Neonatal Care Essentials: Vitamin K Prophylaxis & Newborn Resuscitation
Comprehensive evidence-based notes for nursing students
Table of Contents
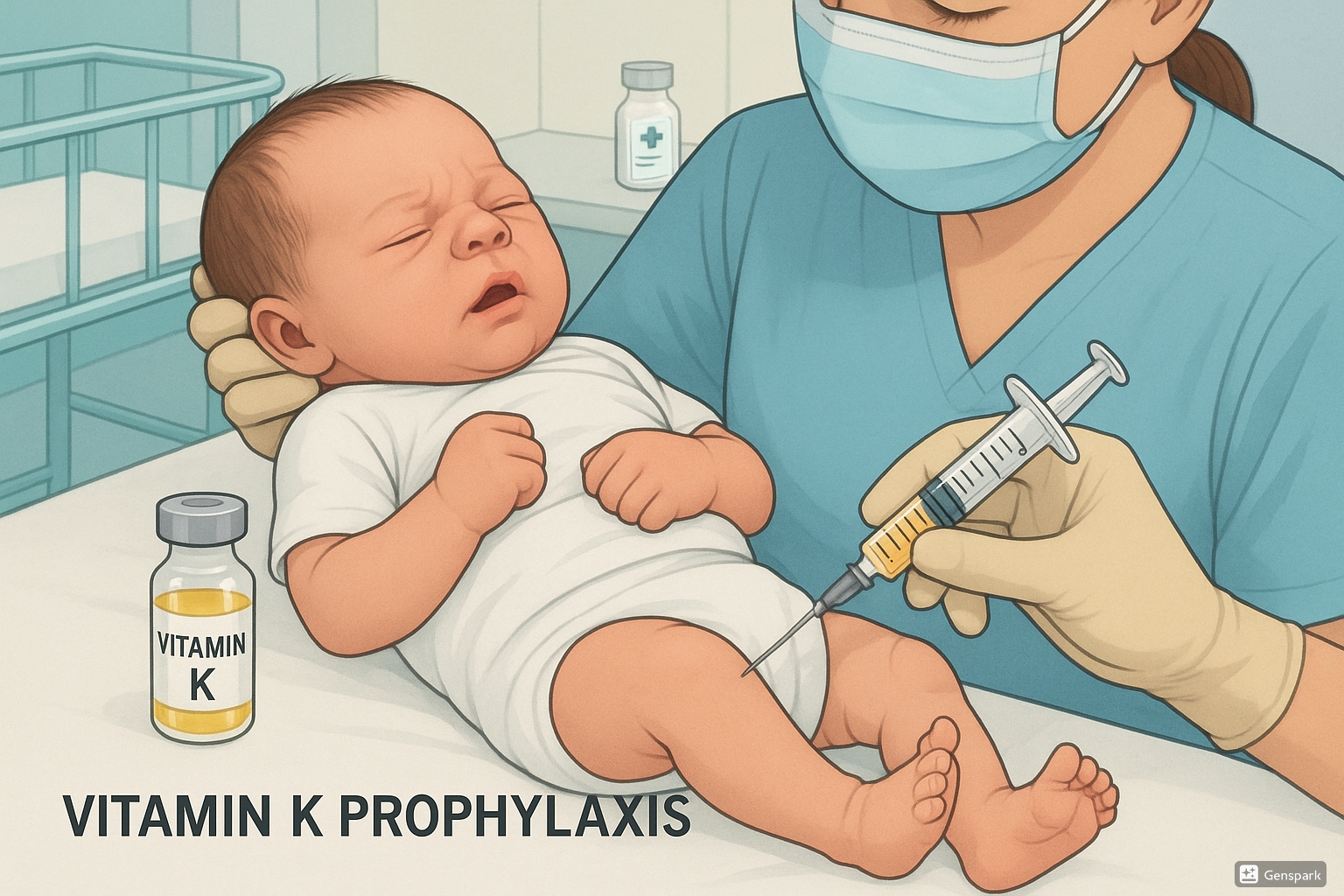
Vitamin K Prophylaxis
Vitamin K prophylaxis is a crucial preventive intervention administered to newborns shortly after birth to prevent potentially life-threatening bleeding disorders.
