hospice:
Programs providing respite care, symptom management, and social support during daytime hours, allowing patients to return home in the evenings.
The Interdisciplinary Hospice Team
Hospice care is delivered through a comprehensive team approach:
Physicians
- Certification of terminal diagnosis
- Symptom management orders
- Medical direction
Nurses
- Symptom assessment and management
- Care coordination
- Family education and support
Social Workers
- Psychosocial assessment
- Resource connections
- Practical support services
Spiritual Counselors
- Spiritual support and rituals
- Existential concerns
- Cultural practice facilitation
Home Health Aides
- Personal care assistance
- Comfort measures
- Light housekeeping
Volunteers
- Companionship
- Respite care
- Practical assistance
Core Nursing Interventions in Hospice Care
| Domain | Assessment Focus | Key Interventions | Expected Outcomes |
|---|---|---|---|
| Physical Comfort |
|
|
|
| Psychosocial Support |
|
|
|
| Active Dying Care |
|
|
|
| Bereavement Support |
|
|
|
Signs and Symptoms of Approaching Death
Nurses must recognize and educate families about these common changes in the final days and hours:
Days to Weeks Before
- Increased sleep and fatigue
- Decreased appetite and intake
- Social withdrawal
- Reduced interest in surroundings
- Confusion or restlessness
Days to Hours Before
- Altered consciousness
- Difficulty swallowing
- Respiratory pattern changes
- Mottled skin appearance
- Decreased urine output
- Cool extremities
Final Hours
- Cheyne-Stokes breathing
- Inability to arouse
- “Death rattle” (respiratory secretions)
- Jaw relaxation
- Loss of vital signs
- Cessation of breathing and heartbeat
Mnemonic: “PEACE”
A framework for nursing priorities in end-of-life care:
- P – Physical comfort and symptom management
- E – Emotional and psychological support
- A – Autonomy and dignity preservation
- C – Communication with patient and family
- E – Education about the dying process
Assisted Living Facilities
Assisted living facilities (ALFs) are essential community resources providing housing, personalized support services, and healthcare for individuals who need assistance with daily activities but don’t require the intensive medical care of nursing homes. These facilities emphasize independence while offering necessary support.
Services Provided
- ● 24-hour supervision and security
- ● Meals and nutritional support
- ● Medication management
- ● Personal care assistance (bathing, dressing)
- ● Housekeeping and laundry
- ● Transportation services
- ● Social and recreational activities
- ● Basic health monitoring
Physical Environment
- ● Private or semi-private apartments/rooms
- ● Barrier-free design features
- ● Emergency call systems
- ● Common dining areas
- ● Social and recreational spaces
- ● Outdoor areas and gardens
- ● Safety features (handrails, grab bars)
- ● Wellness/fitness facilities
Specialized Programs
- ● Memory care units
- ● Respite care services
- ● Rehabilitation services
- ● Diabetes management programs
- ● Wellness and health promotion
- ● Transitional care programs
- ● Palliative care services
- ● Cultural/religious-specific programs
Community Health Nursing Role in Assisted Living
| Nursing Function | Responsibilities | Best Practices |
|---|---|---|
| Assessment & Monitoring |
|
|
| Medication Management |
|
|
| Health Promotion |
|
|
| Care Coordination |
|
|
| Staff Education |
|
|
Key Considerations for Assisted Living Placement
Client Assessment Factors
- Level of independence in activities of daily living
- Cognitive status and decision-making capacity
- Medical complexity and stability
- Medication management capabilities
- Safety risks (falls, wandering, etc.)
- Social needs and preferences
- Psychological and emotional status
Facility Evaluation Criteria
- Licensure status and regulatory compliance
- Staffing patterns and qualifications
- Available service levels and care options
- Physical environment and accessibility
- Activity and socialization opportunities
- Location relative to family and healthcare providers
- Cost structure and financial policies
Mnemonic: “ASSIST”
Use this mnemonic when assessing assisted living facility appropriateness:
- A – Activities of daily living support needs
- S – Safety requirements and environmental adaptations
- S – Services offered match client needs
- I – Independence level that can be maintained
- S – Social engagement opportunities
- T – Transition readiness (client and family)
Nursing Role in Community Resource Coordination
Community health nurses serve as critical connectors between clients and the diverse community resources available to meet their needs. Effective resource coordination requires comprehensive assessment, navigation skills, and an understanding of the interconnected nature of health and social services.
Core Competencies for Resource Coordination
-
●
Resource Knowledge:
Maintaining comprehensive understanding of available community resources, their eligibility criteria, referral processes, and service limitations.
-
●
Needs Assessment:
Conducting thorough biopsychosocial assessments to identify the complex, interconnected needs of clients and families.
-
●
Navigation Skills:
Guiding clients through complex service systems, helping overcome barriers to access, and facilitating smooth transitions between services.
