Jaundice Management
Community Health Nursing Perspectives
Table of Contents
Introduction
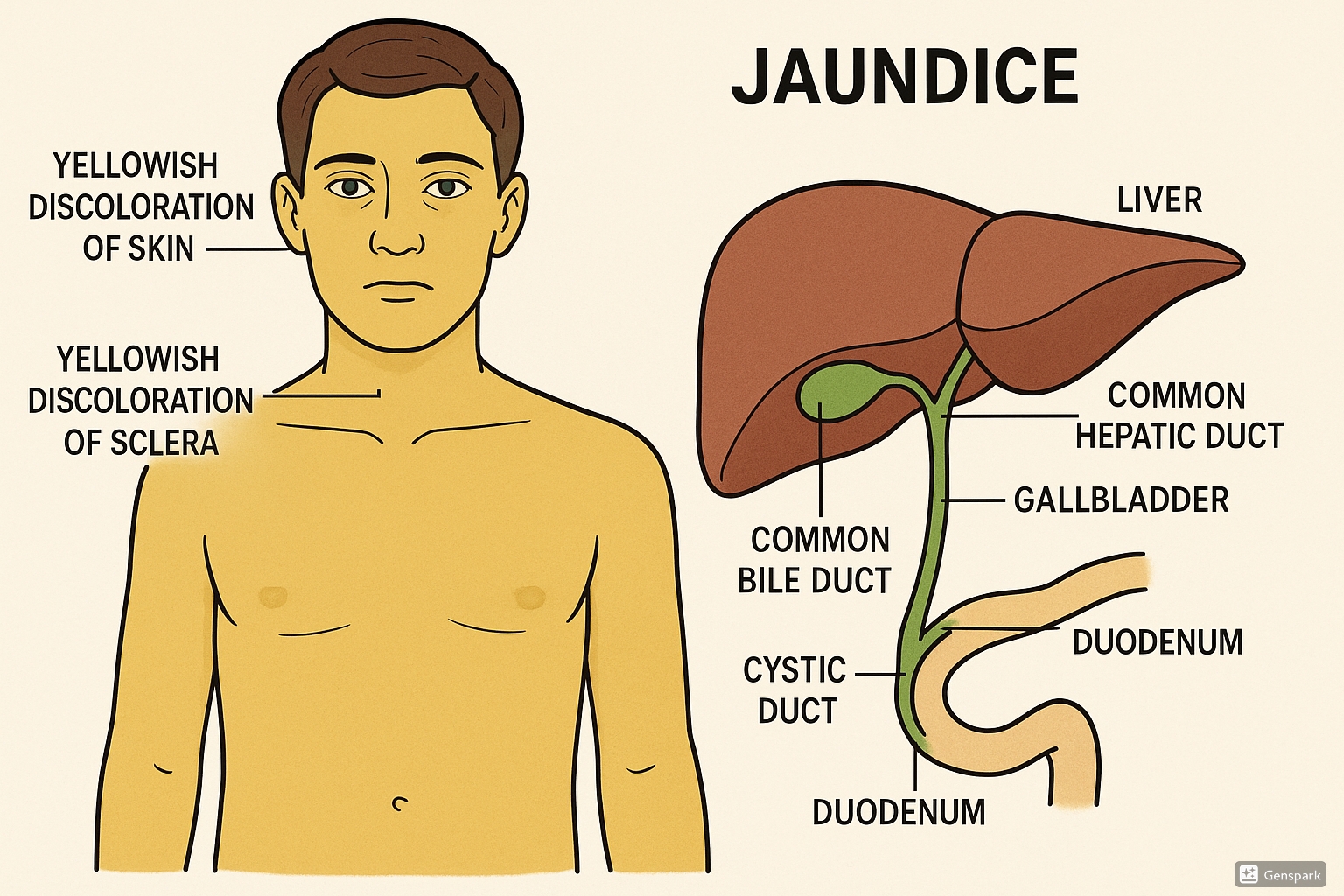
Jaundice, also known as icterus, is a common clinical manifestation characterized by yellowing of the skin, mucous membranes, and sclerae due to hyperbilirubinemia. For community health nurses, understanding jaundice is crucial as it can be an indicator of various underlying conditions ranging from benign to life-threatening.
Community health nurses are often the first healthcare providers to encounter patients with jaundice, especially in rural and underserved areas. Early recognition, prompt intervention, and appropriate referral can significantly impact patient outcomes. This comprehensive guide covers the essential aspects of jaundice management from a community health nursing perspective.
