Community Health Nursing: Essential Assessments and Procedures
A Comprehensive Guide for Nursing Students
Table of Contents
Introduction to Community Health Assessment
Community health assessment is a cornerstone of public health nursing practice, providing essential data for developing health promotion and disease prevention strategies. These assessments help identify health risks, monitor community health status, and evaluate the effectiveness of health interventions.
Community health nurses employ various assessment techniques to gather comprehensive health data from individuals and populations. These include anthropometric measurements, vital signs monitoring, screening for common health conditions, and educating community members about self-examination procedures.
This comprehensive guide focuses on essential community health assessment procedures that nursing students should master. Each assessment is presented with step-by-step instructions, normal values, interpretation guidelines, and nursing considerations to ensure accurate and effective community health assessments.
Anthropometric Measurements
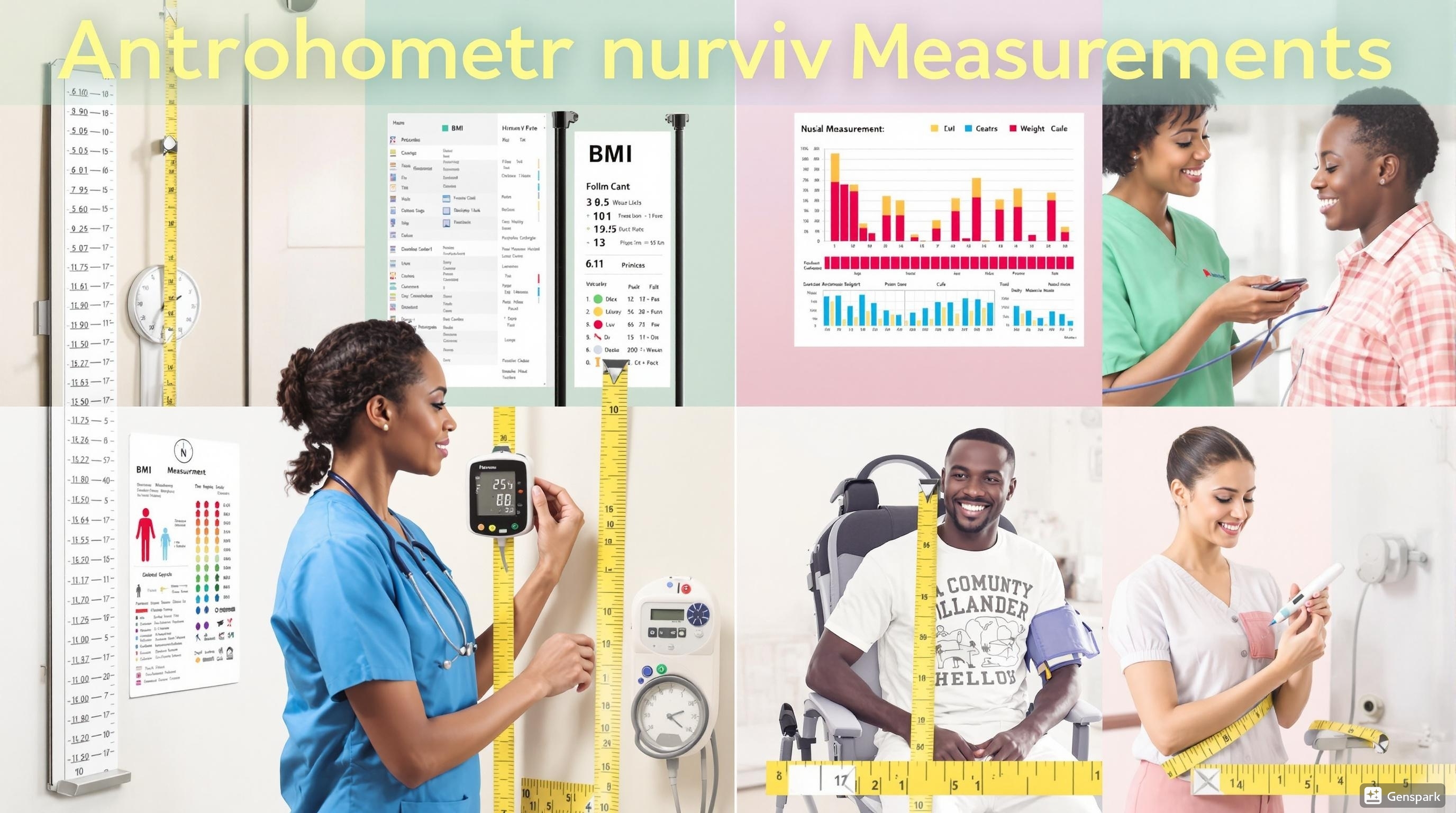
Comprehensive anthropometric measurements being performed by a community health nurse
Anthropometric measurements are quantitative assessments of body dimensions that provide valuable information about growth, development, and nutritional status. In community health nursing, these measurements are essential for health screening, nutritional assessment, and monitoring growth patterns, especially in children.
Key Anthropometric Measurements
| Measurement | Equipment | Procedure | Nursing Considerations |
|---|---|---|---|
| Height | Stadiometer or measuring tape | Patient stands with back against wall, heels together, looking straight ahead | Remove shoes; ensure straight posture; read at eye level |
| Weight | Calibrated weighing scale | Patient stands on scale with minimal clothing | Zero the scale before use; weigh at the same time of day |
| Head Circumference | Non-stretchable tape measure | Measure the widest part of the head (occipitofrontal circumference) | Important for infants up to 36 months; plot on growth chart |
| Mid-Upper Arm Circumference (MUAC) | MUAC tape | Measure midpoint between acromion process and olecranon process | Quick screening tool for malnutrition; use non-dominant arm |
| Waist Circumference | Non-stretchable tape measure | Measure at midpoint between lowest rib and iliac crest | Indicator for abdominal obesity and metabolic risk |
Height Measurement Procedure
Step 1: Explain the procedure to the patient.