What is Vitamin K?
Vitamin K is a fat-soluble vitamin essential for blood clotting. It’s named after the German word for clotting, koagulation (spelled with a K). There are different types of Vitamin K:
- Vitamin K1 (phylloquinone) – Found in leafy green vegetables (makes up about 90% of overall Vitamin K levels)
- Vitamin K2 (menaquinones) – Produced by bacteria in the intestinal tract (makes up about 10% of overall Vitamin K levels)
Vitamin K activates clotting factors in the coagulation cascade, enabling the blood to form clots and prevent excessive bleeding.
Why Newborns Need Vitamin K
Newborns are born with very low levels of Vitamin K for several reasons:
- Limited placental transfer – Vitamin K does not cross the placenta efficiently
- Sterile gut – Newborns lack the intestinal bacteria needed to produce Vitamin K2
- Immature liver – The newborn liver cannot efficiently utilize the small amounts of Vitamin K available
Human milk contains very limited amounts of Vitamin K (1-9 μg/L), while formula has higher levels (around 55 μg/L). Thus, exclusively breastfed infants are at higher risk of Vitamin K deficiency bleeding if they do not receive supplementation.
Vitamin K Deficiency Bleeding (VKDB)
Vitamin K Deficiency Bleeding (VKDB), formerly known as Hemorrhagic Disease of the Newborn (HDN), is a rare but serious condition where a newborn develops spontaneous bleeding due to low levels of Vitamin K.
| Classification | Timing | Common Bleeding Sites | Risk Factors |
|---|---|---|---|
| Early VKDB | First 24 hours of life | Skin, brain, abdomen | Maternal medications that interfere with Vitamin K (Warfarin, seizure medications, tuberculosis medications) |
| Classic VKDB | Days 2-7 of life (typically days 2-3) | Gastrointestinal tract, umbilical cord site, skin, nose, circumcision site | Breastfeeding or insufficient milk intake |
| Late VKDB | Week 1 to month 6 (peak: weeks 3-8) | Brain, skin, gastrointestinal tract | Exclusive breastfeeding without Vitamin K supplementation, undetected liver/gallbladder disease, chronic diarrhea, antibiotic use |
Warning Signs of VKDB
VKDB often occurs with no early symptoms, making prevention critical. Signs to monitor include:
- Difficulty feeding, lethargy, fussiness
- Bulging soft spots on baby’s head
- Unexplained bruising or pooling of blood under the skin
- Bleeding from nose, skin, circumcision site, gums, or umbilical cord
- Pale appearance
- Yellow eyes after three weeks of age
- Blood in diaper or stool, black tarry stool after day 3
- Vomiting blood
Current Guidelines
All major health organizations worldwide recommend routine Vitamin K prophylaxis for newborns:
| Organization | Recommendations |
|---|---|
| World Health Organization (WHO) | All newborns should receive 1 mg of Vitamin K IM after birth (after the first hour of skin-to-skin contact and initiation of breastfeeding). (Strong recommendation, moderate quality evidence) |
| American Academy of Pediatrics (AAP) | Vitamin K1 should be given to all newborns as a single, intramuscular dose of 0.5 to 1 mg. |
| Centers for Disease Control and Prevention (CDC) | One shot intramuscularly in the thigh within 6 hours of birth. |
| National Institute for Health and Care Excellence (NICE) | Vitamin K should be administered as a single dose of 1 mg intramuscularly as the most clinically and cost-effective method. |
| European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) | Three options:
1) 1 mg Vitamin K1 by IM injection at birth, OR 2) 3 × 2 mg Vitamin K1 orally at birth, at 4-6 days, and at 4-6 weeks, OR 3) 2 mg Vitamin K1 orally at birth and weekly 1 mg for 3 months |
Administration Methods
Intramuscular (IM) Administration
Pros:
- Highly effective at preventing both classic and late VKDB
- Single dose (better compliance)
- Slow release effect provides protection for months
- Regulated, standardized dose
Cons:
- Pain at injection site (can be minimized with holding or nursing during administration)
- Potential for bleeding, redness, irritation, or bruising at injection site
- May not be 100% effective in cases of undetected gallbladder or liver disease