Definition & Pathophysiology
Jaundice is defined as yellowish discoloration of the skin, sclera, and mucous membranes resulting from excessive bilirubin deposition in tissues. It becomes clinically apparent when serum bilirubin levels exceed 2-3 mg/dL.
Bilirubin Metabolism
- Production: Bilirubin is produced from the breakdown of hemoglobin in aged or damaged red blood cells.
- Transportation: Unconjugated (indirect) bilirubin binds to albumin and travels to the liver.
- Conjugation: In hepatocytes, bilirubin is converted to water-soluble conjugated (direct) bilirubin.
- Excretion: Conjugated bilirubin is excreted into bile and ultimately eliminated through feces.
Pathophysiological Basis
Jaundice occurs due to disruption in bilirubin metabolism at various stages:
| Stage | Process Affected | Result |
|---|---|---|
| Pre-hepatic | Excessive production of bilirubin | ↑ Unconjugated bilirubin |
| Hepatic | Impaired uptake, conjugation, or excretion by liver | ↑ Both unconjugated and conjugated bilirubin |
| Post-hepatic | Obstruction of bile flow | ↑ Conjugated bilirubin |
Types of Jaundice
Understanding the different types of jaundice helps community health nurses in effective screening and appropriate referrals.
1. Pre-hepatic Jaundice
- Caused by excessive RBC hemolysis
- Elevated unconjugated bilirubin
- Examples: Sickle cell disease, Thalassemia, G6PD deficiency, Malaria
- Features: Dark urine, normal colored stools
2. Hepatic Jaundice
- Caused by liver dysfunction
- Mixed hyperbilirubinemia
- Examples: Hepatitis, Cirrhosis, Drug-induced liver injury
- Features: Dark urine, pale stools, hepatomegaly
3. Post-hepatic Jaundice
- Caused by biliary obstruction
- Elevated conjugated bilirubin
- Examples: Gallstones, Bile duct strictures, Pancreatic cancer
- Features: Dark urine, clay-colored stools, pruritus
Special Types of Jaundice
Physiological Jaundice in Newborns
Common and usually benign condition affecting up to 60% of full-term and 80% of preterm infants.
Causes: Immature liver, increased bilirubin production, enterohepatic circulation
Pathological Jaundice in Newborns
Requires immediate attention as it can lead to kernicterus and neurological damage.
Causes: Blood group incompatibility, infections, metabolic disorders
Mnemonic: “PH-JAP” for Jaundice Classification
- P – Pre-hepatic (Production excessive)
- H – Hepatic (Hepatocellular dysfunction)
- J – Journey blocked (Obstructive)
- A – Assess urine & stool color
- P – Patient history crucial for diagnosis
Screening & Diagnosis
Early identification of jaundice through systematic screening is vital in community health practice. Community health nurses should follow a structured approach to screen, diagnose, and determine the severity of jaundice.
Clinical Assessment
History Taking
- Onset and progression of symptoms
- Associated symptoms (fever, abdominal pain, pruritus)
- Recent medications and herbal remedies
- Travel history and exposure to hepatitis
- Alcohol consumption pattern
- Family history of liver or blood disorders
Physical Examination
- Inspection: Yellow discoloration of sclera, skin, mucous membranes
- Palpation: Liver span, tenderness, masses
- Signs of chronic liver disease: Spider angiomas, palmar erythema
- Abdominal examination: Ascites, splenomegaly
- Neurological examination: Encephalopathy signs
Clinical Pearl:
Always examine jaundice in natural light. Yellow discoloration typically follows a cephalocaudal progression, first appearing in sclera (visible at bilirubin levels >2 mg/dL), then face, trunk, and finally extremities.