Step 2: Ask the patient to remove shoes and any head ornaments.
Step 3: Position the patient with heels, buttocks, and shoulder blades against the stadiometer or wall.
Step 4: Ensure the patient’s head is in the Frankfurt plane (imaginary line from the lower margin of the eye orbit to the auditory meatus is horizontal).
Step 5: Ask the patient to take a deep breath and stand tall.
Step 6: Lower the headpiece to rest firmly on the crown of the head.
Step 7: Read the measurement at eye level to the nearest 0.1 cm or 1/8 inch.
Step 8: Record the measurement and interpret using standard growth charts.
Weight Measurement Procedure
Step 1: Calibrate the scale to zero before use.
Step 2: Ask the patient to remove heavy clothing, shoes, and empty pockets.
Step 3: Ask the patient to stand still in the center of the scale platform.
Step 4: Wait for the digital display to stabilize or balance the scale weights.
Step 5: Record the weight to the nearest 0.1 kg or 0.2 lb.
Step 6: Interpret findings based on age, gender, and previous measurements.
Interpretation of Anthropometric Data
Anthropometric measurements are most valuable when:
- Compared to standardized references (WHO growth charts, CDC growth charts)
- Tracked over time to monitor growth patterns or weight changes
- Used in combination with other health assessment data
- Interpreted in the context of the individual’s health history
Mnemonic: “MEASURE” for Quality Anthropometric Assessment
M – Maintain calibrated equipment
E – Explain procedure to the patient
A – Accurate positioning of the patient
S – Standardized technique for each measurement
U – Use appropriate reference standards
R – Record measurements precisely
E – Evaluate trends over time
Body Mass Index (BMI)
Body Mass Index (BMI) is a screening tool that uses height and weight measurements to estimate body fat and assess health risks associated with weight status. While BMI has limitations (it doesn’t directly measure body fat or account for muscle mass), it remains a valuable screening tool in community health settings due to its simplicity and cost-effectiveness.
BMI Calculation
Metric Formula:
BMI = Weight (kg) / Height² (m²)
Imperial Formula:
BMI = [Weight (lbs) / Height² (inches²)] × 703
BMI Categories for Adults
| BMI Range | Weight Status | Health Risk |
|---|---|---|
| Below 18.5 | Underweight | Increased risk for nutritional deficiencies, osteoporosis |
| 18.5 – 24.9 | Normal or Healthy Weight | Lowest risk for weight-related health problems |
| 25.0 – 29.9 | Overweight | Increased risk for heart disease, diabetes, hypertension |
| 30.0 – 34.9 | Obesity Class I | High risk for weight-related health problems |
| 35.0 – 39.9 | Obesity Class II | Very high risk for weight-related health problems |
| 40.0 and above | Obesity Class III (Severe) | Extremely high risk for weight-related health problems |
BMI Calculation Procedure
Step 1: Measure height and weight using standardized techniques.
Step 2: Convert measurements if needed (pounds to kilograms, inches to meters).
Step 3: Calculate BMI using the appropriate formula.
Step 4: Interpret the BMI value using standard categories.
Step 5: Document the BMI value and category in the patient’s record.
Step 6: Provide appropriate education based on the BMI category.
Sample BMI Calculation
Example 1 (Metric):
Weight: 70 kg, Height: 1.75 m
BMI = 70 ÷ (1.75)² = 70 ÷ 3.0625 = 22.9 kg/m²
Interpretation: Normal weight
Example 2 (Imperial):
Weight: 160 lbs, Height: 65 inches
BMI = (160 ÷ 65²) × 703 = (160 ÷ 4225) × 703 = 0.0379 × 703 = 26.6 kg/m²
Interpretation: Overweight
Nursing Considerations for BMI Assessment
- BMI is less accurate for athletes, older adults, and pregnant women
- Use BMI in conjunction with waist circumference for better risk assessment
- Approach BMI discussions with sensitivity to avoid stigmatization
- For children and adolescents, use age- and gender-specific BMI percentiles
- Consider cultural factors and health beliefs when discussing weight
Mnemonic: “WEIGH-T” for BMI Communication
W – Words matter (use neutral, non-stigmatizing language)
E – Educate on BMI as one health indicator among many
I – Individual factors affect interpretation
G – Goals should be realistic and patient-centered
H – Health behaviors matter more than numbers
T – Trends over time are more informative than single readings
Temperature Monitoring
Body temperature monitoring is a fundamental vital sign assessment that provides valuable information about a person’s physiological status. In community health nursing, temperature monitoring helps detect infection, assess fever patterns, monitor treatment effectiveness, and screen for various health conditions.