Oral Administration
Pros:
- Non-invasive, pain-free method
- Multiple dosing regimens available
- Weekly dosing may protect infants with undiagnosed gallbladder problems
Cons:
- Requires multiple doses (compliance issues)
- Variable absorption, especially if given on empty stomach
- Less effective in preventing late VKDB than injection
- Risk of spitting up doses
- In US, no FDA-approved oral preparation (unregulated supplements)
- Less effective in infants with undetected gallbladder disease
Memory Aid: “The VKDB Shield”
V – Verify dosage (1 mg IM for term infants)
K – Know administration technique (anterolateral thigh)
D – Document thoroughly (time, site, lot number)
B – Breastfed babies need it most (higher risk)
S – Single IM dose vs multiple oral doses (IM preferred)
H – High-risk groups need special attention (preterm, maternal medications)
I – Inform parents about benefits (prevention of bleeding)
E – Education about warning signs (if prophylaxis refused)
L – Late VKDB potentially most dangerous (brain bleeds)
D – Delay injection until after first breastfeeding/bonding
Special Populations
Preterm Infants
Preterm infants are at higher risk for VKDB due to:
- More immature liver and circulatory systems
- Even lower baseline Vitamin K levels than term infants
- Delayed feeding initiation
- Potential exposure to antibiotics
| Weight Category | Recommended Dose |
|---|---|
| ≥1500g (>3.3 pounds) | 1 mg IM |
| <1500g (≤3.3 pounds) | 0.5 mg IM |
| <1000g (≤2.2 pounds) | 0.3 mg IM or IV |
| <32 weeks and >1000g | 0.5 mg IM or IV |
Note: Intravenous administration is not recommended for prophylaxis due to shorter half-life than IM administration.
High-Risk Infants
Certain infants require special attention regarding Vitamin K prophylaxis:
- Infants requiring surgical procedures
- Infants with birth trauma
- Exclusively breastfed infants
- Infants exposed to maternal medications that interfere with Vitamin K metabolism:
- Anticoagulants (Warfarin)
- Anticonvulsants (phenytoin, phenobarbital, carbamazepine)
- Antibiotics (certain cephalosporins)
- Tuberculosis medications (rifampin, isoniazid)
- Infants with undiagnosed liver or gallbladder disease
Addressing Parental Refusal
Parental refusal of Vitamin K prophylaxis is increasing, leading to an increase in cases of late VKDB. Common reasons for refusal include:
- Belief that risks of the shot outweigh benefits
- Perception that oral administration is more natural
- Mistrust of medical providers or pharmaceutical industry
- Reliance on social media for health information
- Concerns about vaccine ingredients extending to any injections
- Belief that a gentle birth eliminates the need for Vitamin K
- Misconceptions about cancer risks (thoroughly disproven)
Evidence-Based Counseling Points
- VKDB is rare but potentially devastating, with mortality rates around 20%
- Of infants who survive late VKDB, approximately 40% have long-term brain damage
- The alleged link between Vitamin K and childhood cancer has been conclusively disproven by multiple large studies
- The risk of severe allergic reaction is extremely rare (only one published case report with current formulation)
- Pain can be minimized by administering the injection during skin-to-skin contact or breastfeeding
- A “gentle” or uncomplicated birth does not prevent VKDB, as it’s related to natural Vitamin K deficiency, not birth trauma
Nurse’s Role in Addressing Refusal
- Assess and address specific parental concerns
- Provide evidence-based information at the parents’ level of understanding
- Acknowledge parental autonomy while emphasizing the medical recommendation
- If parents still refuse IM Vitamin K, discuss oral alternatives
- Document the discussion and parental decision
- Provide education on warning signs of VKDB if prophylaxis is declined
Best Practices & Updates
Recent Updates in Vitamin K Prophylaxis
1. Weekly Oral Dosing Shows Promise
Recent studies from Japan and Italy (2024) found that weekly oral dosing regimens of Vitamin K may be more effective than the traditional three-dose regimens, especially for exclusively breastfed infants.