Laboratory Investigations
| Test Category | Specific Tests | Significance |
|---|---|---|
| Liver Function Tests | Total bilirubin, Direct/Indirect bilirubin, ALT, AST, ALP, GGT, Albumin | Pattern helps differentiate type of jaundice |
| Complete Blood Count | Hemoglobin, WBC, Platelet count, Peripheral smear | Indicates hemolysis or infection |
| Coagulation Profile | PT/INR, aPTT | Evaluates liver synthetic function |
| Viral Markers | HBsAg, Anti-HCV, HAV IgM | Identifies viral hepatitis |
| Additional Tests | Reticulocyte count, Direct Coombs test, Iron studies | Helpful in hemolytic jaundice |
Imaging Studies
- Ultrasound abdomen: First-line imaging, evaluates liver size, texture, biliary dilatation, gallstones
- CT scan: Better visualization of liver parenchyma, masses, and biliary tract
- MRCP (Magnetic Resonance Cholangiopancreatography): Non-invasive visualization of biliary tree
- ERCP (Endoscopic Retrograde Cholangiopancreatography): Both diagnostic and therapeutic for biliary obstruction
Special Screening Considerations
Neonatal Jaundice Screening
- Visual assessment under natural daylight
- Transcutaneous bilirubinometry (non-invasive)
- Serum bilirubin if TcB ≥ 12 mg/dL
- Plot on hour-specific nomogram
- Follow-up within 24-48 hours of discharge
Community Screening Programs
- High-risk population identification
- Hepatitis screening in endemic areas
- Awareness and education campaigns
- Health camps with basic liver function testing
- Follow-up system for identified cases
Standing Orders: Definition & Uses
Definition
Standing orders are written documents containing rules, policies, procedures, regulations, and orders for the conduct of patient care in various clinical situations. They are generally established and approved by a medical facility or practice group.
Role in Jaundice Management
Standing orders enable community health nurses to initiate appropriate care for patients with jaundice without having to contact a physician for every action, particularly in remote areas with limited medical access.
| Aspect | Standing Order Components for Jaundice |
|---|---|
| Assessment |
|
| Laboratory Tests |
|
| Interventions |
|
| Referral Criteria |
|
| Documentation |
|
Sample Standing Order for Community Health Nurse
STANDING ORDER: JAUNDICE ASSESSMENT AND INITIAL MANAGEMENT
Purpose:
To guide community health nurses in the assessment and initial management of patients presenting with jaundice.
Assessment Authorization:
- Complete clinical assessment using standardized jaundice assessment form
- Order the following laboratory tests:
- Total and direct bilirubin
- ALT, AST, ALP, GGT, albumin
- Complete blood count
- Prothrombin time/INR
- Basic metabolic panel
- Arrange for abdominal ultrasound if available
Intervention Authorization:
- Initiate oral rehydration if no contraindications
- Provide dietary counseling (low fat, high carbohydrate diet)
- Administer antipruritic medication as per protocol:
- Cholestyramine 4g PO up to TID if cholestatic pattern (high direct bilirubin, elevated ALP)
- Antihistamines for pruritus (Diphenhydramine 25mg PO q6h PRN)
URGENT Referral Criteria (any of the following):
- Total bilirubin >10 mg/dL
- Direct bilirubin >5 mg/dL
- ALT or AST >500 U/L
- INR >1.5
- Altered mental status, fever >38°C, severe abdominal pain
- Signs of dehydration or hemodynamic instability
Approved by: _________________________ Date: ___________
Medical Director
Benefits of Standing Orders in Jaundice Management:
- Standardizes care across different community settings
- Reduces delay in initiating appropriate interventions
- Maximizes the scope of practice for community health nurses
- Improves efficiency in resource-limited settings
- Ensures consistent documentation and follow-up
Primary Care Management
Primary care management of jaundice focuses on supportive care, addressing uncomfortable symptoms, and preventing complications while treating the underlying cause.
General Management Principles
Hydration
- Encourage adequate fluid intake (2-3L daily)
- Monitor for dehydration
- IV fluids if oral intake inadequate
Nutrition
- Small, frequent meals
- Low-fat diet if cholestatic jaundice
- Protein restriction if encephalopathy
- Medium-chain triglycerides
Rest
- Adequate physical rest
- Avoidance of strenuous activities
- Sleep hygiene counseling
Symptom Management
| Symptom | Nursing Interventions | Medical Management |
|---|---|---|
| Pruritus |
|
|
| Fatigue |
|
|
| Nausea/Vomiting |
|
|
| Abdominal Pain |
|
|
Special Considerations for Neonatal Jaundice
Phototherapy
Primary intervention for moderate neonatal jaundice
- Expose maximum skin surface
- Shield eyes and genitalia
- Monitor hydration status
- Regular temperature monitoring
- Position change every 2 hours
- Interrupt only for feeding and brief parental contact
Breastfeeding Management
Breastfeeding should continue during treatment
- Increase frequency (8-12 times/day)
- Monitor for adequate hydration
- Supplementation only if medically indicated
- Lactation support as needed
- Education on proper latch and positioning
Caution:
Avoid the following medications in patients with jaundice due to hepatic dysfunction:
- Acetaminophen (high doses)
- NSAIDs
- Sedatives/hypnotics
- Aminoglycosides
- Isoniazid
- Tetracyclines
- Methotrexate
- Statins
- Some anti-epileptics
Patient Education
Key Educational Topics
- Disease Process: Simple explanation of jaundice and the underlying cause
- Diet: Specific dietary recommendations based on the type of jaundice
- Medications: Purpose, dosage, schedule, and potential side effects
- Warning Signs: Symptoms requiring immediate medical attention
- Follow-up Care: Importance of regular monitoring and appointments
- Liver Protection: Avoiding alcohol, hepatotoxic medications, and herbs
- Infection Prevention: Hand hygiene and avoiding high-risk exposures
Mnemonic: “YELLOWS” for Patient Education in Jaundice
- Y – Your symptoms and when to seek help
- E – Eating guidelines and nutrition
- L – Liver protection strategies
- L – Laboratory tests and follow-up
- O – Oral medication instructions
- W – Water and hydration importance
- S – Self-care and symptom management
First Aid & Emergencies
While jaundice itself is not typically an emergency, certain accompanying conditions or complications require immediate intervention.