Normal Temperature Ranges
| Measurement Site | Normal Range (°F) | Normal Range (°C) |
|---|---|---|
| Oral | 97.6 – 99.6°F | 36.5 – 37.5°C |
| Axillary | 96.4 – 97.3°F | 34.8 – 36.3°C |
| Tympanic | 97.0 – 100.2°F | 36.1 – 37.9°C |
| Rectal | 98.6 – 100.4°F | 37.0 – 38.0°C |
| Temporal | 97.5 – 99.5°F | 36.4 – 37.4°C |
Temperature Classification
| Classification | Temperature Range (°F) | Temperature Range (°C) |
|---|---|---|
| Hypothermia (Severe) | Below 89.6°F | Below 32.0°C |
| Hypothermia (Moderate) | 89.6 – 95.0°F | 32.0 – 35.0°C |
| Hypothermia (Mild) | 95.0 – 96.8°F | 35.0 – 36.0°C |
| Normal | 96.8 – 99.5°F | 36.0 – 37.5°C |
| Fever (Low-grade) | 99.5 – 100.9°F | 37.5 – 38.3°C |
| Fever (Moderate) | 101.0 – 103.0°F | 38.3 – 39.4°C |
| Fever (High) | 103.1 – 105.0°F | 39.5 – 40.5°C |
| Hyperpyrexia | Above 105.0°F | Above 40.5°C |
Oral Temperature Measurement Procedure
Step 1: Wash hands and explain the procedure to the patient.
Step 2: Ensure the patient hasn’t had hot or cold drinks, food, or smoked in the last 15-30 minutes.
Step 3: Apply disposable cover to the thermometer probe if using an electronic thermometer.
Step 4: Place the thermometer under the tongue in the posterior sublingual pocket (to the side of the frenulum).
Step 5: Ask the patient to close their mouth gently around the thermometer.
Step 6: Leave in place until the electronic thermometer signals completion (usually 10-30 seconds).
Step 7: Remove the thermometer, note the reading, and dispose of the cover properly.
Step 8: Document the temperature, site, time, and any relevant observations.
Factors Affecting Body Temperature
- Age: Infants and older adults have less stable temperature regulation
- Circadian rhythm: Temperature typically lowest in early morning, highest in late afternoon/evening
- Hormonal changes: Menstrual cycle, pregnancy, and menopause affect temperature
- Exercise: Increases body temperature temporarily
- Environment: Extreme ambient temperatures affect body temperature
- Medications: Antipyretics, steroids, and some antibiotics influence temperature
Nursing Considerations for Temperature Monitoring
- Choose the appropriate site based on patient age, condition, and accessibility
- Use the same site and method for serial measurements for accurate trend analysis
- Consider age-specific normal ranges, especially for infants and older adults
- Document fever patterns (continuous, intermittent, remittent, relapsing)
- Report temperatures above 101.0°F (38.3°C) or below 96.8°F (36.0°C) promptly
- Educate patients about proper technique for home temperature monitoring
Mnemonic: “FEVER” for Temperature Assessment
F – Frequency of monitoring based on condition
E – Equipment selection appropriate for patient
V – Verify technique and proper placement
E – Evaluate pattern and associated symptoms
R – Record accurate readings and interventions
Blood Pressure Monitoring
Blood pressure monitoring is a critical assessment in community health nursing that helps screen for hypertension, evaluate cardiovascular health, monitor treatment effectiveness, and identify individuals at risk for cardiovascular disease. Accurate measurement and interpretation of blood pressure values are essential skills for community health nurses.
Blood Pressure Classification for Adults
| Category | Systolic (mmHg) | Diastolic (mmHg) |
|---|---|---|
| Normal | <120 | and <80 |
| Elevated | 120-129 | and <80 |
| Hypertension Stage 1 | 130-139 | or 80-89 |
| Hypertension Stage 2 | ≥140 | or ≥90 |
| Hypertensive Crisis | >180 | and/or >120 |
Source: American Heart Association (2017)
Equipment for Blood Pressure Measurement
- Sphygmomanometer: Aneroid, digital, or mercury (less common now)
- Blood pressure cuff: Various sizes (pediatric, standard adult, large adult, thigh)
- Stethoscope: For auscultatory method
- Alcohol wipes: For cleaning equipment between patients
Blood Pressure Measurement Procedure (Auscultatory Method)
Step 1: Explain the procedure to the patient and have them rest for 5 minutes.
Step 2: Position the patient seated with back supported, feet flat on floor, arm at heart level.
Step 3: Expose the upper arm and ensure no constrictive clothing.
Step 4: Select the appropriate cuff size (bladder width 40% of arm circumference, length 80%).
Step 5: Palpate the brachial artery in the antecubital fossa.
Step 6: Position the cuff 2-3 cm above the antecubital fossa with the center of the bladder over the brachial artery.
Step 7: Palpate the radial pulse and inflate the cuff until the pulse disappears, then inflate 30 mmHg higher.
Step 8: Place the stethoscope over the brachial artery without pressing too firmly.
Step 9: Deflate the cuff slowly (2-3 mmHg per second).
Step 10: Note the systolic pressure (first Korotkoff sound) and diastolic pressure (fifth Korotkoff sound).
Step 11: Deflate the cuff completely and remove it.
Step 12: Wait 1-2 minutes and repeat for verification.
Step 13: Document the blood pressure, patient position, arm used, and cuff size.
Home Blood Pressure Monitoring Education
Community health nurses should educate patients on proper home blood pressure monitoring techniques:
- Use a validated device with appropriate cuff size
- Measure at the same time each day (morning and evening)
- Avoid caffeine, exercise, and smoking for 30 minutes before measurement
- Sit quietly for 5 minutes before measurement
- Use proper positioning (seated, back supported, arm at heart level)
- Take 2-3 readings, 1 minute apart, and record all values
- Maintain a blood pressure log to share with healthcare providers
Factors Affecting Blood Pressure
Factors That Increase BP
- Pain, anxiety, stress
- Full bladder
- Caffeine consumption
- Nicotine use
- Certain medications (NSAIDs, decongestants)
- Talking during measurement
- Cold environment
Factors That Decrease BP
- Prolonged standing
- Dehydration
- Blood loss
- Valsalva maneuver
- Certain medications (antihypertensives)
- Warm environment
- Post-prandial state (after eating)
Mnemonic: “PRESSURE” for Accurate BP Measurement
P – Position patient properly
R – Rest patient for 5 minutes before measurement
E – Equipment should be calibrated and appropriate size
S – Support arm at heart level
S – Silence during measurement (no talking)
U – Uncross legs with feet flat on floor
R – Repeat measurement for verification
E – Empty bladder before procedure
Menstrual Cycle
The menstrual cycle is a monthly series of hormonal and physiological changes in females of reproductive age that prepares the body for potential pregnancy. In community health nursing, understanding the menstrual cycle is essential for reproductive health education, menstrual hygiene promotion, identifying abnormal patterns, and providing comprehensive women’s health care.