2. Timing of Administration
Current recommendations support delaying Vitamin K administration until after the first hour of life to allow for uninterrupted skin-to-skin contact and initiation of breastfeeding, while still administering within the first 6 hours of life.
3. Pain Reduction Strategies
Evidence supports administering Vitamin K during breastfeeding or skin-to-skin contact to reduce pain. Simple analgesic interventions like sucrose solution or breast milk can also reduce procedural pain during IM administration.
Newborn Resuscitation
Newborn resuscitation involves a systematic approach to supporting babies who require assistance transitioning to extrauterine life. The Neonatal Resuscitation Program (NRP) provides evidence-based guidelines for this critical care.
NRP Overview & Principles
The Neonatal Resuscitation Program (NRP) is an evidence-based approach to care of the newborn at birth that facilitates effective team-based care. The majority of newborns transition successfully to extrauterine life with minimal or no assistance, but approximately 10% require some intervention to establish breathing, and 1% need extensive resuscitative measures.
Key Principles:
- Most newborns requiring intervention need only respiratory support
- Effective ventilation is the cornerstone of successful newborn resuscitation
- Resuscitation should follow a systematic approach based on assessment
- Team communication and role clarity are essential
- Prevention of heat loss is crucial for successful outcomes
Memory Aid: “A-B-C-D of Neonatal Resuscitation”
A – Airway (open the airway)
B – Breathing (establish effective ventilation)
C – Circulation (chest compressions if needed)
D – Drugs (medication administration if indicated)
Initial Assessment
Initial assessment determines the need for resuscitation and begins with three key questions:
- Is the baby term?
- Is the baby breathing or crying?
- Does the baby have good muscle tone?
If the answer to all three questions is “yes,” the baby can usually remain with the mother for routine care:
- Provide warmth
- Clear airway if needed
- Dry the infant
- Ensure ongoing evaluation
If any answer is “no,” the infant should receive one or more of the following:
- Warmth and positioning
- Clearing of airway as needed
- Drying, stimulation
- Assessment of breathing, heart rate, and color
The Apgar Score
While not used to determine need for resuscitation, the Apgar score provides a standardized assessment at 1 and 5 minutes after birth:
| Sign | 0 points | 1 point | 2 points |
|---|---|---|---|
| Appearance (Color) | Blue or pale | Body pink, extremities blue | Completely pink |
| Pulse (Heart rate) | Absent | <100 bpm | ≥100 bpm |
| Grimace (Reflex irritability) | No response | Grimace/weak cry when stimulated | Cry or active withdrawal |
| Activity (Muscle tone) | Limp | Some flexion | Well-flexed |
| Respiration | Absent | Slow, irregular | Good, crying |
Resuscitation Algorithm
The following algorithm outlines the sequential steps of newborn resuscitation according to the latest guidelines:
Birth
Term gestation? Breathing or crying? Good tone?
If YES → Routine care: Provide warmth, clear airway if needed, dry, ongoing evaluation
If NO → Continue to next step
Initial Steps (First 30 seconds)
- Provide warmth
- Position head in “sniffing” position
- Clear airway if necessary (only suction mouth then nose if obvious obstruction)
- Dry, stimulate, reposition
- Evaluate respirations, heart rate, and activity
Assessment (30-60 seconds)
Apneic, gasping, or HR <100/min?