Emergency Conditions Associated with Jaundice
1. Acute Liver Failure
Signs & Symptoms:
- Jaundice + altered mental status
- Coagulopathy (INR > 1.5)
- Hypoglycemia
- Hepatic encephalopathy
First Aid:
- Secure airway if encephalopathic
- IV access and fluid resuscitation
- Glucose monitoring & correction
- Position in recovery position if altered mental status
- Immediate transport to hospital
2. Ascending Cholangitis (Charcot’s Triad)
Signs & Symptoms:
- Jaundice + fever + right upper quadrant pain
- Hypotension
- Mental confusion
First Aid:
- Position of comfort (usually semi-recumbent)
- IV access if available
- Monitor vital signs every 15 minutes
- Nothing by mouth
- Urgent transport to hospital
3. Severe Hemolysis
Signs & Symptoms:
- Jaundice + pallor + tachycardia
- Fatigue and weakness
- Dark urine
- Shortness of breath
First Aid:
- Rest in comfortable position
- Oxygen supplementation if available
- IV access if possible
- Transport to hospital
4. Severe Acute Pancreatitis with Jaundice
Signs & Symptoms:
- Jaundice + severe epigastric pain radiating to back
- Nausea and vomiting
- Fever
- Signs of shock
First Aid:
- Nothing by mouth
- Position for comfort (often leaning forward)
- IV access if available
- Monitor vital signs
- Urgent transport to emergency facility
First Aid for Neonatal Jaundice
Mild to Moderate Neonatal Jaundice
First Aid Measures:
- Encourage frequent breastfeeding (10-12 times/day)
- Expose to indirect sunlight through window glass for short periods
- Monitor hydration status
- Observe for worsening signs
- Arrange prompt medical evaluation
Severe Neonatal Jaundice (Emergency)
Warning Signs:
- Extreme yellow coloration extending to extremities
- Poor feeding or lethargy
- High-pitched cry
- Arching of back, neck (opisthotonus)
- Fever or hypothermia
First Aid:
- Immediate medical attention – call emergency services
- Maintain temperature
- Continue breastfeeding if alert
- Position safely to maintain airway
Critical Warning Signs Requiring Emergency Care:
- Altered mental status or confusion
- Severe abdominal pain
- High fever with jaundice
- Bleeding tendencies (gums, nose, bruising)
- Rapid onset of jaundice (< 24-48 hours)
- Hypotension or tachycardia
- Severe dehydration
- Inability to tolerate oral intake
Emergency Assessment Tool
RAPID JAUNDICE EMERGENCY ASSESSMENT
Any abnormal findings warrant prompt medical attention
Community First Responder Kit for Jaundice Emergencies
- Disposable gloves
- Basic airway management supplies
- IV access equipment (if trained)
- Glucose monitoring device
- Pulse oximeter
- Blood pressure monitoring equipment
- Emergency contact list of nearby hospitals with liver specialists
- Jaundice assessment tool
- Emergency transport plan
Referral Guidelines
Determining when and where to refer patients with jaundice is a critical responsibility for community health nurses. Timely referral can significantly impact patient outcomes.