Normal Menstrual Cycle Characteristics
| Characteristic | Normal Range | When to Seek Healthcare |
|---|---|---|
| Cycle Length | 21-35 days (average 28 days) | Cycles consistently shorter than 21 or longer than 35 days |
| Menstrual Flow Duration | 3-7 days | Bleeding for less than 3 or more than 7 days |
| Blood Loss | 30-80 mL per cycle | Excessive bleeding (soaking through pad/tampon hourly) |
| Color | Bright red to dark red/brown | Unusual colors (gray/pink), large clots |
| Discomfort | Mild cramps, breast tenderness | Severe pain that interferes with daily activities |
Phases of the Menstrual Cycle
1. Menstrual Phase (Days 1-5)
- Shedding of endometrial lining
- Low levels of estrogen and progesterone
- FSH begins to rise, stimulating follicle development
2. Follicular Phase (Days 1-13)
- Overlaps with menstrual phase
- Rising estrogen levels
- Development of ovarian follicles
- Thickening of endometrium
3. Ovulation (Day 14 in a 28-day cycle)
- LH surge triggers release of egg from dominant follicle
- Estrogen peaks then drops briefly
- Cervical mucus becomes thin and slippery
- Most fertile period
4. Luteal Phase (Days 15-28)
- Empty follicle forms corpus luteum
- Progesterone rises, preparing endometrium for implantation
- If no pregnancy, corpus luteum degenerates
- Hormone levels fall, triggering menstruation
Hormonal Regulation of the Menstrual Cycle
| Hormone | Source | Primary Functions |
|---|---|---|
| Follicle-Stimulating Hormone (FSH) | Anterior pituitary | Stimulates follicle development and estrogen production |
| Luteinizing Hormone (LH) | Anterior pituitary | Triggers ovulation and corpus luteum formation |
| Estrogen | Ovarian follicles | Proliferates endometrium, thins cervical mucus, provides negative feedback to hypothalamus |
| Progesterone | Corpus luteum | Prepares endometrium for implantation, thickens cervical mucus |
| Gonadotropin-Releasing Hormone (GnRH) | Hypothalamus | Stimulates release of FSH and LH from pituitary |
Common Menstrual Disorders
| Disorder | Characteristics | Community Health Nursing Interventions |
|---|---|---|
| Dysmenorrhea | Painful menstruation, cramping | Education on pain management, lifestyle modifications, referral if severe |
| Amenorrhea | Absence of menstruation | Screening for causes, nutritional counseling, referral for evaluation |
| Menorrhagia | Excessive or prolonged bleeding | Anemia screening, iron supplementation education, urgent referral if severe |
| Oligomenorrhea | Infrequent menstruation | Education on cycle tracking, screening for PCOS, referral as needed |
| Premenstrual Syndrome (PMS) | Physical and emotional symptoms before menstruation | Lifestyle modifications, stress management education, symptom tracking |
Menstrual Health Assessment in Community Nursing
Step 1: Obtain a comprehensive menstrual history including:
- Age at menarche
- Cycle length and regularity
- Duration and amount of flow
- Associated symptoms
- Impact on daily activities
Step 2: Assess for menstrual disorders using validated screening tools when available.
Step 3: Evaluate impact on quality of life and functional status.
Step 4: Screen for anemia if heavy bleeding is reported.
Step 5: Provide education on normal menstrual patterns and self-care measures.
Step 6: Refer to healthcare provider for abnormal patterns or concerning symptoms.
Community Health Nursing Interventions for Menstrual Health
- Education on normal menstrual patterns and variations
- Promotion of menstrual hygiene practices
- Teaching about menstrual tracking methods (calendar, apps)
- Increasing access to menstrual hygiene products
- Screening for menstrual disorders in community settings
- Providing information on hormonal and non-hormonal management options
- Addressing cultural myths and misconceptions about menstruation
Mnemonic: “CYCLES” for Menstrual Health Assessment
C – Consistency and color of flow
Y – Years since menarche and pattern over time
C – Cycle length and regularity
L – Length of bleeding days
E – Effect on daily activities
S – Symptoms associated with menstruation
Breast Self-Examination (BSE)
Breast self-examination (BSE) is a screening method that helps individuals become familiar with the normal appearance and feel of their breasts, allowing them to detect any changes or abnormalities. While BSE is not a replacement for clinical breast examinations or mammography, it promotes breast awareness and early detection of potential breast health issues.