-
●
Advocacy:
Advocating for client needs within service systems, addressing gaps in care, and securing necessary services when barriers arise.
-
●
Coordination:
Orchestrating multiple services and providers to create cohesive care plans that address interrelated client needs.
Resource Coordination Process
-
1
Comprehensive Assessment
Conduct holistic needs assessment considering health, functional, psychological, social, financial, and environmental factors.
-
2
Resource Identification
Match client needs with appropriate community resources, considering accessibility, affordability, and cultural appropriateness.
-
3
Referral and Connection
Facilitate warm handoffs to services, provide necessary documentation, and prepare clients for what to expect.
-
4
Barrier Identification and Mitigation
Anticipate and address potential barriers to service utilization, including transportation, financial, or communication challenges.
-
5
Follow-up and Monitoring
Track referral outcomes, assess effectiveness of services, and adjust plans as client needs evolve.
Resource Coordination Tools and Strategies
Community Resource Mapping
Creating comprehensive inventories of local resources, including service details, eligibility criteria, and contact information. Updated regularly and shared across healthcare teams.
Electronic Referral Systems
Utilizing integrated technology platforms that streamline referral processes, track outcomes, and facilitate communication between healthcare providers and community organizations.
Care Coordination Teams
Forming multidisciplinary teams including nurses, social workers, and community health workers to provide comprehensive coordination across medical and social service sectors.
Standardized Assessment Tools
Implementing validated tools to comprehensively assess social determinants of health and resource needs, ensuring consistent identification of service gaps.
Community Partnerships
Developing formal relationships with community organizations to streamline referral processes, share information, and collaboratively address service gaps.
Follow-up Protocols
Establishing structured follow-up processes to ensure clients successfully connect with referred services and to evaluate the effectiveness of resource coordination.
Overcoming Barriers to Resource Utilization
| Barrier Category | Common Barriers | Nursing Interventions |
|---|---|---|
| Access Barriers |
|
|
| Financial Barriers |
|
|
| Informational Barriers |
|
|
| Personal/Cultural Barriers |
|
|
| System Barriers |
|
|
Mnemonic: “BRIDGE”
Use this mnemonic for effective community resource coordination:
- B – Build comprehensive assessment of client needs
- R – Research appropriate community resources
- I – Identify and address potential barriers
- D – Develop referral relationships with providers
- G – Guide clients through service connections
- E – Evaluate outcomes and adjust as needed
Global Best Practices in Community Resource Utilization
Innovative approaches to community resource coordination and utilization have emerged globally, offering valuable models that can be adapted across different healthcare systems. These exemplary practices demonstrate effective integration of services to address complex client needs.
Netherlands: Integrated Neighborhood Care
The Buurtzorg model from the Netherlands has revolutionized community care through self-managed nursing teams providing comprehensive services within defined neighborhoods.
- ● Small, autonomous nursing teams (8-12 nurses) responsible for 50-60 clients in a neighborhood
- ● Holistic approach integrating medical care with social support and community connection
- ● Development of informal neighborhood support networks as adjuncts to formal services
- ● Sophisticated IT support for efficient documentation and resource coordination
Key outcome: Demonstrated reductions in hospitalization rates, increased client satisfaction, and cost-effectiveness compared to traditional care models.
Australia: Integrated HealthPathways
Australia’s HealthPathways system creates standardized, locally relevant pathways connecting primary care providers with community and specialist resources.
- ● Web-based portal providing condition-specific pathways and resource information
- ● Locally adapted content developed collaboratively by primary care and specialists
- ● Integration of medical, social, and community resources in single platform
- ● Regular updates reflecting service changes and emerging evidence
Key outcome: Reduced referral rejection rates, improved appropriateness of resource utilization, and enhanced care coordination across sectors.
Canada: CAPC/CPNP Programs
Canada’s Community Action Program for Children (CAPC) and Canada Prenatal Nutrition Program (CPNP) demonstrate effective community-based resource networking for vulnerable populations.
- ● Community-driven programs tailored to local needs and resources
- ● Co-location of multiple services (nutrition, parenting, healthcare) at accessible community sites
- ● Peer support components integrated with professional services
- ● Cultural adaptation of programs for Indigenous and immigrant communities
Key outcome: Improved maternal-child health indicators, enhanced parenting confidence, and increased service utilization by traditionally underserved populations.
Japan: Community-Based Integrated Care System
Japan’s response to an aging population has produced innovative community-based care systems integrating healthcare, long-term care, housing, and social services.
- ● Geographic organization of comprehensive services within 30-minute radius communities
- ● Community care coordination centers managing transitions across settings
- ● Integration of volunteer networks with formal services
- ● Prevention-focused programming to maintain independence
Key outcome: Enhanced aging in place, reduced institutionalization rates, and community revitalization through intergenerational initiatives.