Referral Decision Criteria
| Urgency Level | Clinical Findings | Referral Destination | Time Frame |
|---|---|---|---|
| Emergency |
|
Emergency department with critical care capabilities | Immediate (call ambulance) |
| Urgent |
|
Hospital emergency department | Same day |
| Semi-urgent |
|
Gastroenterologist or internal medicine specialist | Within 1-3 days |
| Routine |
|
Primary care physician or gastroenterologist | Within 1-2 weeks |
Special Referral Considerations for Neonatal Jaundice
| Age | Total Bilirubin Level | Other Factors | Referral Action |
|---|---|---|---|
| <24 hours | Any visible jaundice | – | Immediate referral to pediatrician |
| 24-48 hours | >10 mg/dL | – | Urgent referral |
| 48-72 hours | >15 mg/dL | – | Urgent referral |
| >72 hours | >17 mg/dL | – | Urgent referral |
| Any age | Any level | Signs of acute bilirubin encephalopathy | Emergency referral |
| Any age | Rising >5 mg/dL/day | – | Urgent referral |
Referral Documentation
Essential Information to Include
- Patient demographics and contact information
- Detailed history of present illness
- Onset and progression of jaundice
- Associated symptoms
- Vital signs and physical examination findings
- Laboratory results (if available)
- Imaging results (if available)
- Interventions already provided
- Current medications
- Allergies
Sample Referral Format
URGENT REFERRAL: JAUNDICE
Date/Time: [Insert]
Patient: [Name], [Age], [Sex]
Chief Complaint: Progressive jaundice x 3 days
History: Onset, progression, associated symptoms
Vitals: BP, HR, RR, Temp, SpO2
Exam: Key findings, including severity of jaundice
Labs: Available results
Interventions: Actions taken
Reason for Referral: Specific concern
Referring Nurse: [Name & Contact]
Referral Pathway
Best Practice Tip:
Establish and maintain a directory of referral resources including contact information, specialty services, and referral procedures for various healthcare facilities in your region. Update this information regularly and ensure it’s accessible to all community health nurses.
Community Health Nurse’s Role
Community health nurses play a pivotal role in the comprehensive management of jaundice through various functions that span prevention, early detection, management, and follow-up care.
Prevention & Health Promotion
- Conduct hepatitis vaccination campaigns
- Educate communities about liver health and protection
- Promote safe water and food practices to prevent hepatitis A
- Advocate for safe injection practices to prevent hepatitis B and C
- Raise awareness about alcohol-related liver disease
- Educate pregnant women about neonatal jaundice
- Promote early and exclusive breastfeeding
Screening & Early Detection
- Conduct routine health assessments with jaundice screening
- Implement newborn jaundice screening protocols
- Organize community screening for viral hepatitis in high-risk areas
- Train community health workers to recognize jaundice
- Conduct home visits for newborn jaundice assessment
- Create referral linkages for confirmatory testing
- Follow up on laboratory results and ensure proper communication
Case Management
- Implement standing orders for jaundice management
- Provide home-based care for stable patients with jaundice
- Monitor treatment adherence and effectiveness
- Coordinate care between different healthcare providers
- Manage symptoms like pruritus, fatigue, and nausea
- Provide nutritional counseling specific to liver conditions
- Conduct regular follow-up assessments
- Document progress and update care plans accordingly
Patient Education & Support
- Provide education about the specific cause of jaundice
- Teach self-monitoring techniques and warning signs
- Provide medication education and medication management
- Educate on dietary modifications for liver health
- Teach stress management techniques
- Provide emotional support and counseling
- Connect patients with support groups when appropriate
- Address misconceptions and cultural beliefs about jaundice
Collaborative & Advocacy Roles
| Collaborative Partner | Role of Community Health Nurse |
|---|---|
| Primary Care Providers |
|
| Specialists (Gastroenterologists, Hepatologists) |
|
| Nutritionists/Dietitians |
|
| Social Workers |
|
| Community Leaders |
|
Documentation and Reporting
Required Documentation
- Comprehensive assessment findings
- Care plans and interventions
- Patient response to interventions
- Education provided and comprehension level
- Referrals and follow-up plans
Surveillance Reporting
- Mandated reporting of certain causes of jaundice (e.g., acute viral hepatitis)
- Cluster identification and reporting
- Adverse events from treatments
- Community trends and patterns
Quality Improvement
- Track outcomes for jaundice management
- Identify system barriers to care
- Implement improvement strategies
- Participate in practice audits
Mnemonic: “JAUNDICE” for Community Health Nurse’s Role
- J – Judge severity and implement standing orders
- A – Assess comprehensively and regularly
- U – Understand underlying cause and appropriate management
- N – Nurture patient through education and support
- D – Document findings, interventions, and outcomes
- I – Initiate timely referrals when indicated
- C – Collaborate with other healthcare providers
- E – Educate for prevention and health promotion
Global Best Practices
Various regions worldwide have developed innovative approaches to managing jaundice in community settings. These practices offer valuable insights that can be adapted to different healthcare environments.