Importance of Breast Self-Examination
- Promotes breast awareness and familiarity with normal breast tissue
- Helps identify changes that may warrant medical attention
- Empowers individuals to take an active role in their breast health
- Can detect breast changes between clinical examinations
- Particularly important for individuals with a family history of breast cancer
Recommended Schedule
The American Cancer Society recommends breast awareness rather than structured BSE. However, for those who choose to perform BSE, the following guidelines apply:
- Perform monthly, 3-5 days after menstruation begins (when breasts are least tender and swollen)
- For postmenopausal women or those who have had hysterectomies, choose a consistent day each month
- For those on hormonal contraceptives, select a consistent day after completing the active pills
Breast Self-Examination Procedure
Step 1: Visual Inspection with Arms at Sides
- Stand in front of a mirror with good lighting
- Observe breasts for changes in size, shape, contour, or symmetry
- Look for skin changes (redness, dimpling, puckering, rash)
- Check for nipple changes (inversion, discharge, direction)
Step 2: Visual Inspection with Arms Raised
- Raise arms overhead and press hands together
- Look for the same changes as in Step 1
- Pay attention to any dimpling or puckering that becomes more apparent
Step 3: Visual Inspection with Hands on Hips
- Place hands on hips and press firmly to flex chest muscles
- Observe for asymmetry or changes in contour
- Lean forward slightly to observe how breasts hang
Step 4: Manual Examination Lying Down
- Lie down with a pillow under the right shoulder and right arm behind head
- Use the finger pads of the left hand to examine the right breast
- Apply firm, smooth pressure in a circular motion
- Cover the entire breast from collarbone to bra line and from armpit to sternum
- Use a systematic pattern (vertical lines, concentric circles, or wedges)
- Repeat on the left breast with right hand
Step 5: Manual Examination Sitting or Standing
- Repeat the manual examination while sitting or standing
- Many women find it easier to examine the upper outer quadrant while standing
- Can be performed in the shower when skin is wet and slippery
Step 6: Nipple Examination
- Gently squeeze each nipple between thumb and index finger
- Note any discharge (clear, milky, yellow, green, or bloody)
- Report any discharge to healthcare provider
What to Look For During BSE
| Finding | Description | Action |
|---|---|---|
| Lump or thickening | Firm, usually painless area that feels different from surrounding tissue | Seek medical evaluation promptly |
| Skin changes | Dimpling, puckering, redness, scaling, or orange-peel appearance | Report to healthcare provider |
| Nipple changes | New inversion, retraction, or deviation in direction | Seek medical evaluation |
| Nipple discharge | Spontaneous discharge, especially if bloody or from one breast only | Report to healthcare provider promptly |
| Change in size or shape | Asymmetry that is new or changing | Seek medical evaluation |
Community Health Nursing Education Points
- BSE is one component of a comprehensive breast health plan that includes clinical breast exams and mammography
- BSE helps individuals become familiar with their normal breast tissue
- Breast tissue normally feels lumpy and varies throughout the menstrual cycle
- Not all breast changes indicate cancer, but all unusual findings should be evaluated
- Provide reassurance that most breast lumps are benign
- Emphasize the importance of prompt medical evaluation for any concerning changes
Mnemonic: “BREAST” for Self-Examination
B – Begin with visual inspection
R – Raise arms and check for changes
E – Examine systematically with a pattern
A – All areas covered (collarbone to bra line, armpit to sternum)
S – Squeeze nipple to check for discharge
T – Track and report changes promptly
Testicular Self-Examination (TSE)
Testicular self-examination (TSE) is a screening procedure that enables males to check their testicles for abnormalities that could indicate testicular cancer or other conditions. While not universally recommended as a screening method, TSE promotes awareness of testicular health and can lead to early detection of testicular abnormalities, particularly in high-risk individuals.
Importance of Testicular Self-Examination
- Promotes awareness of normal testicular anatomy and feel
- Helps identify abnormalities that may require medical attention
- May lead to early detection of testicular cancer, which is highly treatable when caught early
- Particularly important for high-risk individuals (history of undescended testicle, family history of testicular cancer)
- Empowers males to take an active role in their reproductive health
Recommended Schedule
For those who choose to perform TSE, the following schedule is recommended:
- Perform monthly after a warm bath or shower when the scrotum is relaxed
- Choose a consistent day each month to establish a routine
- Start in adolescence and continue throughout adulthood
Testicular Self-Examination Procedure
Step 1: Preparation
- Perform after a warm shower or bath when the scrotum is relaxed
- Stand in front of a mirror to observe any visual changes
- Check for any swelling, lumps, or changes in skin color
Step 2: Examination of Each Testicle
- Hold the scrotum in the palms of both hands
- Use both hands to gently roll each testicle between thumbs and fingers
- One testicle may be larger or hang lower than the other (normal variation)
Step 3: Feel for Normal Anatomy
- Locate the epididymis, a soft, rope-like structure on the back of each testicle
- Become familiar with this normal structure to avoid confusing it with abnormalities
- Note the normal size, shape, and consistency of each testicle
Step 4: Check for Abnormalities
- Feel for any hard lumps, nodules, or changes in consistency
- Note any unusual heaviness or significant difference between testicles
- Check for any pain or tenderness during examination
Step 5: Documentation and Follow-up
- Make note of any changes or concerns
- Seek medical attention promptly for any abnormalities
- Continue monthly examinations to monitor for changes
What to Look For During TSE
| Finding | Description | Action |
|---|---|---|
| Lump or nodule | Hard, painless mass on the testicle (most common sign of testicular cancer) | Seek medical evaluation promptly |
| Swelling | Enlargement of one or both testicles | Report to healthcare provider |
| Pain or discomfort | Persistent ache or sharp pain in testicle or scrotum | Seek medical evaluation |
| Heaviness | Sensation of heaviness in the scrotum | Report to healthcare provider |
| Change in consistency | Testicle feels harder or has different texture | Seek medical evaluation |
Conditions That May Be Detected Through TSE
| Condition | Characteristics | Nursing Considerations |
|---|---|---|
| Testicular Cancer | Painless lump or swelling; may present with heaviness | Emphasize importance of prompt medical evaluation; highly curable when detected early |
| Epididymitis | Inflammation of epididymis; painful swelling, often with redness | Educate about STI prevention; typically treated with antibiotics |
| Orchitis | Inflammation of testicle; painful swelling, often with fever | Discuss importance of mumps vaccination; provide comfort measures education |
| Hydrocele | Fluid collection around testicle; painless swelling | Reassure about benign nature; may require surgical correction if large |
| Varicocele | Enlarged veins within scrotum; feels like “bag of worms” | Educate about potential fertility implications; typically on left side |
Community Health Nursing Education Points
- Testicular cancer most commonly affects males between 15 and 35 years of age
- Risk factors include cryptorchidism (undescended testicle), family history, and previous testicular cancer
- Most testicular masses are not cancer, but all require medical evaluation
- Testicular cancer has one of the highest cure rates of all cancers when detected early
- Address embarrassment and privacy concerns that may prevent males from performing TSE
- Emphasize that TSE is a simple procedure that takes only a few minutes
Mnemonic: “TESTICLE” for Self-Examination
T – Time it after a warm shower
E – Examine one at a time
S – Size and shape should be noted
T – Texture should be smooth and firm
I – Identify the epididymis (normal structure)
C – Check for lumps, swelling, or pain
L – Look for changes from previous examinations
E – Evaluate any concerns with a healthcare provider
Warning Signs of Various Diseases
Recognizing the early warning signs of diseases is crucial for timely intervention and improved health outcomes. Community health nurses play a vital role in educating the public about these warning signs and encouraging appropriate healthcare-seeking behavior. This section covers common warning signs for several major disease categories that community health nurses should be familiar with.