If YES → Initiate PPV with 21% oxygen (room air), consider SpO₂ monitoring
If NO but labored breathing or persistent cyanosis → CPAP, consider SpO₂ monitoring
Ventilation Phase (30-60 seconds of PPV)
- Ensure effective ventilation (chest movement)
- Consider:
- Repositioning head
- Suctioning airway
- Ventilating with open mouth
- Increasing pressure
- Alternative airway (supraglottic or endotracheal tube)
- Check HR
HR <60/min? → Begin chest compressions
Circulation Phase (Compressions + PPV)
- 3:1 ratio of compressions to ventilations
- 90 compressions and 30 breaths per minute
- Consider increasing oxygen to 100%
- Check HR after 60 seconds
HR <60/min despite effective ventilation and compressions? → Consider medications
Medication Phase
- Epinephrine: 0.01-0.03 mg/kg of 1:10,000 solution (IV preferred)
- Consider volume expansion (10 mL/kg normal saline)
- Continue PPV and chest compressions
- Reassess and repeat epinephrine every 3-5 minutes if HR remains <60/min
Critical Decision Points
- HR <100/min → Start PPV
- HR <60/min despite 30 seconds of effective ventilation → Start chest compressions
- HR <60/min despite 60 seconds of compressions and ventilation → Consider medications
Memory Aid: “The Golden Minutes”
60 seconds – Complete initial steps and assessment
90 seconds – Establish effective ventilation
2 minutes – Begin chest compressions if needed
3 minutes – Consider epinephrine if no response
Ventilation Techniques
Effective ventilation is the single most important and effective intervention in neonatal resuscitation. The 2023 AHA/AAP guidelines provide updated recommendations on devices and interfaces for delivering positive-pressure ventilation (PPV).
Ventilation Devices
| Device | Advantages | Disadvantages | Recommendations |
|---|---|---|---|
| T-piece Resuscitator |
|
|
Preferred device for delivering PPV |
| Self-inflating Bag |
|
|
Backup device when T-piece or flow-inflating bag unavailable or gas source fails |
| Flow-inflating Bag |
|
|
Acceptable alternative to T-piece resuscitator |
Ventilation Interfaces
| Interface | Advantages | Disadvantages | Recommendations |
|---|---|---|---|
| Face Mask |
|
|
Standard interface for initial PPV |
| Supraglottic Airway |
|
|
May be considered as primary interface instead of face mask for newborns ≥34 weeks’ gestation |
| Endotracheal Tube |
|
|
Reserved for ineffective bag-mask ventilation, prolonged ventilation needs, or special circumstances |
Ventilation Parameters
- Initial pressure: 20-25 cm H₂O for term infants (adjust based on chest rise)
- PEEP: 5 cm H₂O when available
- Rate: 40-60 breaths per minute (consider using phrases like “Breathe, two, three”)
- Initial oxygen: 21% (room air) for term infants; 21-30% for preterm infants
- Inspiratory time: 0.5-1 second
2023 Update on Ventilation
The 2023 AHA/AAP focused update recommends:
- Using a T-piece resuscitator to deliver PPV is preferred to the use of a self-inflating bag
- A self-inflating bag should be available as a backup in the event of compressed gas failure
- Use of a supraglottic airway may be considered as a primary interface instead of a face mask for newborns ≥34 weeks’ gestation
Chest Compressions
Chest compressions are indicated when the heart rate remains below 60 beats per minute despite 30 seconds of effective positive-pressure ventilation.