Thailand: Integrating Traditional Medicine
Thailand has successfully integrated traditional herbal remedies with modern medical management for adult jaundice in community settings.
Key Features:
- Evidence-based herbal supplements as adjuncts to conventional treatment
- Standard formulations for different causes of jaundice
- Integrated training for community health nurses
- Clear guidelines for when to use traditional vs. conventional approaches
- Reduced stigma and improved treatment adherence
*Only evidence-based traditional remedies with known safety profiles are included
Norway: Home Phototherapy Program
Norway has pioneered home-based phototherapy for neonatal jaundice, reducing hospital admissions and improving family-centered care.
Key Features:
- Portable phototherapy devices lent to families
- Daily home visits by community health nurses
- Telemedicine support from pediatricians
- Clear safety protocols and monitoring guidelines
- Improved breastfeeding rates and maternal satisfaction
- Cost-effective compared to hospital admission
India: Mobile Health Units for Jaundice
India has implemented mobile health units equipped to screen, diagnose, and provide initial management for jaundice in rural areas.
Key Features:
- Portable diagnostic equipment (bilirubin meters, ultrasound)
- Point-of-care testing for hepatitis
- Telemedicine linkage with specialists
- Community health nurse-led services
- Integration with regional referral system
- Health education component during village visits
South Africa: Jaundice Surveillance System
South Africa has developed an effective community-based surveillance system for jaundice to identify outbreaks and high-risk communities.
Key Features:
- Community health worker reporting network
- Mobile app for real-time data collection
- Geographic mapping of cases
- Early warning system for hepatitis outbreaks
- Targeted intervention deployment
- Integration with national health information system
Australia: Aboriginal Community Jaundice Program
Australia has developed culturally sensitive jaundice education and management programs for Aboriginal communities with high hepatitis B prevalence.
Key Features:
- Culturally appropriate educational materials
- Aboriginal health worker involvement in program design
- Integration of traditional healing practices
- Community-determined approach to screening
- Family-centered care model
- Long-term follow-up through community connections
Rwanda: SMS-Based Neonatal Jaundice Protocol
Rwanda has implemented an SMS-based system for managing neonatal jaundice in remote areas with limited access to healthcare facilities.
Key Features:
- Smartphone app for bilirubin estimation from skin/sclera photos
- Decision support algorithms for community health workers
- SMS notifications for follow-up visits
- Emergency transport coordination system
- Remote consultation with pediatricians
- Significant reduction in kernicterus cases
Implementation Considerations
| Best Practice | Adaptation Considerations | Resource Requirements |
|---|---|---|
| Home Phototherapy |
|
|
| Mobile Health Units |
|
|
| SMS-Based Systems |
|
|
Integration Strategy:
When adopting global best practices, consider implementing a phased approach:
- Conduct a community needs assessment specific to jaundice management
- Identify which best practices align with local needs and resources
- Adapt protocols to local context and healthcare system
- Pilot test the adapted approach in a limited area
- Evaluate effectiveness and make necessary adjustments
- Develop training materials for community health nurses
- Scale up successful interventions with continuous monitoring
References
- World Health Organization. (2022). Guidelines for the prevention, care and treatment of persons with chronic hepatitis B infection. WHO.
- American Academy of Pediatrics. (2022). Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics.
- National Institute for Health and Care Excellence. (2021). Jaundice in newborn babies under 28 days. NICE Guideline.
- Roy-Chowdhury N, Roy-Chowdhury J. (2021). Classification and causes of jaundice or asymptomatic hyperbilirubinemia. UpToDate.
- Sharma D, Farahbakhsh N, Sharma S, Sharma P, Sharma A. (2017). Role of home phototherapy in neonatal hyperbilirubinemia. Journal of Neonatal-Perinatal Medicine.
- World Health Organization. (2018). Guidelines for the care and treatment of persons diagnosed with chronic hepatitis C virus infection. WHO.
- Dennery PA, Seidman DS, Stevenson DK. (2001). Neonatal hyperbilirubinemia. New England Journal of Medicine.
- Gazzin S, Tiribelli C. (2015). Bilirubin-induced neurological damage. Journal of Maternofetal & Neonatal Medicine.
- Ministry of Health Singapore. (2022). Nursing management of adult patients with jaundice: Clinical practice guidelines. MOH Singapore.
- International Council of Nurses. (2020). Community health nursing practice guidelines. ICN.