Cardiovascular Disease Warning Signs
Chest Pain or Discomfort
Pressure, squeezing, fullness, or pain in the center or left side of the chest that lasts more than a few minutes or comes and goes
Action: Call emergency services immediately (911/local emergency number)
Upper Body Discomfort
Pain or discomfort in one or both arms, back, neck, jaw, or stomach
Action: Seek immediate medical attention
Shortness of Breath
Difficulty breathing that occurs with or without chest discomfort
Action: Call emergency services
Other Signs
Cold sweat, nausea, lightheadedness, extreme fatigue
Action: Seek immediate medical attention
Stroke Warning Signs (BE FAST)
Mnemonic: “BE FAST”
B – Balance: Sudden loss of balance or coordination
E – Eyes: Sudden trouble seeing in one or both eyes
F – Face: Facial drooping, especially on one side
A – Arms: Weakness or numbness in one arm
S – Speech: Slurred speech or difficulty speaking
T – Time: Time to call emergency services immediately
Action: Call emergency services immediately if any of these signs appear. Note the time when symptoms first appeared.
Diabetes Warning Signs
Frequent Urination
Particularly noticeable at night (nocturia)
Excessive Thirst
Persistent, unquenchable thirst despite drinking fluids
Unexplained Weight Loss
Despite normal or increased appetite
Extreme Fatigue
Persistent tiredness and weakness
Blurred Vision
Changes in visual acuity
Slow-Healing Sores
Cuts and wounds that heal slowly
Action: Schedule an appointment with a healthcare provider for diabetes screening
Cancer Warning Signs (CAUTION)
Mnemonic: “CAUTION”
C – Change in bowel or bladder habits
A – A sore that does not heal
U – Unusual bleeding or discharge
T – Thickening or lump in breast, testicles, or elsewhere
I – Indigestion or difficulty swallowing
O – Obvious change in wart or mole
N – Nagging cough or hoarseness
Action: Make an appointment with a healthcare provider for evaluation if any of these symptoms persist for more than two weeks
Respiratory Disease Warning Signs
| Warning Sign | Description | Potential Conditions |
|---|---|---|
| Chronic Cough | Cough lasting more than 8 weeks | COPD, asthma, lung cancer, tuberculosis |
| Shortness of Breath | Dyspnea with minimal exertion or at rest | COPD, asthma, pulmonary embolism, heart failure |
| Chronic Mucus Production | Persistent phlegm production | COPD, bronchiectasis, chronic bronchitis |
| Wheezing | High-pitched whistling sound during breathing | Asthma, COPD, bronchitis |
| Coughing Up Blood | Hemoptysis | Tuberculosis, lung cancer, pulmonary embolism |
Mental Health Warning Signs
Changes in Mood or Behavior
Persistent sadness, irritability, mood swings, or withdrawal from activities
Changes in Sleep Patterns
Insomnia, oversleeping, or disrupted sleep
Changes in Appetite
Significant weight gain or loss, eating disorders
Difficulty Concentrating
Problems with focus, memory, or decision-making
Thoughts of Death
Suicidal ideation or preoccupation with death
Action for Suicidal Thoughts: Call National Suicide Prevention Lifeline (988) or seek immediate professional help
Community Health Nursing Interventions
- Conduct community education programs about disease warning signs
- Develop and distribute educational materials in multiple languages
- Implement screening programs to identify high-risk individuals
- Provide guidance on appropriate healthcare-seeking behavior
- Address barriers to healthcare access that delay treatment
- Coordinate community resources for preventive health measures
- Conduct follow-up with individuals identified with warning signs
Mnemonic: “DETECT” for Community Warning Sign Education
D – Deliver clear, concise information about warning signs
E – Emphasize the importance of timely action
T – Target high-risk populations with focused education
E – Evaluate understanding through teach-back methods
C – Connect individuals to appropriate healthcare resources
T – Track outcomes and adjust educational approaches accordingly
Tests: Urine for Sugar and Albumin, Blood Sugar, Hemoglobin
Diagnostic testing is an essential component of community health nursing practice, providing objective data for health screening, disease detection, and monitoring treatment effectiveness. This section covers common tests performed in community settings, including urine testing for sugar and albumin, blood glucose monitoring, and hemoglobin assessment.