Compression Technique
- Two-thumb technique (preferred): Two thumbs compress the sternum with fingers encircling the chest and supporting the back
- Two-finger technique: Two fingers compress the sternum while the other hand supports the back (used when umbilical access needed)
- Location: Lower third of sternum, just below an imaginary line connecting the nipples
- Depth: Approximately one-third the anterior-posterior diameter of the chest
Compression-to-Ventilation Coordination
- Ratio: 3 compressions to 1 ventilation (3:1)
- Rate: 90 compressions and 30 breaths per minute (120 events per minute)
- Coordination: Compressions and ventilations should be delivered in a coordinated sequence, not simultaneously
- Count: “One-and-two-and-three-and-breathe” rhythm
Assessment During Compressions
- Check heart rate after 60 seconds of chest compressions and ventilation
- Continue compressions until heart rate is ≥60 beats per minute
- Reassign roles periodically to prevent compressor fatigue
Memory Aid: “The 3C’s of Chest Compressions”
Correct positioning (lower third of sternum)
Compression depth (one-third AP diameter)
Coordinated ratio (3:1 with ventilations)
Medications in Resuscitation
Medications are rarely needed in newborn resuscitation and should only be considered when the heart rate remains below 60 beats per minute despite adequate ventilation with 100% oxygen and chest compressions.
| Medication | Indication | Dose & Route | Preparation | Notes |
|---|---|---|---|---|
| Epinephrine | HR <60/min despite ventilation and chest compressions | 0.01-0.03 mg/kg (0.1-0.3 mL/kg of 1:10,000 solution) IV/IO preferred ETT: 0.05-0.1 mg/kg |
1:10,000 solution (0.1 mg/mL) | May repeat every 3-5 minutes Flush with normal saline after administration |
| Volume Expanders | Suspected blood loss or signs of shock/hypovolemia | 10 mL/kg IV/IO route |
Normal saline or O-negative blood for acute blood loss | Administer over 5-10 minutes May repeat based on response |
| Dextrose | Documented hypoglycemia | 2 mL/kg of D10W (0.2 g/kg) IV/IO route |
D10W solution | Not a routine resuscitation medication Used after resuscitation for confirmed hypoglycemia |
| Sodium Bicarbonate | Prolonged arrest with documented metabolic acidosis | 1-2 mEq/kg (2-4 mL/kg of 0.5 mEq/mL solution) IV/IO route |
0.5 mEq/mL solution (4.2%) | Not recommended during brief resuscitation Administer slowly (not faster than 1 mEq/kg/min) |
| Naloxone | No longer recommended as part of initial resuscitation even with maternal opioid use | 0.1 mg/kg IV/IO/IM/SQ (if used post-resuscitation) |
0.4 mg/mL or 1 mg/mL | Focus on effective ventilation rather than reversing respiratory depression with naloxone |
Administration Routes
- Umbilical venous catheter (UVC) – Preferred route during resuscitation
- Intraosseous (IO) – Alternative when IV access cannot be established
- Endotracheal tube (ETT) – Limited to epinephrine when no IV access; higher doses required
- Peripheral IV – May be used but more difficult to establish during resuscitation
Important Considerations
- Ventilation remains the most important intervention
- Most newborns respond to effective ventilation alone
- Medications should only be considered after effective ventilation and compressions fail to improve heart rate
- When administering medications via ETT, use higher doses and follow with positive pressure breaths to distribute medication
Special Considerations
Preterm Infants
Preterm infants require special considerations during resuscitation:
- Temperature management: Increased risk of hypothermia; use plastic wrap/bag for infants <32 weeks
- Oxygen therapy: Start with lower oxygen concentrations (21-30%) and titrate based on pre-ductal SpO₂
- Gentle ventilation: More susceptible to lung injury; avoid excessive pressures
- Delayed cord clamping: Per 2023 guidelines, preterm infants <34 weeks who do not require resuscitation benefit from delayed cord clamping (≥30 seconds)
- Umbilical cord management: Intact cord milking is not recommended for infants <28 weeks’ gestation