Urine Test for Sugar and Albumin
Urine testing for glucose (sugar) and albumin (protein) is a simple, non-invasive screening method used in community health settings to detect potential kidney disease, diabetes, and other conditions.
Equipment Needed
- Clean specimen container
- Urine reagent strips (dipsticks)
- Timer or watch with second hand
- Clean, dry surface for dipstick
- Gloves
- Color chart for interpretation
Urine Specimen Collection Procedure
Step 1: Explain the procedure to the patient.
Step 2: Provide a clean specimen container and instructions for a clean-catch midstream specimen:
- Wash hands thoroughly
- Clean the genital area with provided wipes (front to back for females)
- Start urinating into the toilet
- After the urine flow is established, collect the sample in the container without touching the inside of the container
- Finish urinating into the toilet
- Secure the lid on the container
Step 3: Receive the specimen and ensure it is properly labeled with patient identification and collection time.
Step 4: Test the specimen within 30 minutes of collection for most accurate results.
Urine Dipstick Testing Procedure
Step 1: Don gloves and ensure proper hand hygiene.
Step 2: Check the expiration date on the dipstick container.
Step 3: Remove one dipstick, immediately close the container tightly.
Step 4: Completely immerse the reagent areas of the strip in fresh, well-mixed urine.
Step 5: Remove the strip immediately, drawing the edge against the rim of the container to remove excess urine.
Step 6: Hold the strip horizontally to prevent mixing of chemicals between reagent areas.
Step 7: Compare each reagent area with the corresponding color chart at the specified time (usually 30-60 seconds depending on the parameter).
Step 8: Record the results promptly.
Step 9: Dispose of the used dipstick and specimen according to facility protocol.
Interpretation of Results
| Parameter | Normal Finding | Abnormal Finding | Clinical Significance |
|---|---|---|---|
| Glucose | Negative | Positive (trace to 4+) | May indicate diabetes mellitus, pregnancy, stress, or other conditions with elevated blood glucose |
| Protein (Albumin) | Negative to trace | Positive (1+ to 4+) | May indicate kidney disease, urinary tract infection, preeclampsia, or other conditions affecting renal function |
Blood Glucose Testing
Blood glucose monitoring is used to assess glycemic control in individuals with diabetes, screen for diabetes, and monitor response to treatment. In community settings, capillary blood glucose testing using a glucometer is commonly performed.
Equipment Needed
- Glucometer (blood glucose meter)
- Test strips compatible with the glucometer
- Lancing device and sterile lancets
- Alcohol swabs
- Gloves
- Cotton balls or gauze
- Sharps container
Blood Glucose Testing Procedure
Step 1: Explain the procedure to the patient.
Step 2: Assemble the equipment and perform hand hygiene.
Step 3: Don gloves.
Step 4: Turn on the glucometer and check that it is functioning properly.
Step 5: Insert a test strip into the glucometer according to manufacturer’s instructions.
Step 6: Select a puncture site (side of fingertip is preferred; avoid central finger pad).
Step 7: Clean the site with an alcohol swab and allow it to dry completely.
Step 8: Prepare the lancing device according to manufacturer’s instructions.
Step 9: Hold the finger firmly and perform the puncture perpendicular to the fingerprint lines.
Step 10: Wipe away the first drop of blood with a clean cotton ball or gauze.
Step 11: Gently squeeze the finger to obtain a hanging drop of blood.
Step 12: Touch the drop of blood to the test strip according to manufacturer’s instructions.
Step 13: Apply pressure to the puncture site with cotton ball or gauze.
Step 14: Read and record the result displayed on the glucometer.
Step 15: Dispose of all materials appropriately (lancet in sharps container).
Step 16: Remove gloves and perform hand hygiene.
Step 17: Document the procedure and result.
Interpretation of Blood Glucose Results
| Classification | Fasting Blood Glucose | Random Blood Glucose | 2-Hour Postprandial |
|---|---|---|---|
| Normal | 70-99 mg/dL (3.9-5.5 mmol/L) | <140 mg/dL (<7.8 mmol/L) | <140 mg/dL (<7.8 mmol/L) |
| Prediabetes | 100-125 mg/dL (5.6-6.9 mmol/L) | N/A | 140-199 mg/dL (7.8-11.0 mmol/L) |
| Diabetes | ≥126 mg/dL (≥7.0 mmol/L) | ≥200 mg/dL (≥11.1 mmol/L) + symptoms | ≥200 mg/dL (≥11.1 mmol/L) |
| Hypoglycemia | <70 mg/dL (<3.9 mmol/L) | <70 mg/dL (<3.9 mmol/L) | <70 mg/dL (<3.9 mmol/L) |
Hemoglobin Testing
Hemoglobin testing measures the amount of hemoglobin in the blood and is used to screen for anemia, assess blood loss, monitor response to treatment, and evaluate various health conditions. In community settings, portable hemoglobinometers are often used for point-of-care testing.
Equipment Needed
- Portable hemoglobinometer
- Hemoglobin test cuvettes or strips
- Lancing device and sterile lancets
- Alcohol swabs
- Gloves
- Cotton balls or gauze
- Sharps container
Hemoglobin Testing Procedure
Step 1: Explain the procedure to the patient.
Step 2: Assemble the equipment and perform hand hygiene.
Step 3: Don gloves.
Step 4: Turn on the hemoglobinometer and ensure it is calibrated and functioning properly.
Step 5: Prepare the test cuvette or strip according to manufacturer’s instructions.
Step 6: Select a puncture site (side of fingertip is preferred).
Step 7: Clean the site with an alcohol swab and allow it to dry completely.
Step 8: Perform the finger puncture with the lancet.
Step 9: Wipe away the first drop of blood with a clean cotton ball or gauze.
Step 10: Collect the blood sample in the cuvette or on the test strip as directed by manufacturer.
Step 11: Insert the filled cuvette or test strip into the analyzer within the specified time frame.
Step 12: Apply pressure to the puncture site with cotton ball or gauze.
Step 13: Read and record the hemoglobin result displayed on the analyzer.
Step 14: Dispose of all materials appropriately (lancet in sharps container).
Step 15: Remove gloves and perform hand hygiene.
Step 16: Document the procedure and result.
Normal Hemoglobin Ranges
| Population Group | Normal Range (g/dL) | Normal Range (g/L) |
|---|---|---|
| Adult Males | 13.5 – 17.5 g/dL | 135 – 175 g/L |
| Adult Females | 12.0 – 15.5 g/dL | 120 – 155 g/L |
| Pregnant Females | 11.0 – 14.0 g/dL | 110 – 140 g/L |
| Children (2-12 years) | 11.5 – 15.5 g/dL | 115 – 155 g/L |
| Newborns | 14.0 – 24.0 g/dL | 140 – 240 g/L |
WHO Classification of Anemia
| Population | Mild Anemia | Moderate Anemia | Severe Anemia |
|---|---|---|---|
| Adult Males | 11.0 – 12.9 g/dL | 8.0 – 10.9 g/dL | <8.0 g/dL |
| Adult Females (non-pregnant) | 11.0 – 11.9 g/dL | 8.0 – 10.9 g/dL | <8.0 g/dL |
| Pregnant Females | 10.0 – 10.9 g/dL | 7.0 – 9.9 g/dL | <7.0 g/dL |
| Children 6-59 months | 10.0 – 10.9 g/dL | 7.0 – 9.9 g/dL | <7.0 g/dL |
Community Health Nursing Considerations for Diagnostic Testing
- Ensure privacy and comfort during testing procedures
- Use culturally sensitive approaches when explaining procedures
- Consider literacy levels when providing instructions
- Address fears or misconceptions about testing
- Ensure proper calibration and quality control of testing equipment
- Develop clear protocols for follow-up of abnormal results
- Establish referral pathways for further diagnostic evaluation
- Provide education about the meaning of test results
Mnemonic: “RESULTS” for Diagnostic Testing in Community Settings
R – Ready equipment and environment
E – Explain procedure clearly
S – Sterile technique when required
U – Understand implications of results
L – Log results accurately
T – Timely follow-up for abnormal findings
S – Share results and explain significance to patient
Good Practices in Community Health Assessment from Around the World
Community health nursing practices vary globally, influenced by cultural, social, and economic factors. Here are some innovative approaches to community health assessment from different regions that could enrich nursing practice:
Japan: Community-Based Prevention Program
Japan’s community-based health promotion program, “Healthy Japan 21,” integrates regular health screenings with community involvement. Community health nurses conduct regular anthropometric measurements and health checks in local community centers, making preventive care more accessible and culturally acceptable.
Sweden: Digital Health Assessment Tools
Swedish community health nurses utilize digital platforms for remote monitoring of vital signs and anthropometric measurements. Patients can upload their home measurements, allowing nurses to track trends and intervene earlier. This approach has been particularly effective in rural areas with limited healthcare access.
Rwanda: Community Health Worker Integration
Rwanda’s community health program trains local health workers to perform basic assessments, including anthropometric measurements and screening tests. These workers collaborate closely with community health nurses, creating a tiered approach that maximizes limited healthcare resources while ensuring quality care.
Australia: Cultural Adaptation of Health Assessments
Australia’s approach to Aboriginal and Torres Strait Islander communities involves culturally adapted health assessments. Community health nurses are trained in culturally respectful practices and modify assessment techniques to align with indigenous health beliefs and practices, improving engagement and outcomes.
India: Mobile Health Clinics
India’s mobile health clinic initiative brings community health assessments to remote villages. Equipped with portable diagnostic equipment, these clinics enable community health nurses to conduct comprehensive assessments, including anthropometric measurements, hemoglobin testing, and urine screening in areas without permanent healthcare facilities.
These global practices demonstrate the importance of adapting community health assessment approaches to local contexts while maintaining standard measurement techniques. By incorporating elements of these successful programs, community health nurses can enhance their practice and improve population health outcomes.

Social Development Assessment
Social development assessment evaluates an individual’s ability to interact with others, establish relationships, and function within their community. In community health nursing, assessing social development helps identify potential developmental delays, screen for social support needs, and guide health promotion interventions.
Key Components of Social Development Assessment
Social Development Milestones by Age
Social Development Assessment Procedure
Step 1: Gather background information about the individual’s social environment.
Step 2: Observe social interactions during the assessment.
Step 3: Ask age-appropriate questions about social activities and relationships.
Step 4: Use standardized screening tools when appropriate (e.g., Ages and Stages Questionnaire).
Step 5: Assess social support networks using tools like ecomaps or genograms.
Step 6: Document observations and screening results.
Step 7: Develop intervention plans for identified concerns.
Community Health Nursing Interventions for Social Development
Mnemonic: “SOCIAL” for Social Development Assessment
S – Support systems and networks
O – Observe interactions during assessment
C – Communication skills (verbal and non-verbal)
I – Individual developmental stage
A – Adaptability to social situations
L – Life experiences affecting social development