Meconium Presence
Current recommendations regarding meconium-stained amniotic fluid:
- Routine intubation for tracheal suction is not recommended
- Initial steps of resuscitation remain the same regardless of meconium consistency
- Emphasis on establishing ventilation quickly in non-vigorous infants
- If PPV required, visualize vocal cords and suction only if obstruction is seen
Congenital Anomalies
Certain congenital anomalies may require modified resuscitation approaches:
- Diaphragmatic hernia: Immediate intubation, no bag-mask ventilation, gastric decompression
- Choanal atresia: Oral airway placement or intubation
- Airway obstructive lesions: Consider EXIT (Ex Utero Intrapartum Treatment) procedure
- Abdominal wall defects: Cover with sterile, warm, moist dressing and position to avoid kinking of vessels
Discontinuing Resuscitation
If a newborn has no detectable heart rate after 10 minutes of complete and adequate resuscitation efforts, it may be reasonable to stop resuscitation. However, the decision to continue or discontinue should consider:
- Gestational age of the infant
- Presumed etiology of the arrest
- Presence of complications
- Potential role of therapeutic hypothermia
- Family’s previously expressed feelings about acceptable risk and disability
Best Practices & Updates
Recent Updates in Newborn Resuscitation (2023)
1. Umbilical Cord Management
- For term and late preterm newborn infants ≥34 weeks’ gestation who do not require resuscitation, delayed cord clamping (≥30 seconds) is beneficial compared with early cord clamping (<30 seconds)
- For nonvigorous term and late preterm newborn infants (35–42 weeks’ gestation), intact cord milking may be reasonable compared with early cord clamping
- For preterm newborn infants <28 weeks’ gestation, intact cord milking is not recommended
2. Ventilation Devices and Interfaces
- Using a T-piece resuscitator to deliver PPV is preferred to using a self-inflating bag
- A self-inflating bag should be available as backup when using T-piece or flow-inflating bags
- Supraglottic airways may be used as primary interface instead of face mask for newborns ≥34 weeks’ gestation
3. Team Communication and Debriefing
- Emphasis on clear role assignments before delivery
- Use of closed-loop communication during resuscitation
- Post-resuscitation debriefings to improve future performance
- Regular team simulation training for rare but critical scenarios
References
- American Academy of Pediatrics, Committee on Fetus and Newborn. Vitamin K and the Newborn Infant. Pediatrics. 2022;149(3):e2021056036.
- World Health Organization. WHO recommendations on newborn health. Guidelines approved by the WHO guidelines review committee. Geneva. 2017.
- Gomersall J, et al. Umbilical cord management at term and late preterm birth: a meta-analysis. Pediatrics. 2021;147:e2020015404.
- Wyckoff MH, et al. 2023 focused update on neonatal resuscitation guidelines. Circulation. 2023;147(13):e1081-e1096.
- Evidence Based Birth. Evidence on: The Vitamin K Shot in Newborns. Updated February 2025.
- Seidler AL, et al. Umbilical cord management for newborns <34 weeks' gestation: a meta-analysis. Pediatrics. 2021;147:e20200576.
- National Institute for Health and Care Excellence (NICE). Postnatal care up to 8 weeks after birth. 2015.
- Trevisanuto D, et al. Devices for administering ventilation at birth: a systematic review. Pediatrics. 2021;148:e2021050174.
- Yamada NK, et al. Supraglottic airways compared with face masks for neonatal resuscitation: a systematic review. Pediatrics. 2022;150:e2022056568.
- Sankar MJ, et al. Vitamin K prophylaxis for prevention of vitamin K deficiency bleeding: a systematic review. J Perinatol. 2016;36(S1):S29-S35.
- Centers for Disease Control and Prevention. Vitamin K Deficiency Bleeding. Updated 2018.
- Katheria AC, et al. Umbilical cord milking in nonvigorous infants: a cluster-randomized crossover trial. Am J Obstet Gynecol. 2023;228:217.e1-217.e14.
